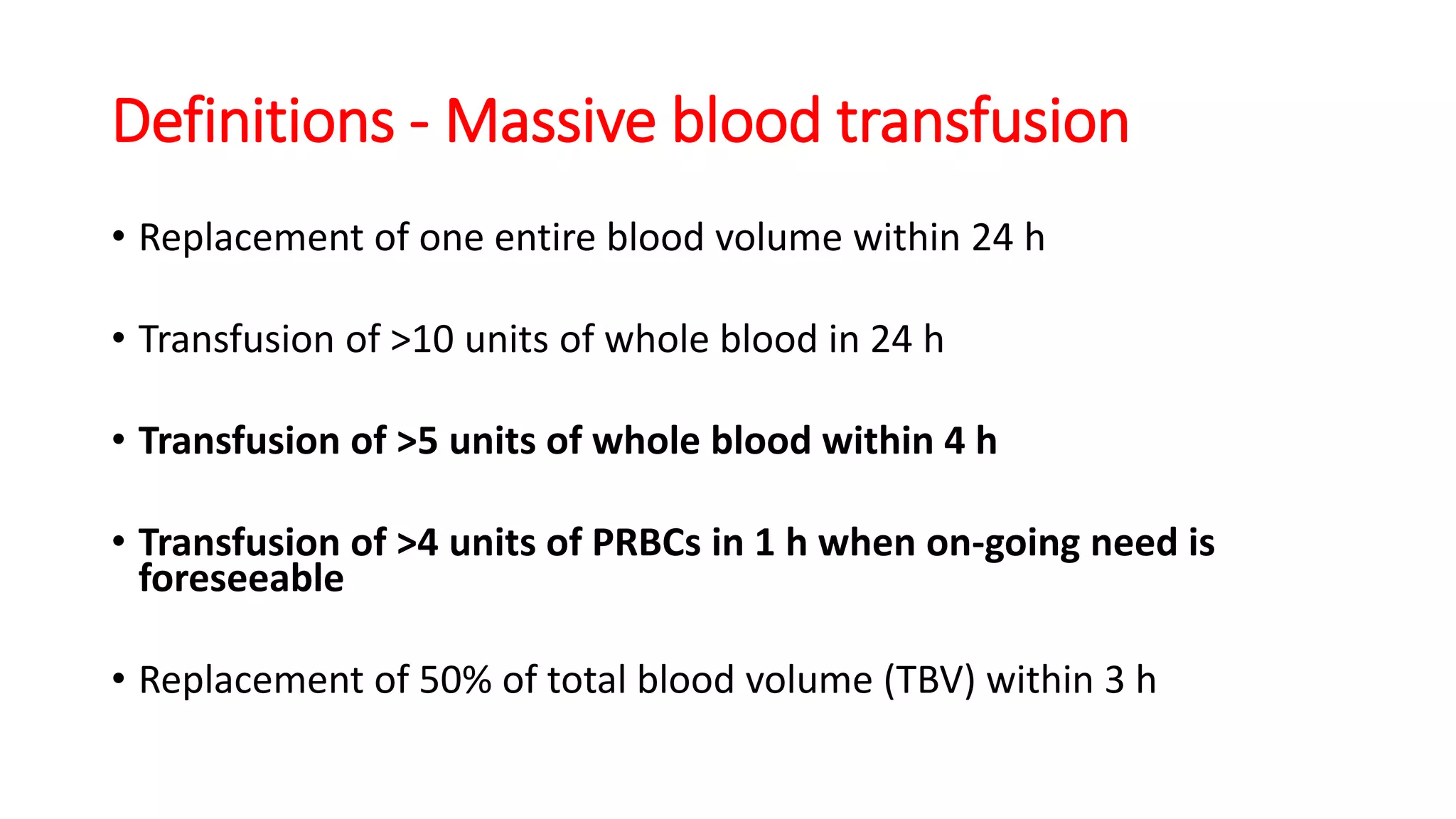
