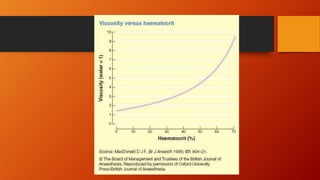
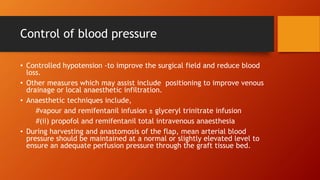
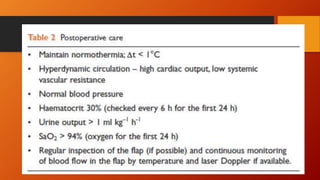
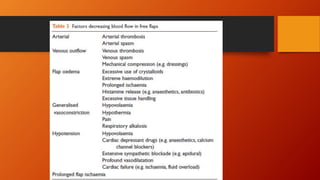
This document discusses anaesthesia considerations for reconstructive free flap surgery. It involves the transfer of free tissue (skin, muscle, bone, etc.) to repair large wounds via microvascular anastomoses. The stages include flap elevation, primary ischemia during transfer, and reperfusion via new blood vessels. Maintaining adequate blood flow and oxygen delivery to the flap is crucial. The anaesthetic aims to provide a hyperdynamic circulation through fluid administration, vasodilation, and temperature control in order to maximize microcirculatory perfusion and minimize secondary ischemia of the transplanted tissue.