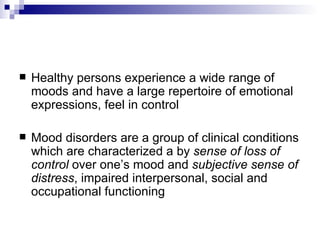
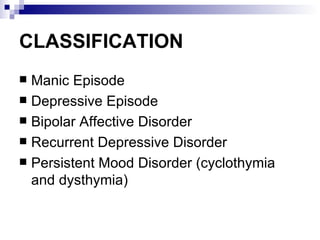
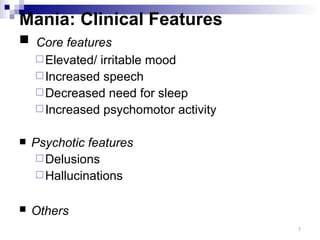
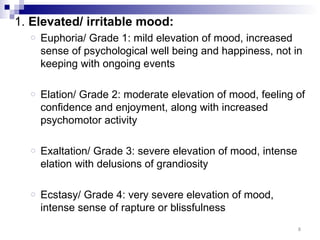
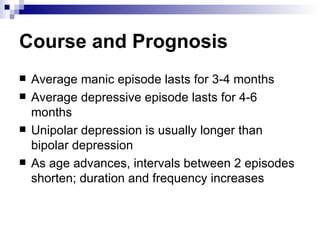
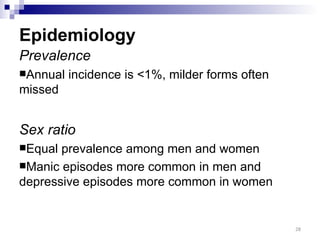
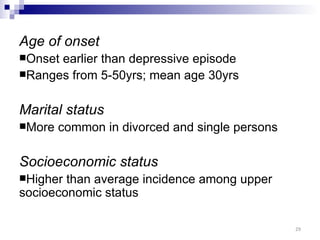
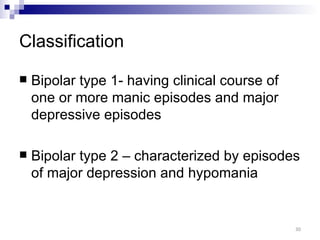
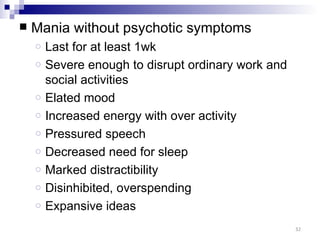
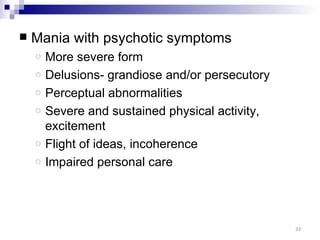
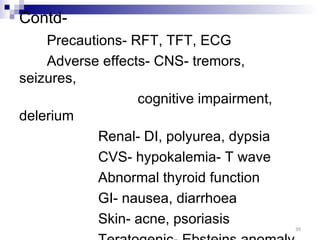
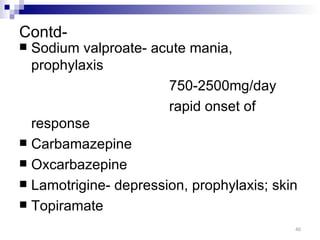
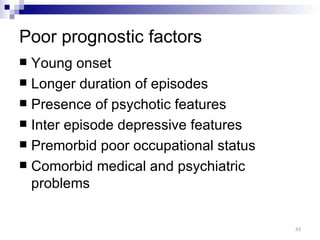
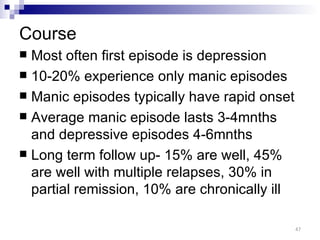
Mood disorders are characterized by a sense of loss of control over one's mood and subjective distress. They include conditions like bipolar disorder and recurrent depressive disorder. Bipolar disorder involves alternating periods of mania and depression, while recurrent depressive disorder involves two or more episodes of major depression. Core features of mania include elevated or irritable mood, increased speech, decreased need for sleep, and increased psychomotor activity, while depression is marked by depressed mood, anhedonia, and loss of energy. Treatment involves mood stabilizers, antipsychotics, benzodiazepines, antidepressants, or electroconvulsive therapy. Prognosis depends on factors like age of onset, duration of episodes, and presence of psych