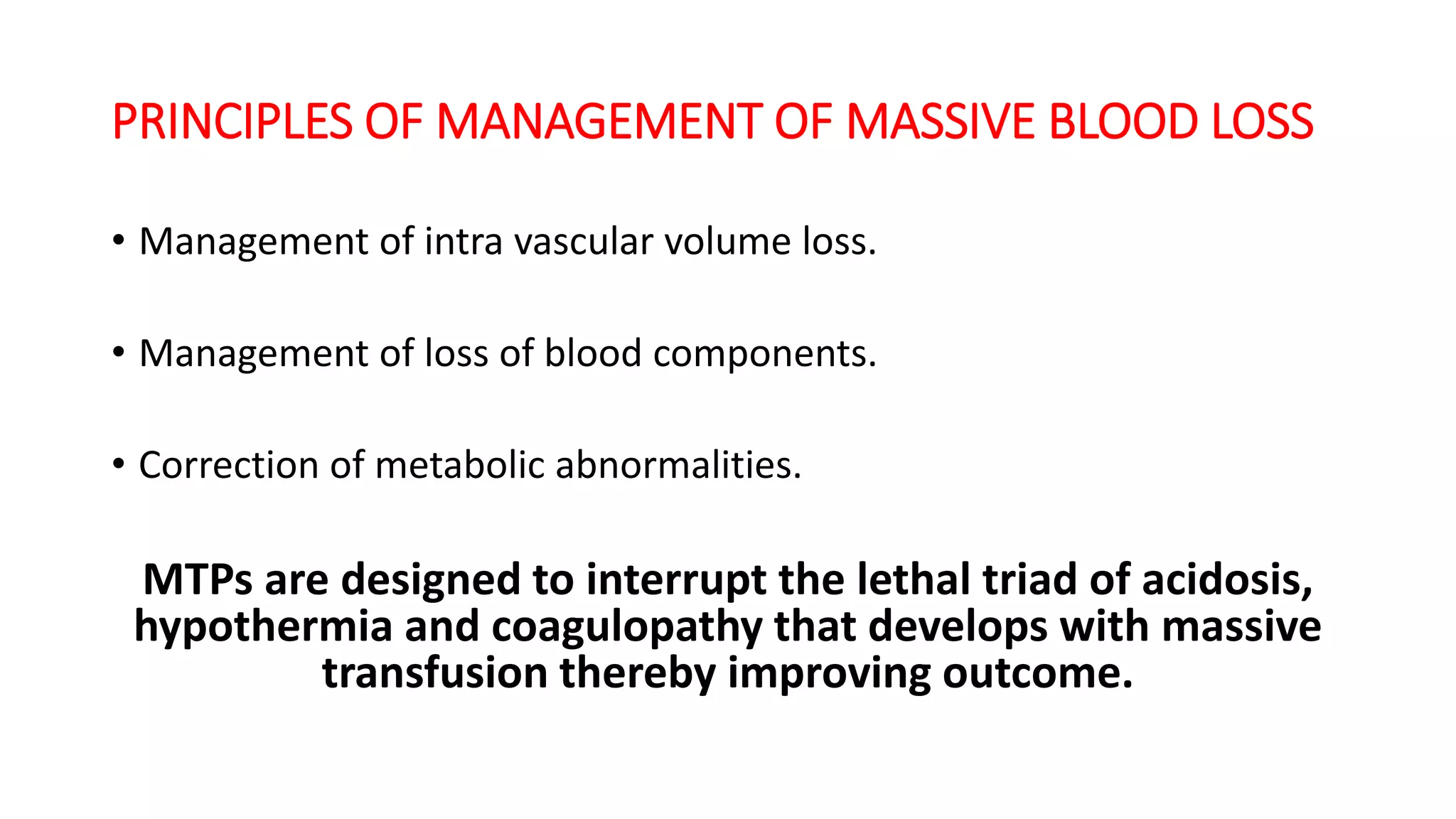
