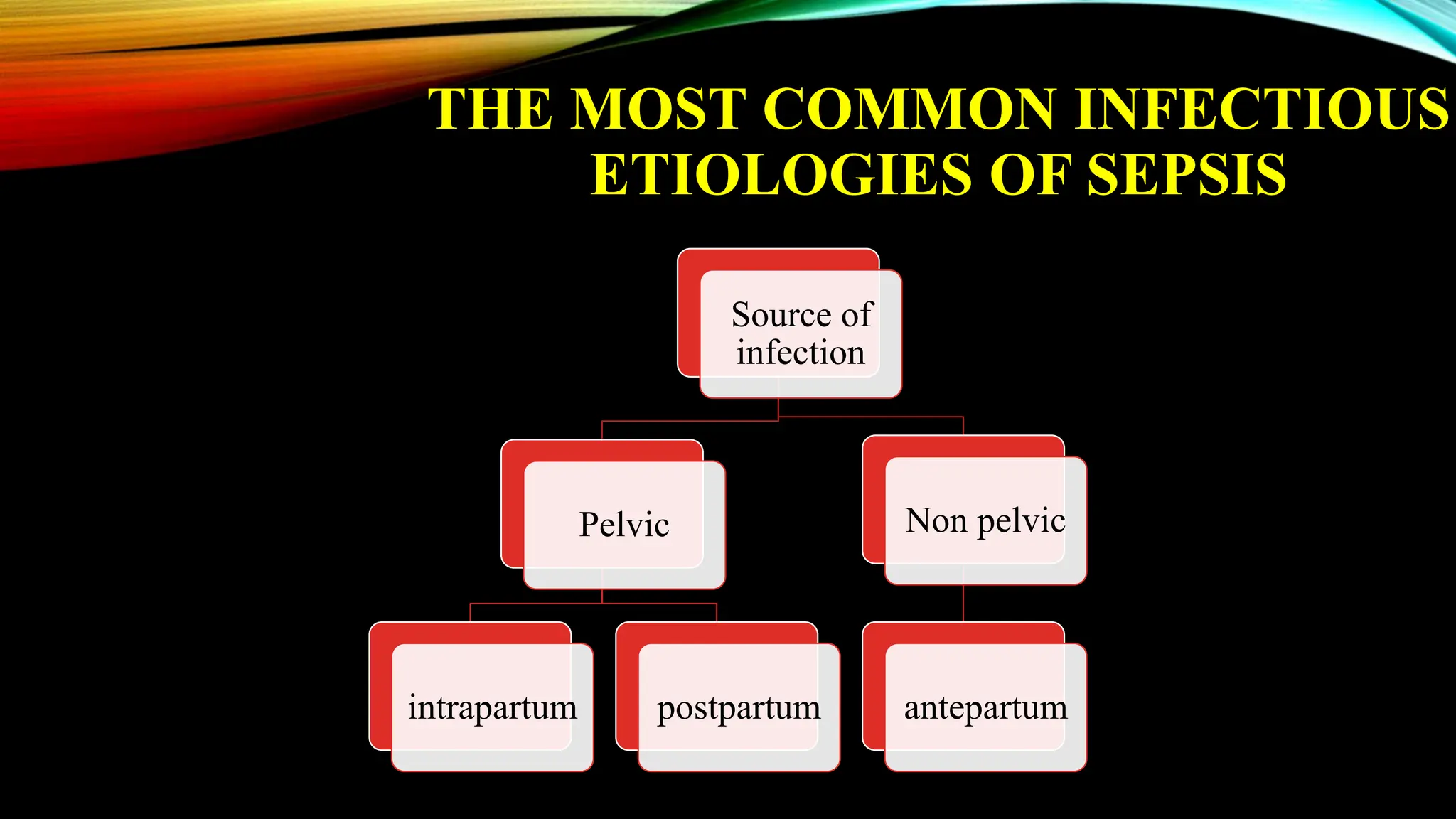
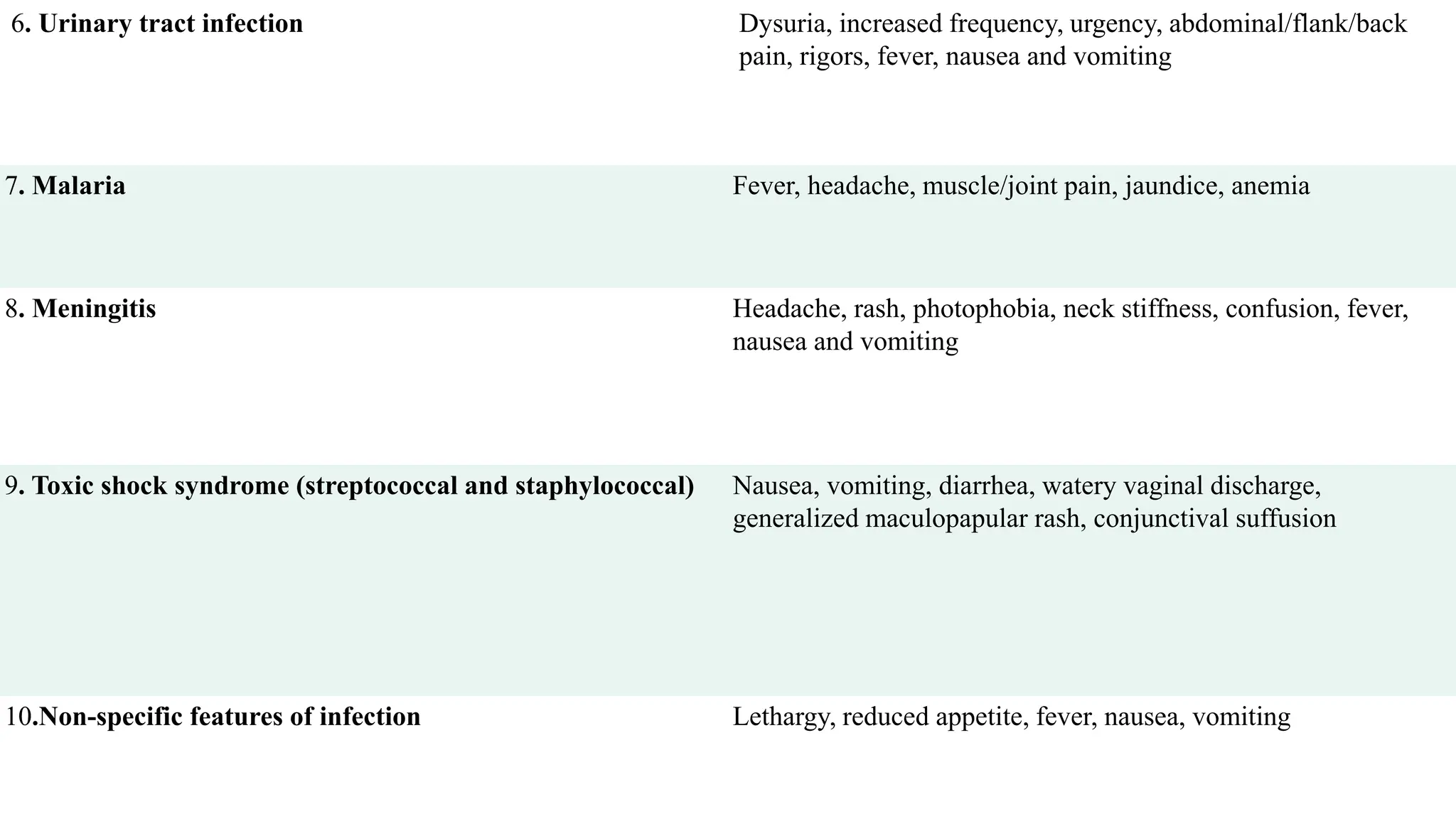
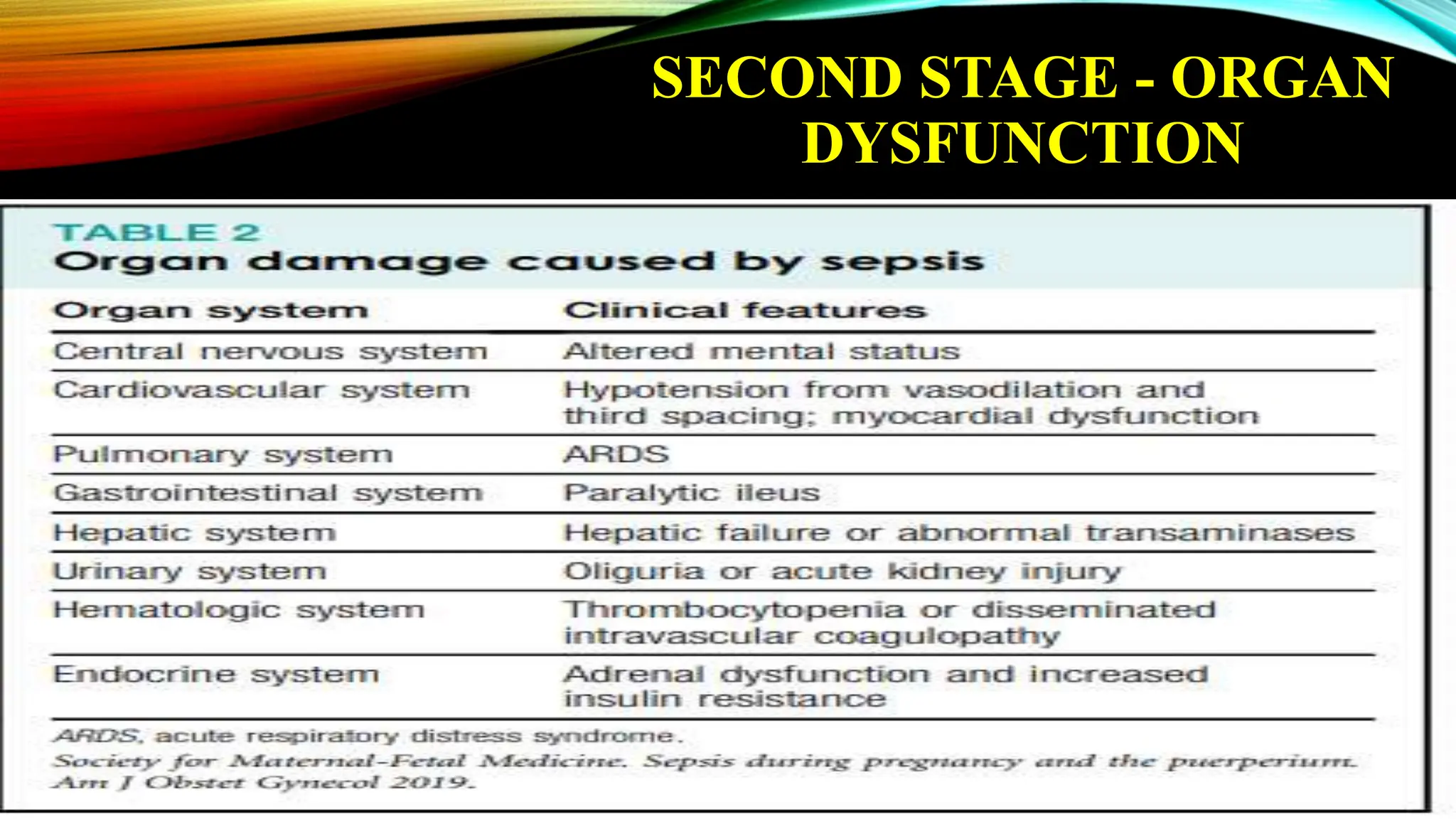
