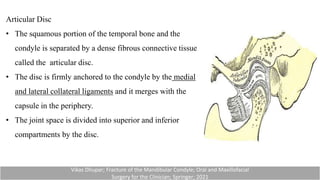
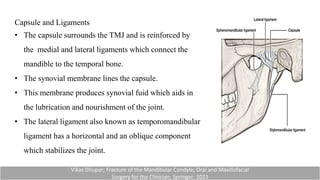
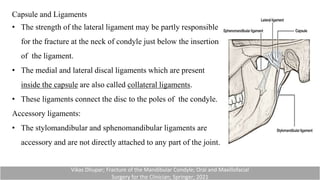
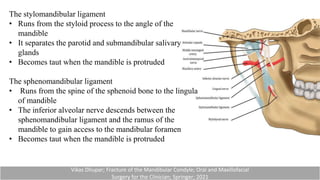
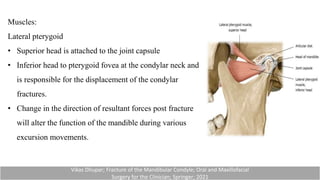
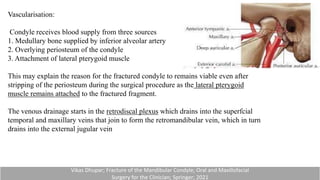
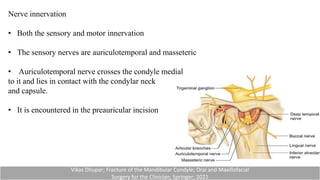
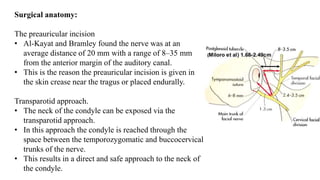
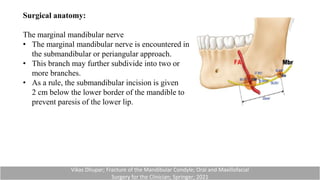
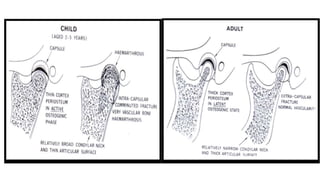
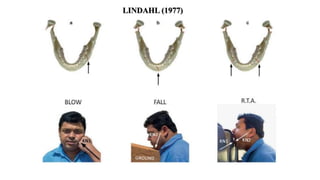
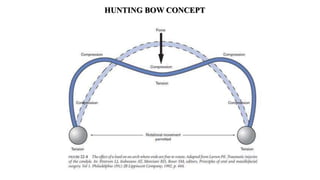
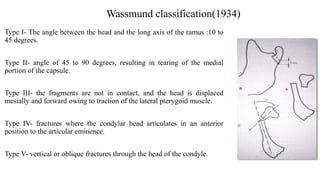
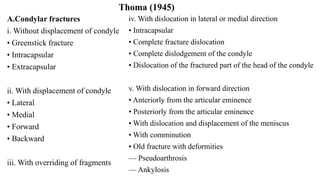
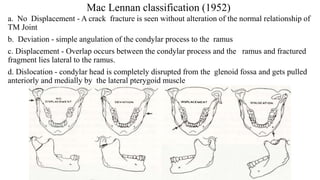
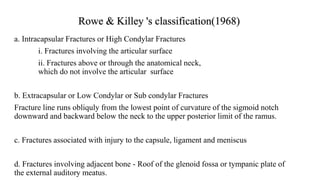
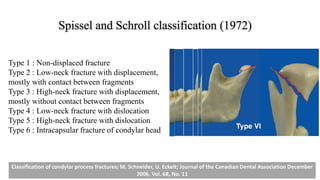
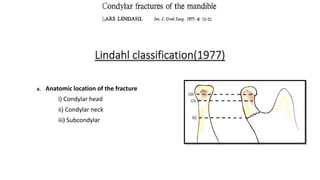
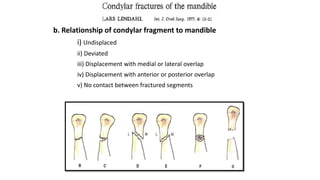
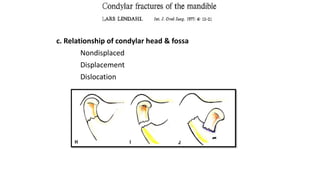
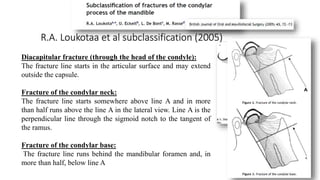
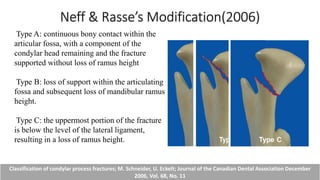