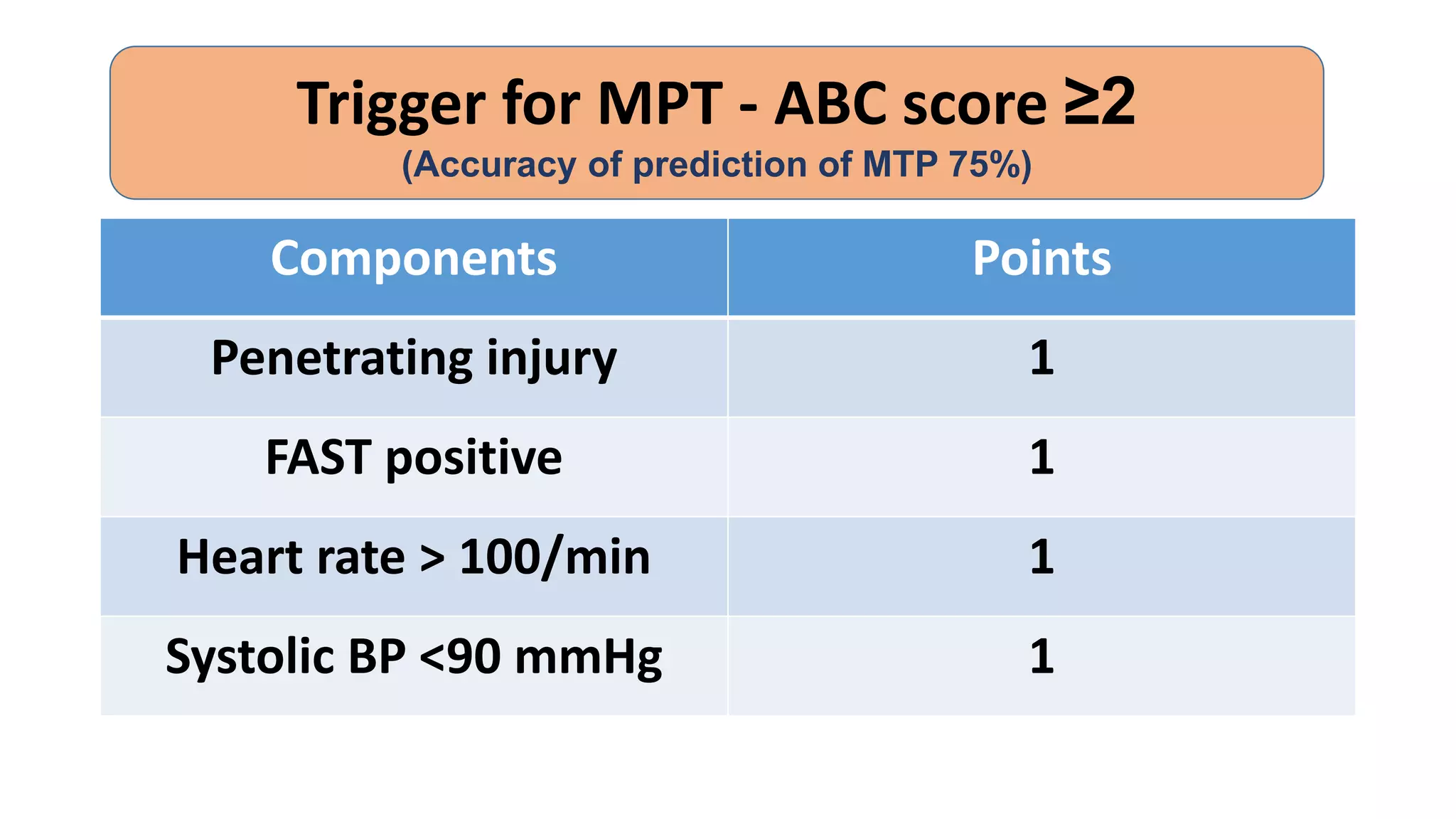
