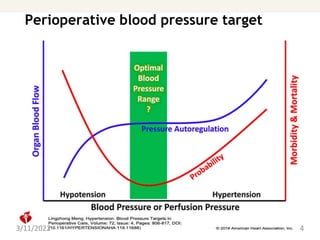
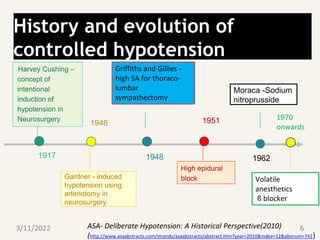
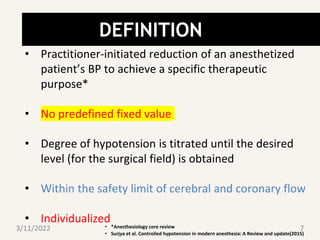
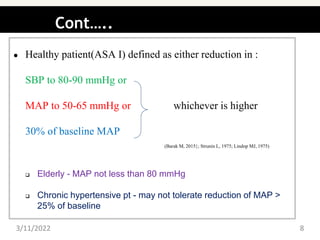
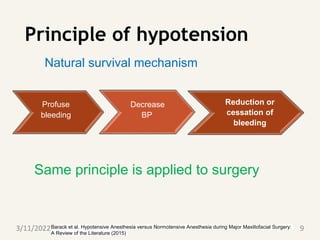
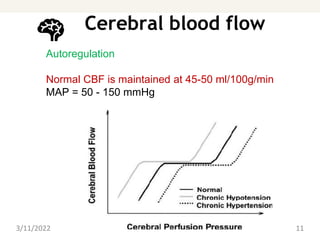
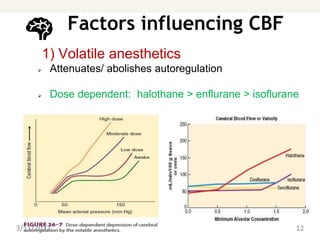
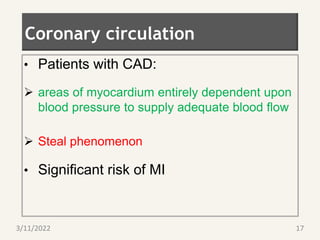
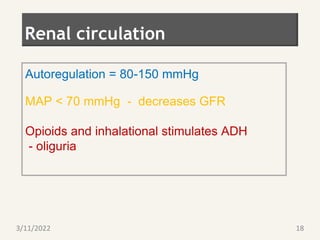
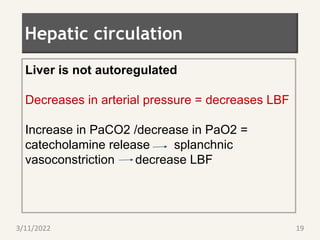
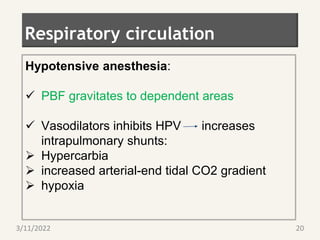
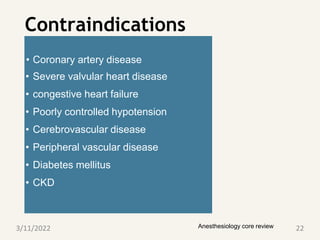
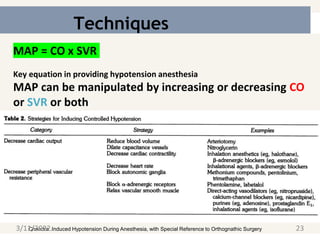
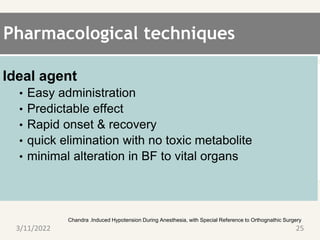
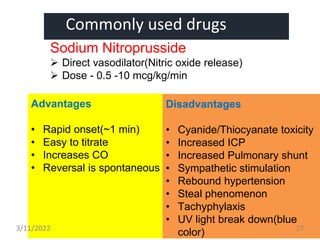
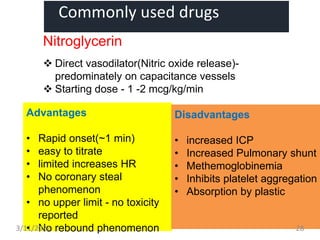
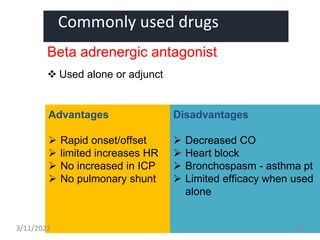
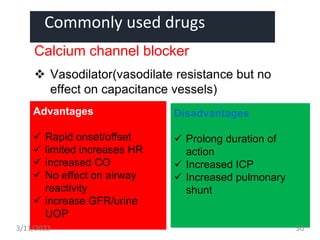
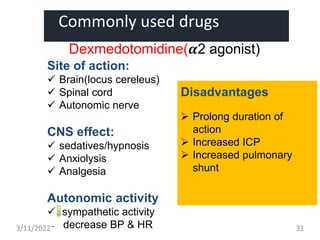
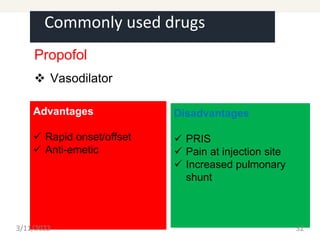
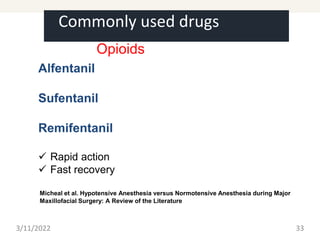
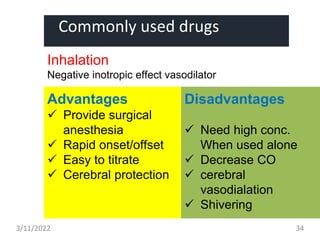
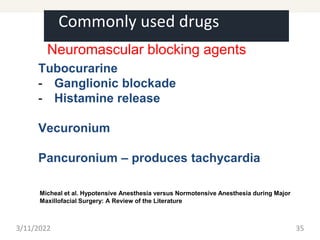
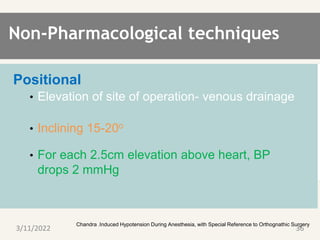
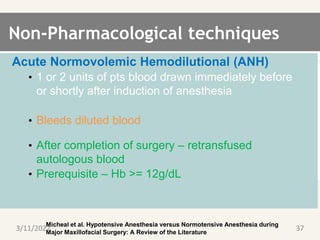