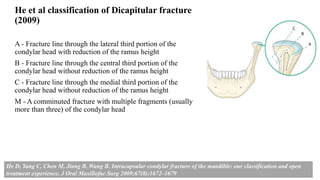
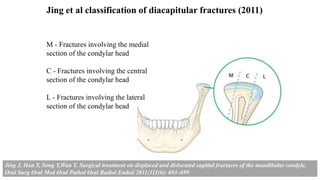
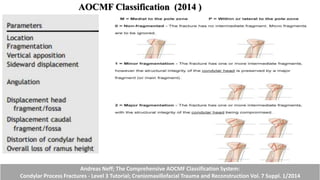
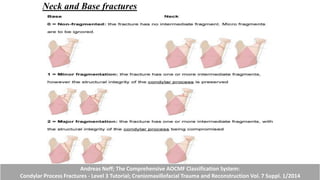
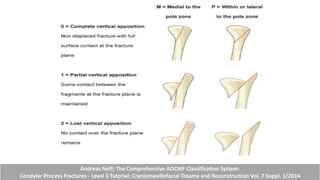
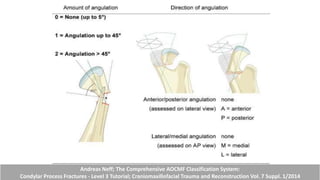
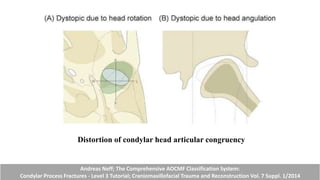
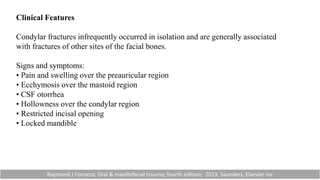
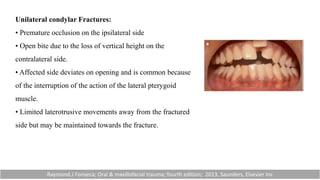
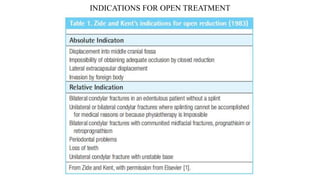
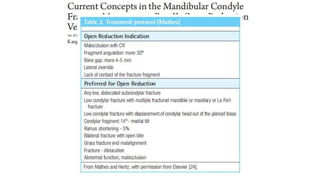
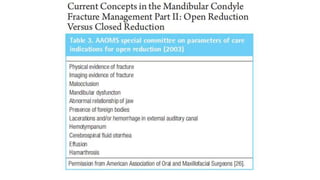
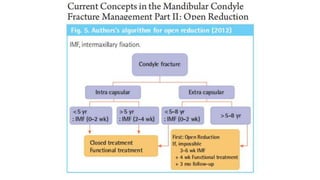
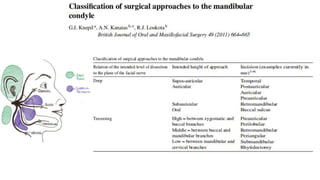
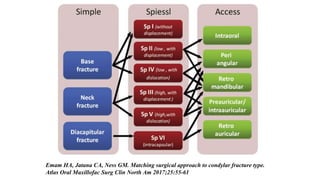
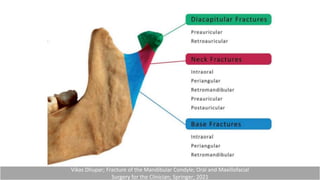
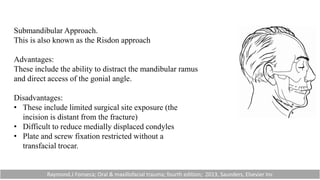
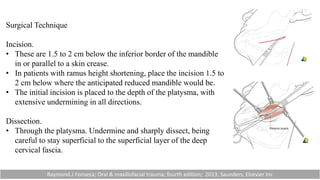
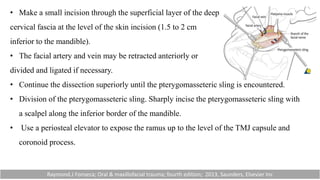
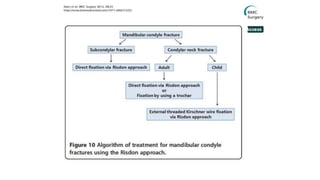
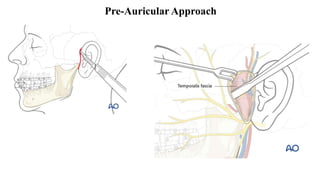
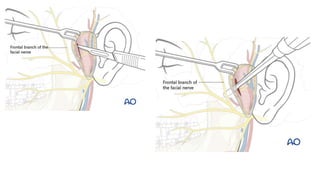
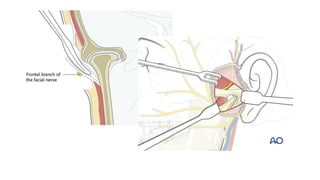