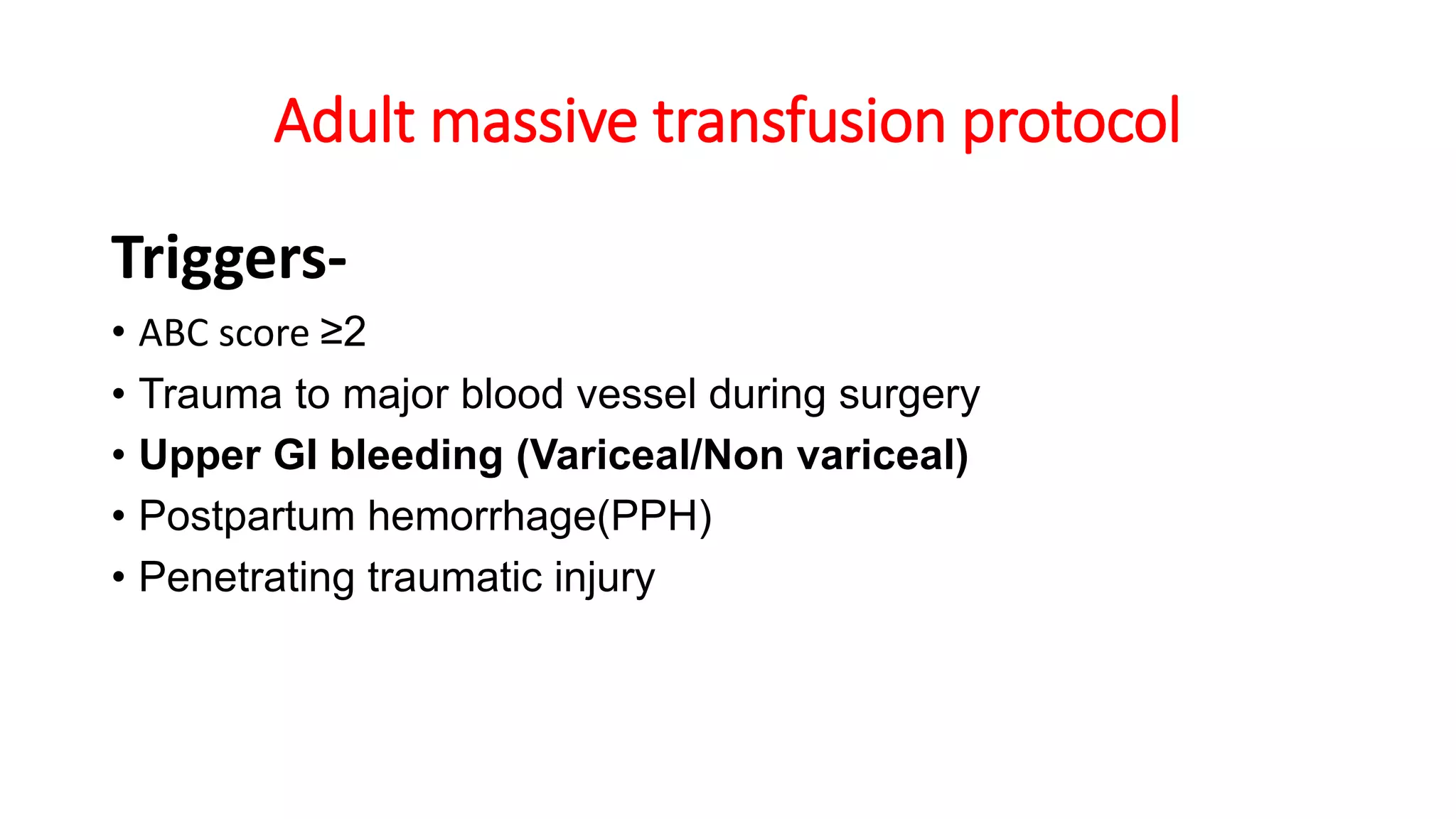
