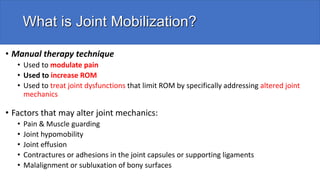
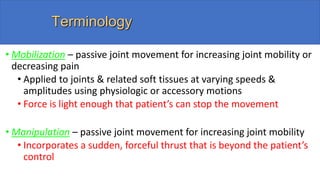
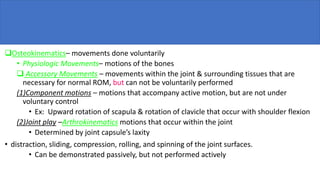
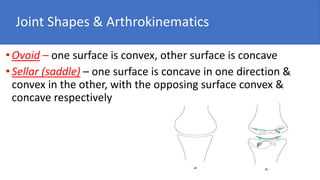
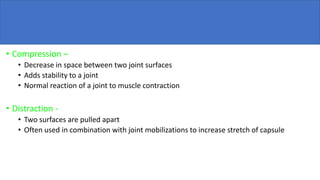
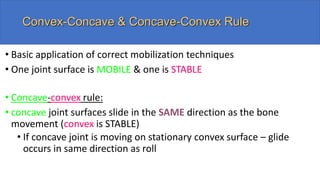
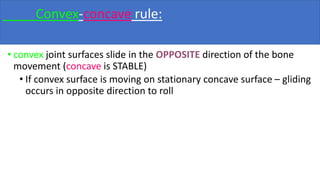
Joint mobilization is a manual therapy technique used to modulate pain, increase range of motion, and treat joint dysfunctions. It involves passive movement of joints and surrounding soft tissues at varying speeds and amplitudes. There are 5 types of joint movement - roll, slide, spin, compression, and distraction. Mobilization techniques are graded based on amplitude and location within the range of motion. Lower grades are used for pain modulation while higher grades aim to increase mobility. Proper positioning, stabilization, direction, and patient response are important considerations when applying mobilization.