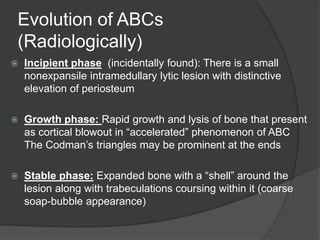
Aneurysmal bone cysts are non-neoplastic, blood-filled lesions of bone that typically affect people under 30 years old. They most commonly occur in the proximal humerus, distal femur, proximal tibia, and spine. On imaging, they appear as an expansile, osteolytic lesion with thinning of the bone cortex. Treatment depends on the activity of the lesion and can include percutaneous sclerotherapy, curettage with bone grafting, or en bloc resection. Curettage with adjuvants has traditionally been the standard treatment but has risks of recurrence or growth plate damage.