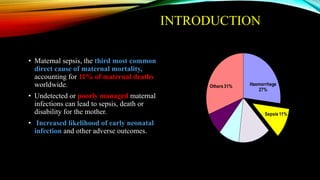
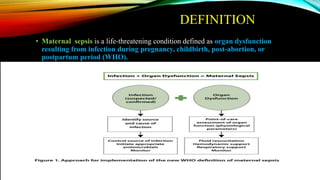
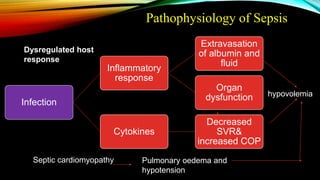
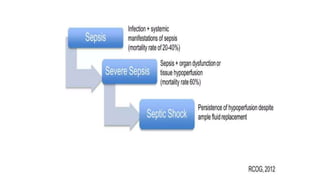
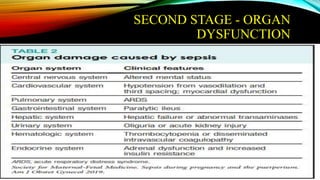
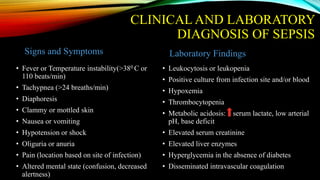
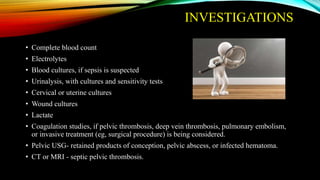
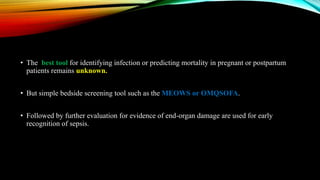
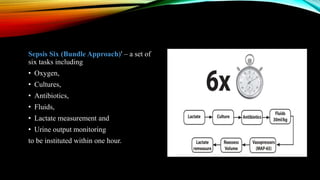
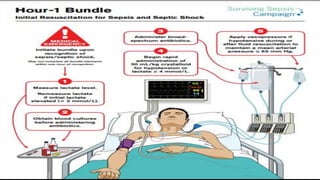
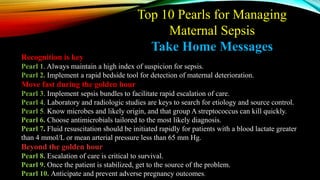
Dr. Niranjan Chavan presented on an obstetrics sepsis bundle approach. Maternal sepsis is a leading cause of maternal mortality worldwide. Early screening and treatment is key to managing sepsis. The sepsis bundle approach involves completing 6 tasks within 1 hour of diagnosis: administering oxygen, collecting cultures, giving antibiotics, fluid resuscitation, measuring lactate levels, and monitoring urine output. Additional treatment may include source control, vasopressors, corticosteroids, DVT prophylaxis, and determining whether delivery is necessary based on maternal and fetal status. With rapid identification and treatment, the sepsis bundle approach can help reduce mortality from this life-threatening condition.