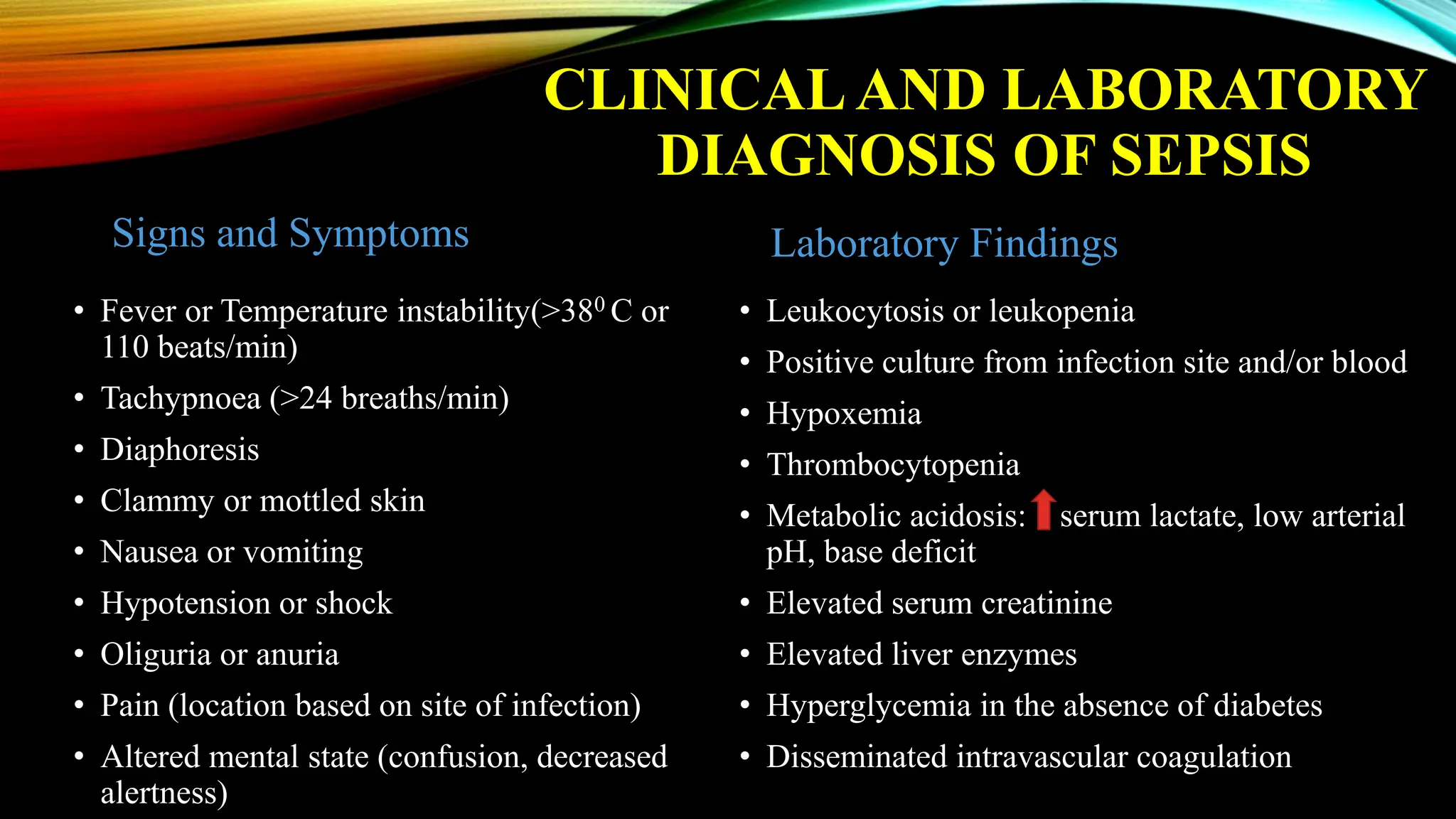
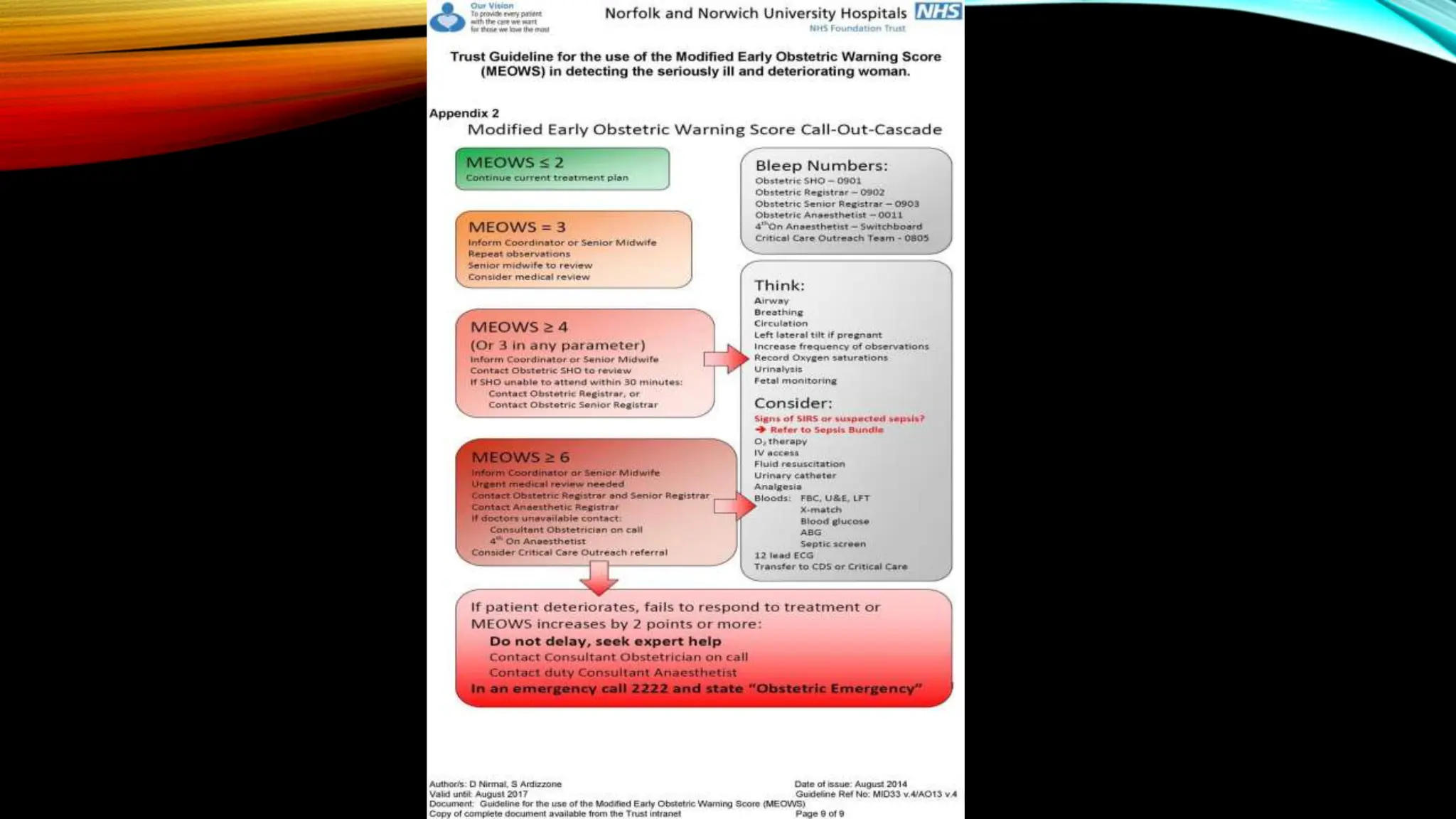
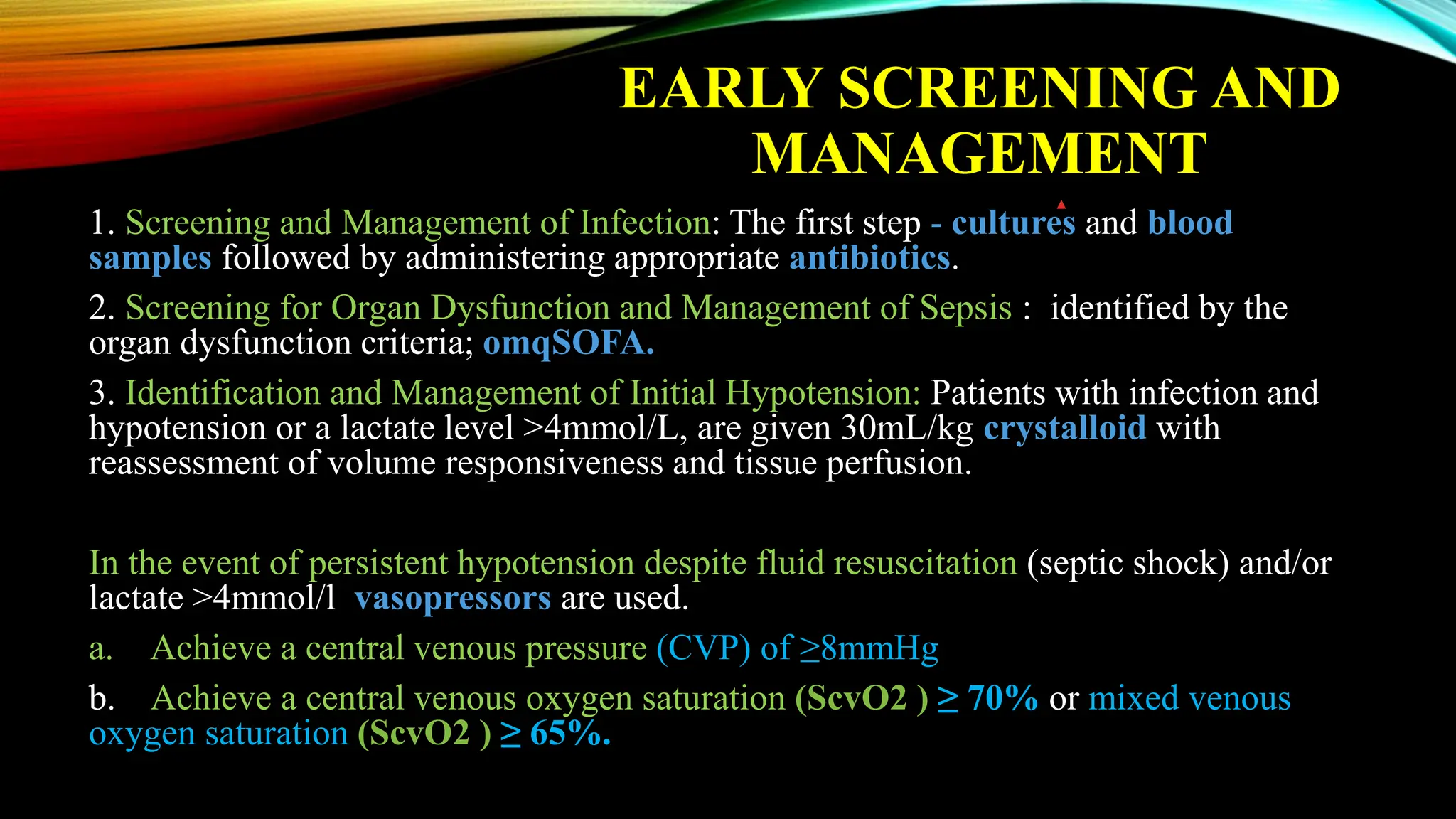
