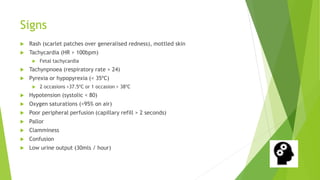
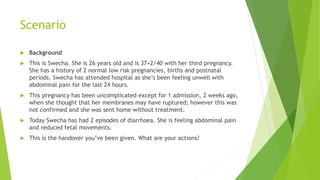
The document outlines the recognition and management of sepsis as an obstetric emergency, emphasizing the critical need for early intervention, including IV antibiotics and fluid resuscitation. Signs and symptoms of sepsis are detailed along with risk factors and the importance of a multi-disciplinary team in management. Additionally, the document introduces a specific case scenario, urging immediate action and adherence to protocols like the 'sepsis six' within the first hour of presentation.