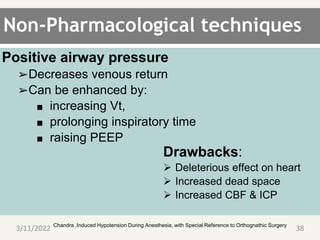
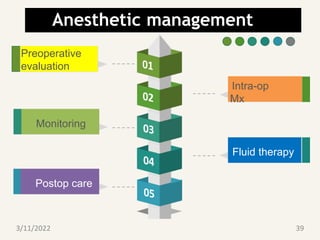
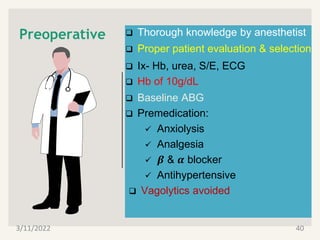
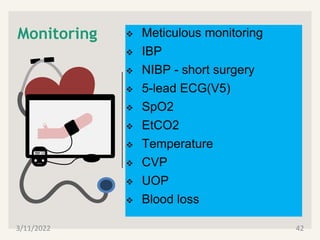
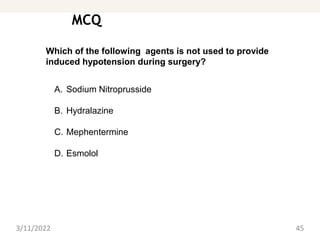
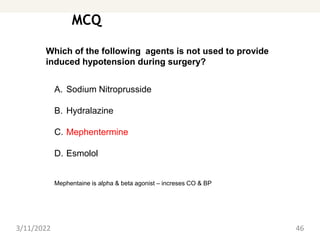
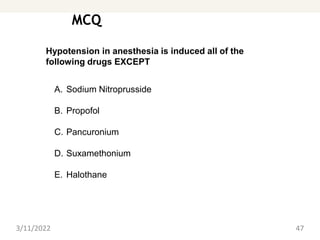
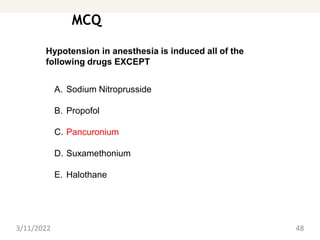
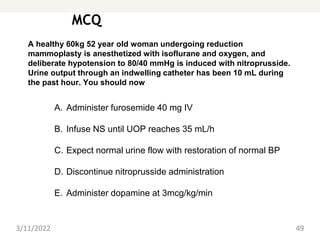
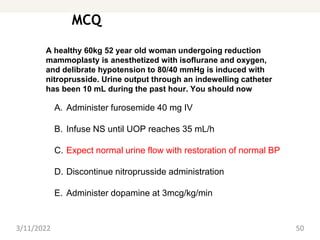
This document provides an outline and overview of controlled hypotension during anesthesia. It begins with definitions and a brief history of controlled hypotension. It then discusses the principles and techniques of inducing hypotension, including pharmacological agents like sodium nitroprusside, nitroglycerin, beta blockers, and calcium channel blockers. It also covers non-pharmacological techniques like positioning and acute normovolemic hemodilution. Monitoring, fluid management, and postoperative care are also outlined. The document concludes with sample multiple choice questions related to controlled hypotension.