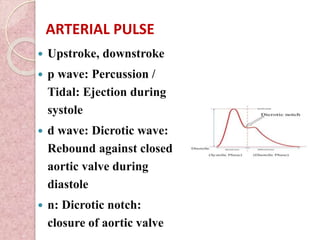
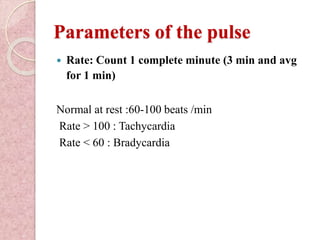
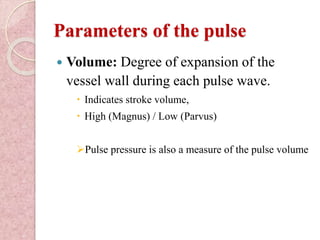
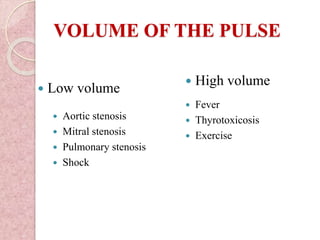
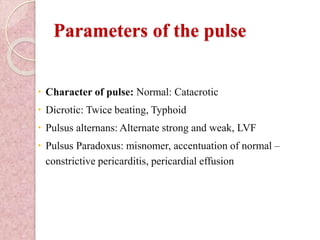
The arterial pulse is caused by the transmission of pressure waves along the arteries during ventricular systole. The pulse can be felt over arteries and provides information about heart rate, rhythm, and volume. The jugular venous pulse reflects right atrial pressure and is assessed by observing waves corresponding to atrial contraction and filling. Together, examining the arterial and jugular pulses provides clinical information about cardiovascular function and hemodynamics.