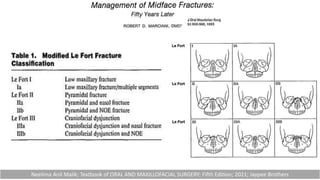
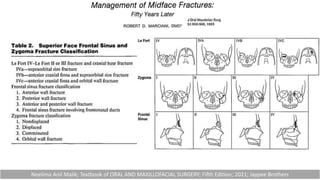
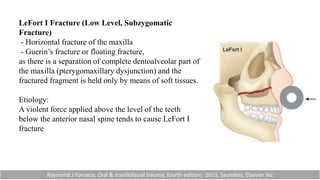
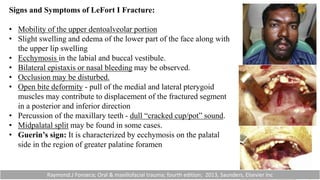
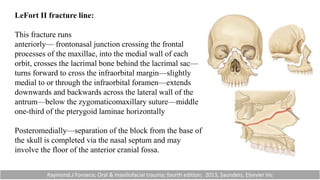
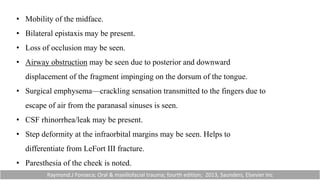
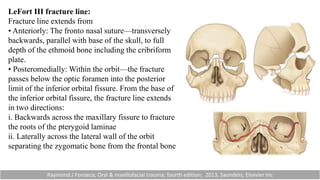
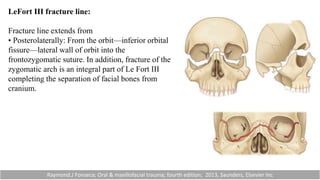
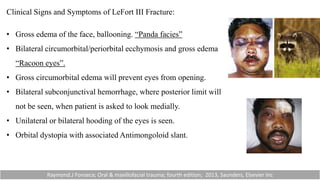
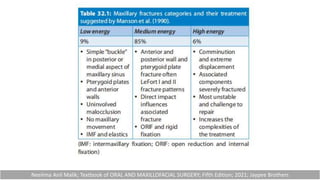
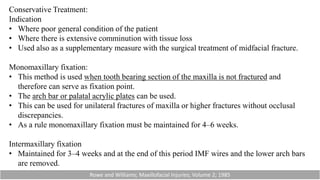
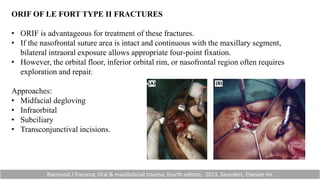
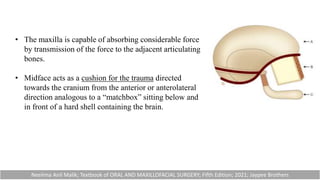
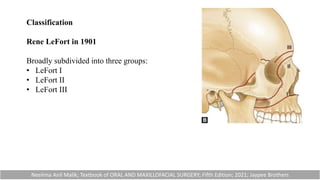
This document discusses midface fractures, known as LeFort fractures. It begins by defining the midface region and describing the bones that make up the midface. It then discusses the classic classifications of LeFort fractures as proposed by LeFort himself and others. Specifically, it describes LeFort I, II, and III fractures in terms of their etiology, fracture lines, and clinical signs. Radiographic examination including waters view and CT are important for diagnosis. Pre-operative planning considers the type of fixation and stabilization needed. Management involves open reduction with plates, screws or wires as well as intermaxillary fixation devices.





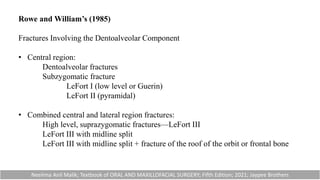
![Rowe and William’s (1985)
Fractures not Involving the Dentoalveolar Component
• Central region:
Fractures of the nasal bones and/or nasal septum.
Lateral nasal injuries
Anterior nasal injuries
Fractures of the frontal process of the maxilla.
Fractures of nasoethmoid
Fractures of Fronto-orbito-nasal
• Lateral region:
Fractures involving the zygomatic bone, arch and maxilla [zygomaticomaxillary
complex (ZMC)] excluding the dentoalveolar component.
Rowe and Williams; Maxillofacial Injuries; Volume 2; 1985](https://image.slidesharecdn.com/midfacefracture-231004082652-0e6fa722/85/Midface-fracture-pptx-9-320.jpg)