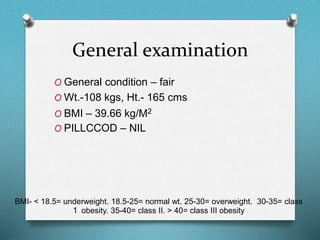
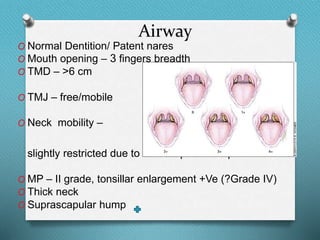
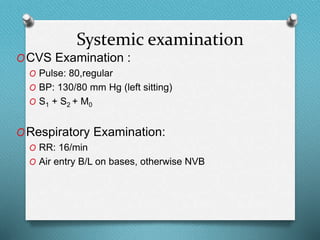
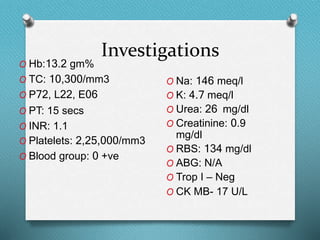
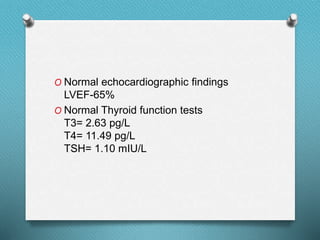
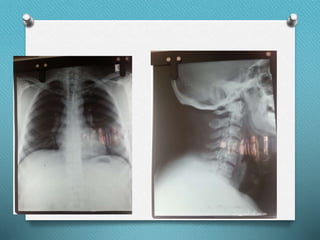
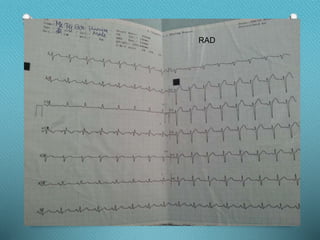
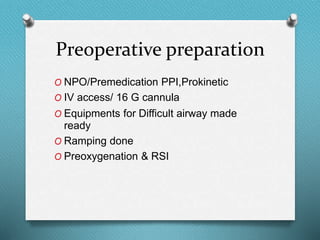
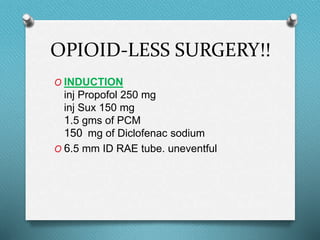
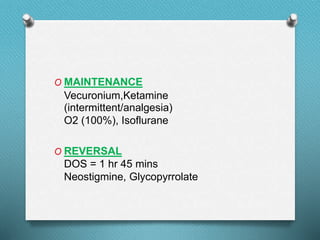
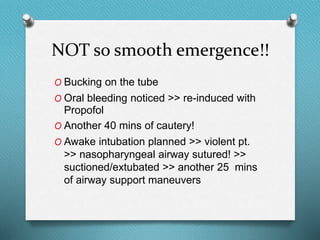
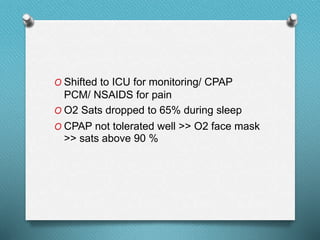
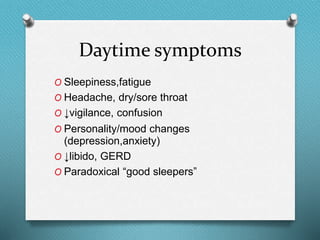
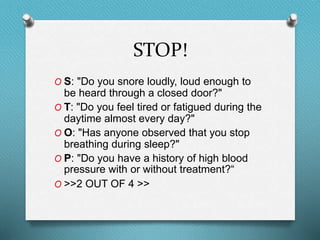
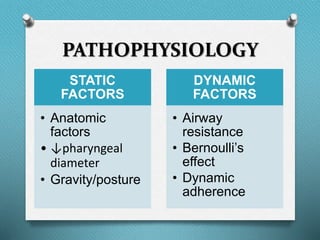
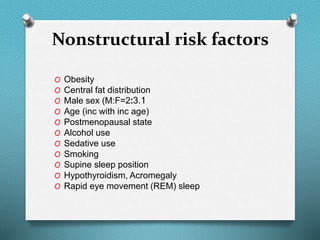
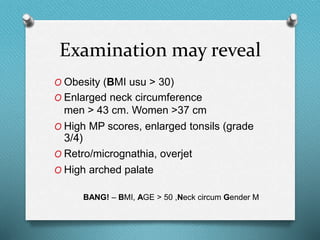
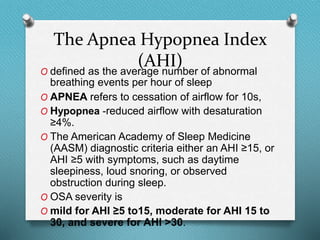
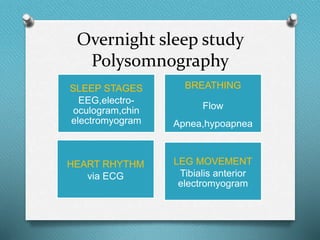
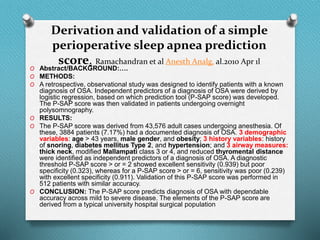
This document summarizes a patient visit and evaluation for obstructive sleep apnea. The 32-year-old male patient presented with snoring, throat pain, and disturbed sleep. Examination found obesity, enlarged tonsils, and other risk factors. Polysomnography was not performed but the patient's symptoms and characteristics were consistent with severe obstructive sleep apnea. The patient underwent uvulopalatopharyngoplasty surgery, which had complications requiring extended operating time. Post-operatively, the patient required oxygen and CPAP support. Risk factors, diagnosis, treatment options and postoperative care for obstructive sleep apnea were discussed.