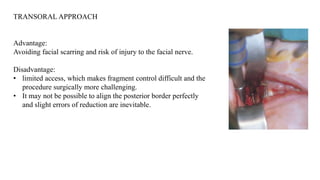
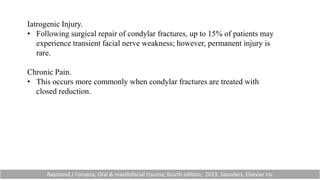
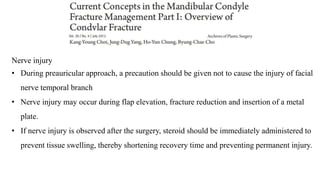
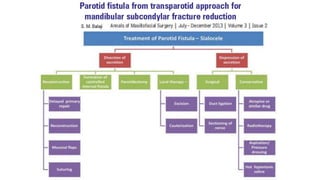
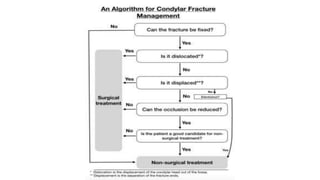
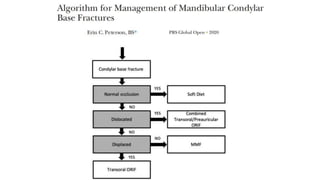
This document provides information on condylar fractures of the mandible. It begins with an introduction stating that condylar fractures account for 17.5-52% of mandibular fractures and can cause functional issues with occlusion, mastication and speech. It then covers the surgical anatomy of the temporomandibular joint and condyle, including the articular disc, capsule, ligaments, muscles, vascularization and nerve innervation. Various classification systems for condylar fractures are also described. The document emphasizes that the unique functional anatomy and challenges of surgery of these fractures can lead to various patient outcomes.