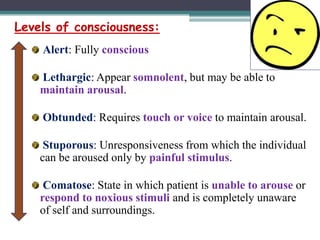
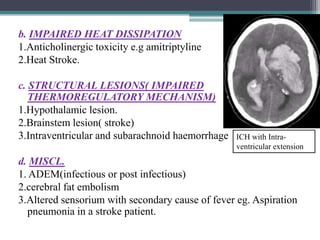
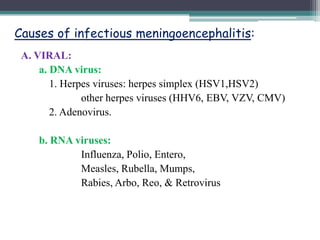
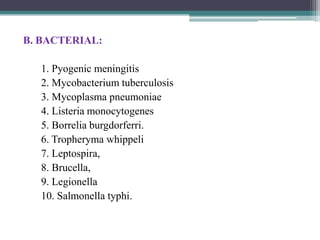
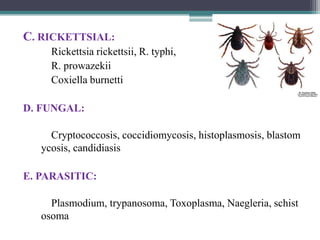
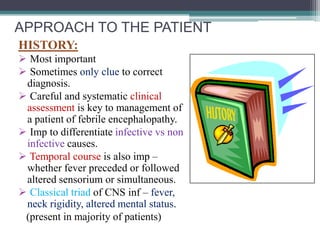
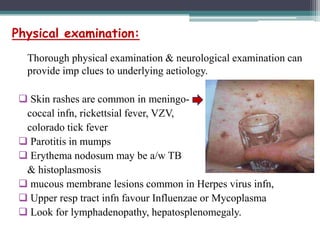
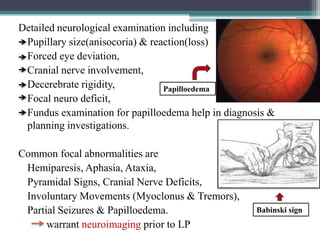
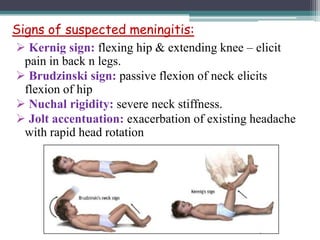
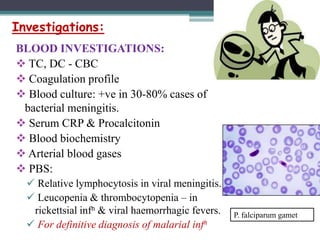
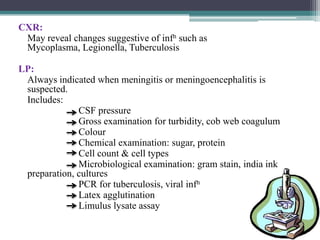
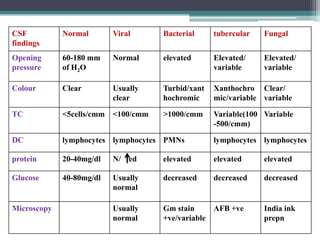
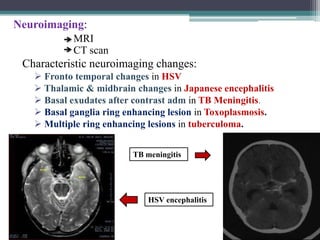
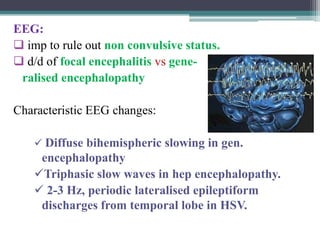
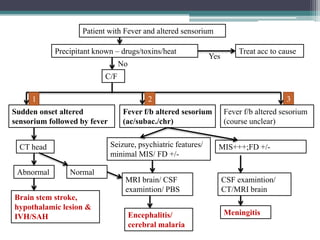
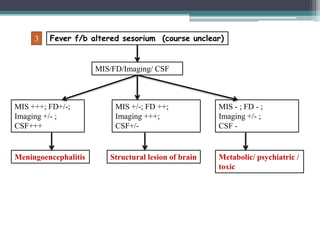
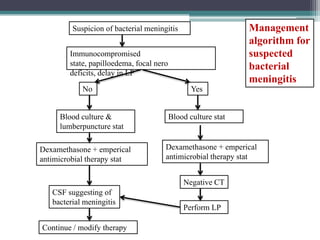
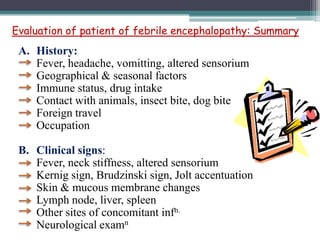
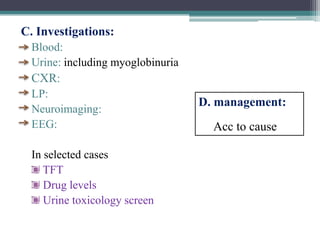
The document discusses the medical emergency of fever with altered sensorium, emphasizing the importance of early recognition and treatment. It outlines various causes including infectious (e.g., encephalitis, meningitis) and non-infectious (e.g., neuroleptic malignant syndrome, heat stroke) origins, along with diagnostic approaches and treatment strategies. Key points include careful patient history, thorough physical examination, and tailored investigations to differentiate between potential etiologies.