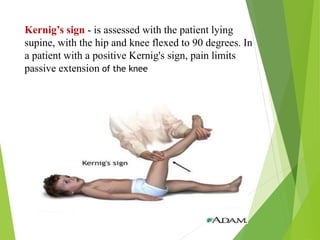
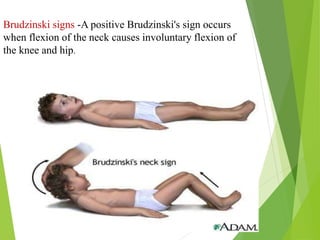
The document discusses meningitis, which is an inflammation of the meninges - the protective membranes surrounding the brain and spinal cord. It has three layers: the dura mater, arachnoid mater, and pia mater. Meningitis can be caused by bacteria, viruses, fungi or parasites. Common types are bacterial, viral and tuberculous meningitis. Symptoms vary with age but may include fever, headache, stiff neck, vomiting, and altered consciousness. Diagnosis involves examining cerebrospinal fluid obtained via lumbar puncture. Treatment involves antibiotics, anticonvulsants, and supportive care like maintaining fluid and nutrition. Complications can include brain damage if not treated promptly.