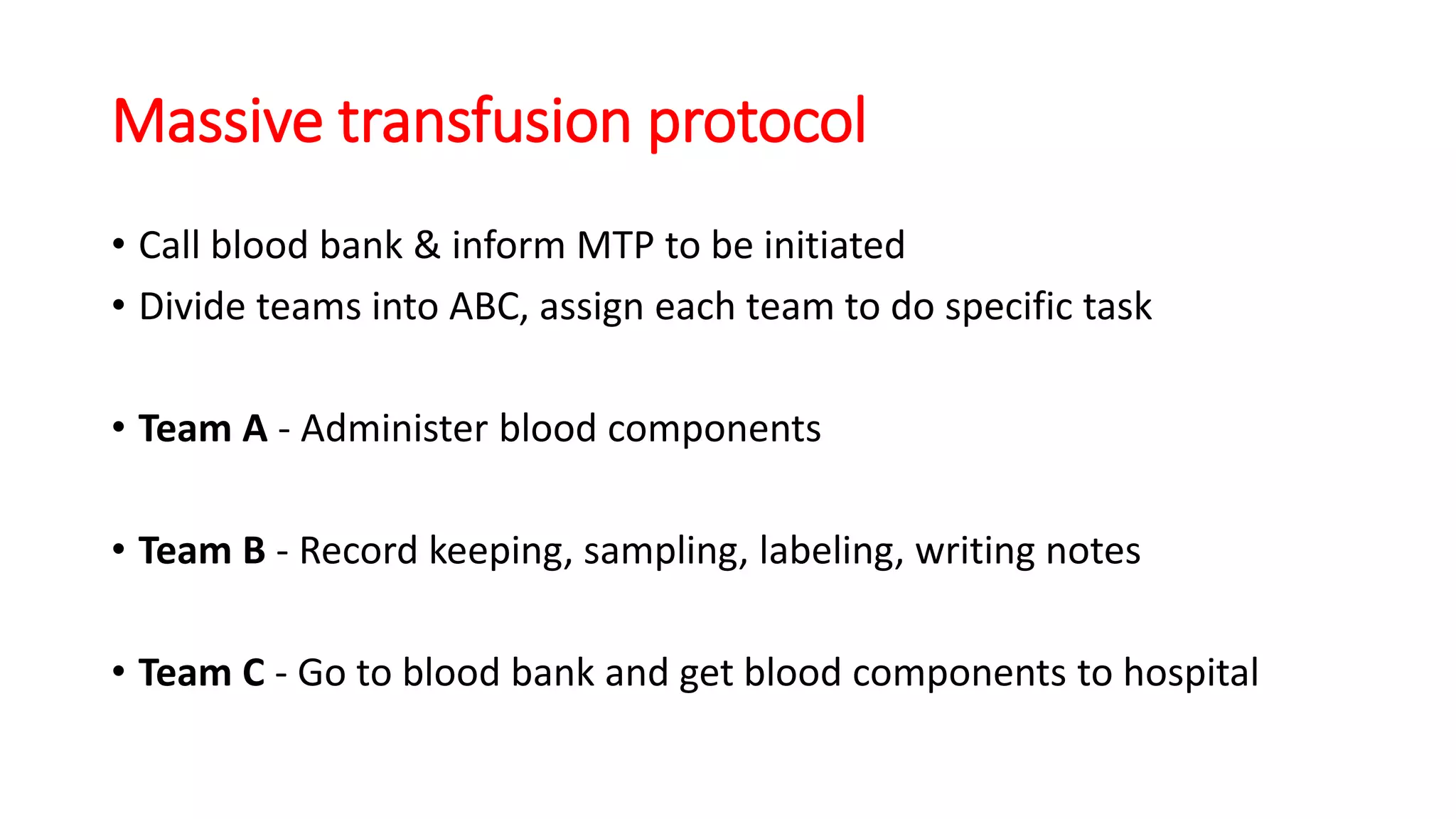
