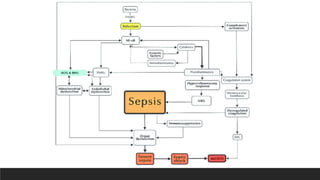
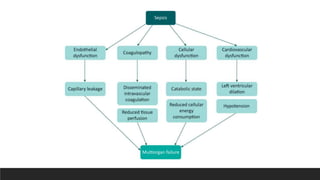
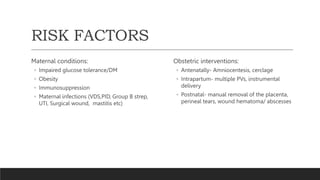
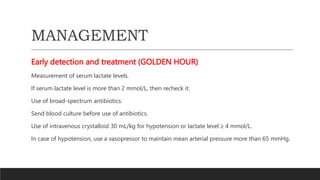
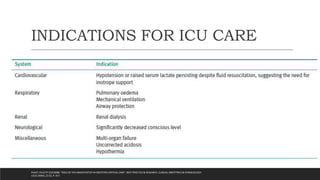
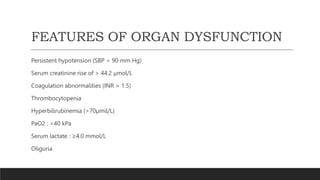
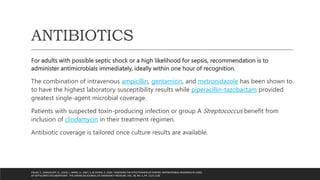
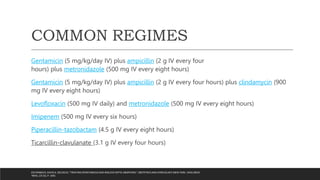
Sepsis and septic shock are life-threatening medical emergencies in obstetric patients that require immediate treatment and resuscitation. Risk factors include underlying maternal conditions and obstetric interventions. Early detection and treatment within an hour is critical and involves administering IV fluids and broad-spectrum antibiotics while measuring lactate levels and stabilizing vital signs. Complications can include hemorrhage, endotoxic shock, acute renal failure, and ARDS. Prevention focuses on optimizing family planning, enforcing safe abortion practices, and administering prophylactic antibiotics in certain high-risk situations.