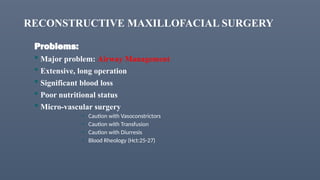
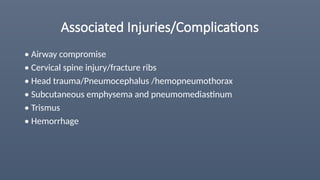
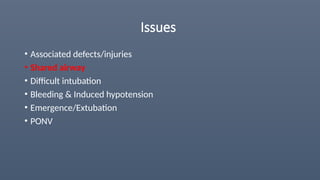
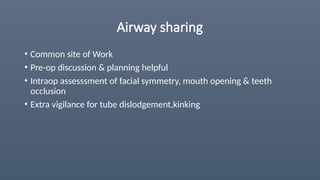
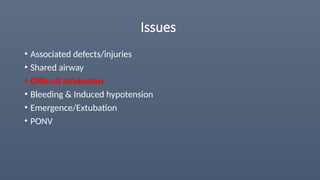
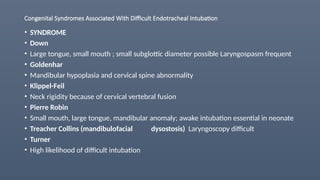
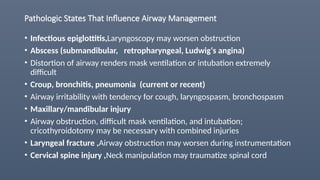
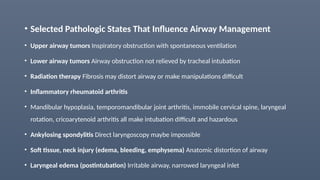
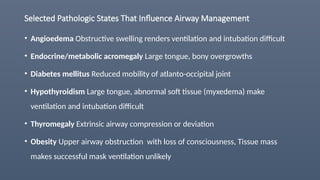
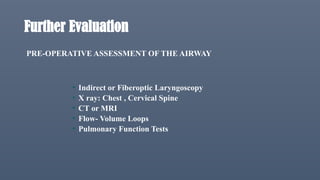
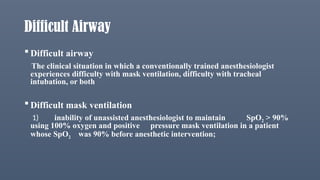
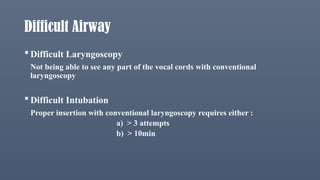
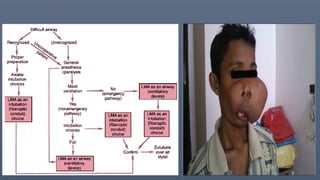
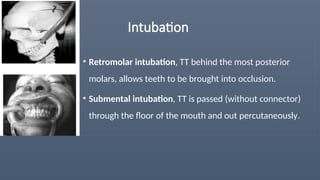
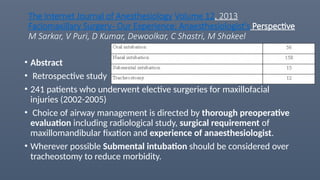
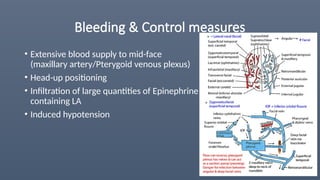
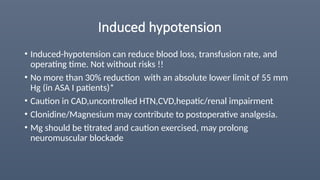
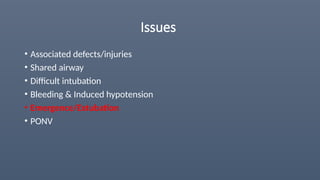
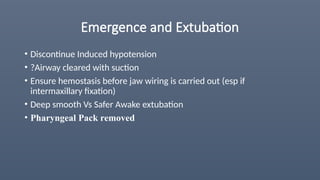
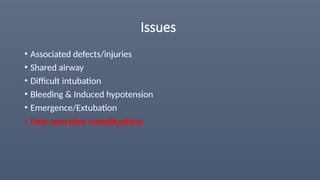
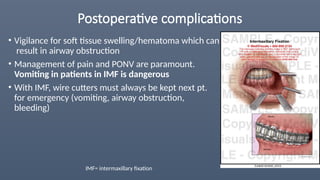
The document discusses anesthetic implications and management strategies for maxillofacial surgery, highlighting the importance of pre-operative evaluation and the challenges posed by associated injuries and conditions affecting airway management. Key issues include the need for careful monitoring of hemodynamic changes during surgery, management of difficult intubation scenarios, and post-operative care to prevent complications such as airway obstruction and vomiting. The use of hypotensive anesthesia is emphasized for reducing intra-operative bleeding, but careful patient selection and monitoring are crucial due to potential risks.