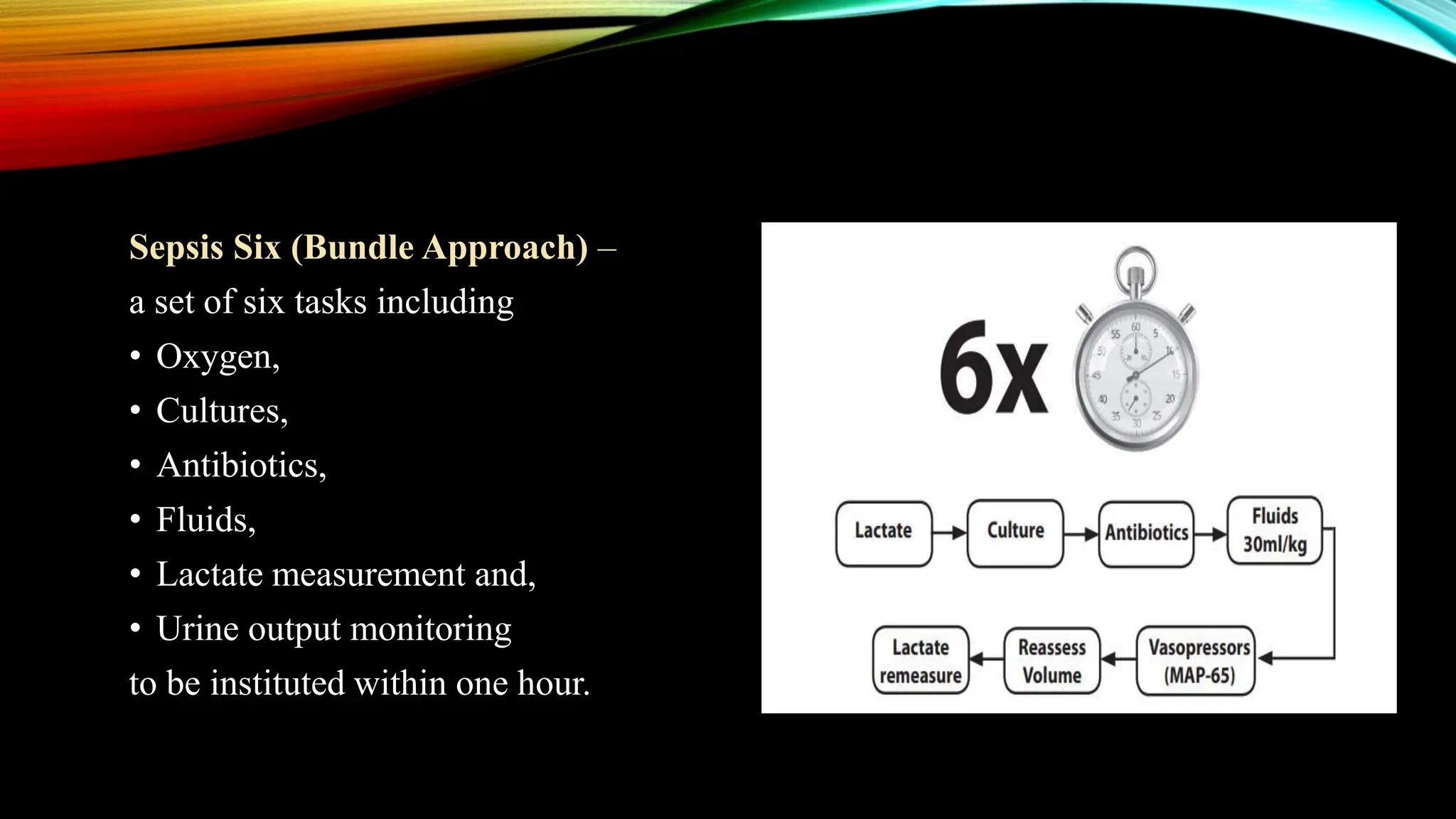
The document details the issues of maternal sepsis, its causes, risk factors, clinical diagnosis, management strategies, and case studies presented at the 9th Annual Conference of the Andhra Pradesh Obstetrics & Gynaecological Society. It emphasizes the importance of timely identification and management of sepsis in obstetric patients to prevent high maternal mortality rates associated with the condition. Additionally, it discusses recommended practices and guidelines for managing obstetric sepsis to improve outcomes for mothers and neonates.