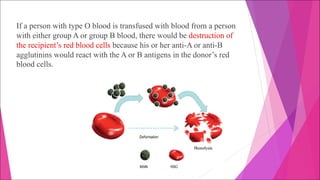
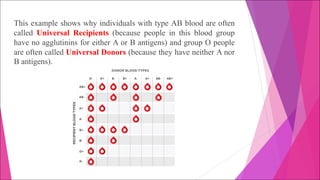
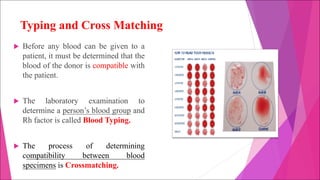
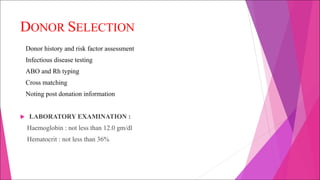
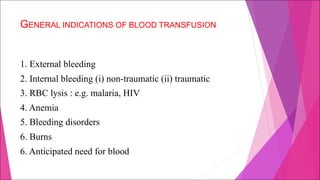
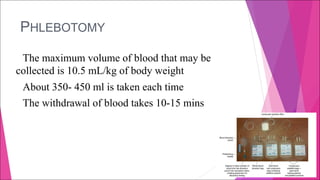
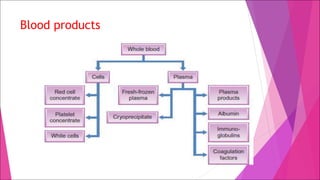
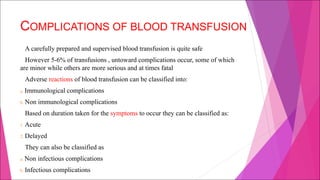
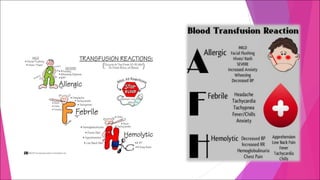
A blood transfusion involves infusing whole blood or blood components into a patient's circulation to treat red blood cell loss or inadequate blood cell production. Blood typing and cross-matching must be performed to match the donor's blood group antigens with the recipient's antibodies to avoid transfusion reactions. Complications can include allergic reactions, circulatory overload, lung injury, and infections if the donor blood is contaminated. Proper donor screening and use of blood products help ensure safe and effective blood transfusions.