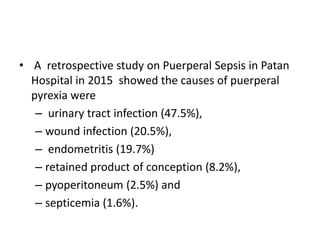
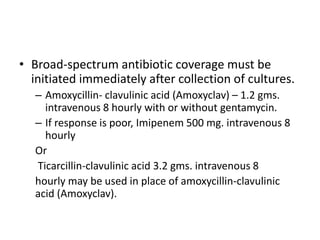
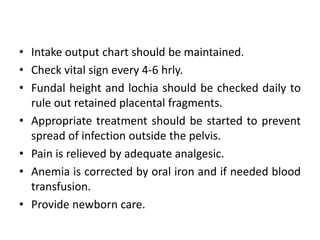
Puerperal sepsis is a major cause of maternal mortality, accounting for 15% of maternal deaths worldwide, typically occurring within 42 days postpartum due to infections in the genital tract. It can arise from both endogenous and exogenous bacteria, with common risk factors including malnutrition, traumatic deliveries, and poor hygiene practices. Effective prevention and treatment strategies include adequate antenatal care, timely treatment of complications, and the use of broad-spectrum antibiotics in severe cases.







































![References
• Arulkumaran, N., & Singer, M. (2013). Puerperal sepsis.
Best Practice and Research: Clinical Obstetrics and
Gynaecology, 27(6), 893–902.
https://doi.org/10.1016/j.bpobgyn.2013.07.004
• Buddeberg, B. S., & Aveling, W. (2015). Puerperal sepsis
in the 21st century: Progress, new challenges and
the situation worldwide. Postgraduate Medical
Journal, 91(1080), 572–578.
https://doi.org/10.1136/postgradmedj-2015-133475
• World Health Organization [WHO]. (2008). Education
material for teachers of midwifery Midwifery education
modules-second edition.](https://image.slidesharecdn.com/puperialsepsis-210331151548/85/Puperial-sepsis-64-320.jpg)