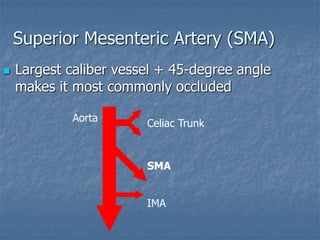
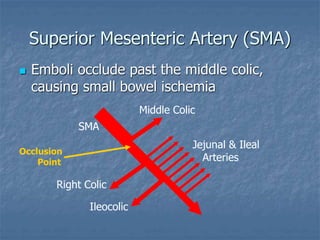
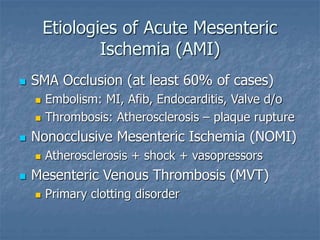
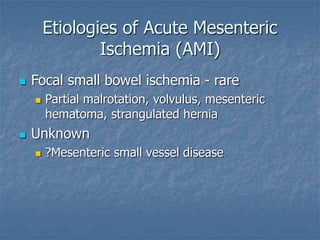
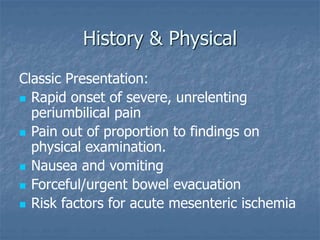
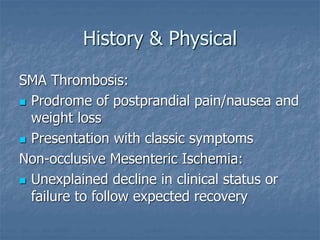
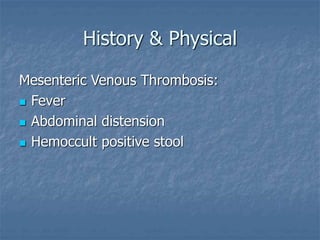
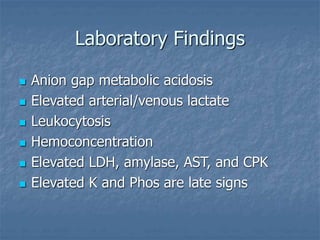
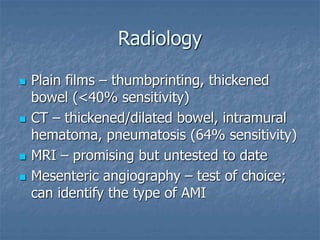
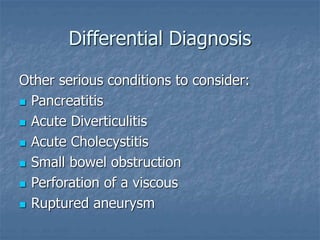
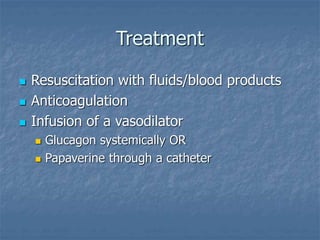
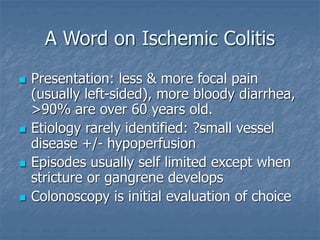
This document discusses acute mesenteric ischemia and infarction. It begins by distinguishing mesenteric ischemia, which involves the small bowel, from ischemic colitis, which involves the colon. It then describes the etiologies of acute mesenteric ischemia, particularly superior mesenteric artery occlusion, embolism, thrombosis, nonocclusive mesenteric ischemia, and mesenteric venous thrombosis. The document outlines the classic presentation, laboratory findings, diagnostic imaging, differential diagnosis, and treatment approaches for acute mesenteric ischemia and infarction.