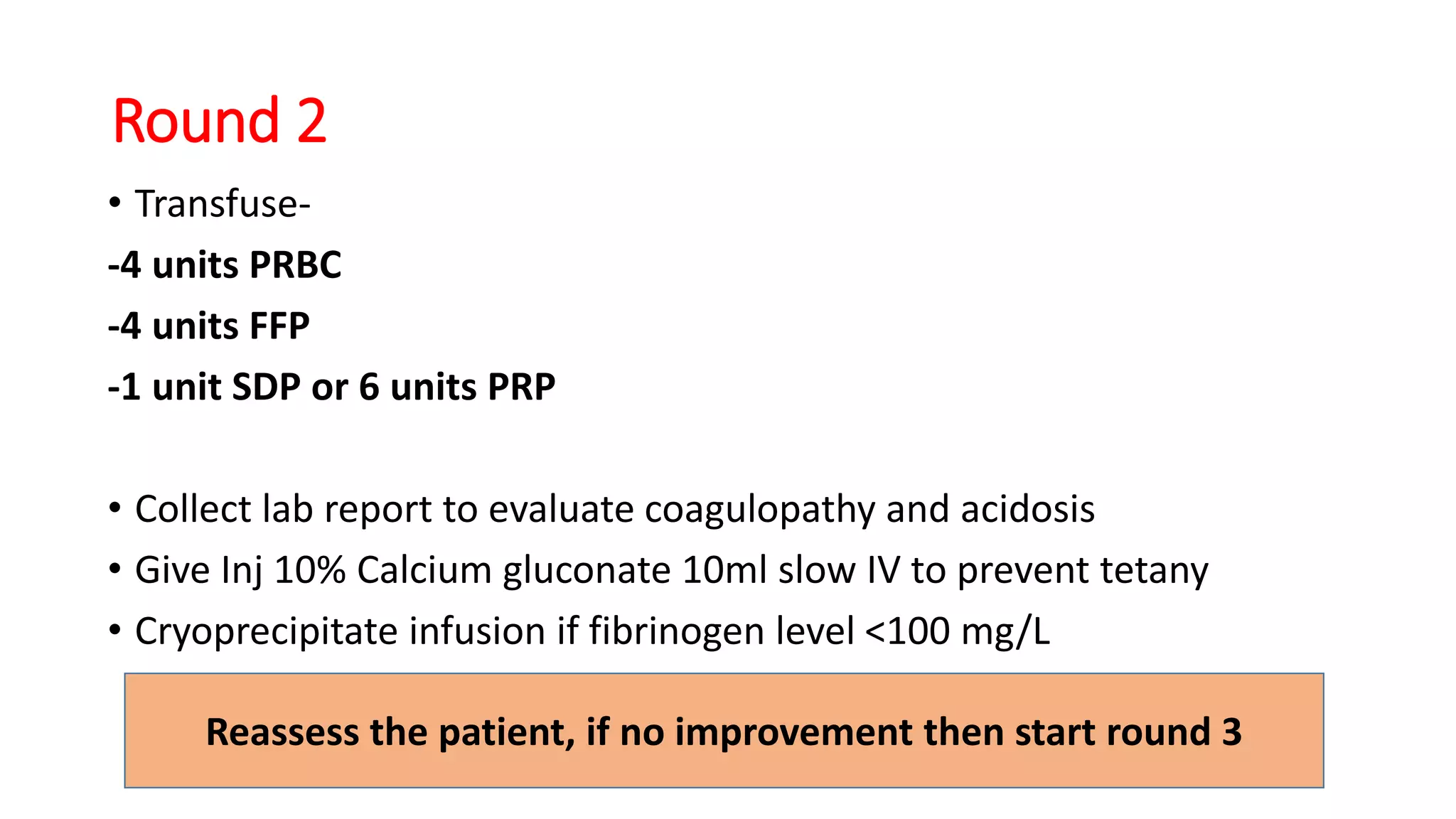
The document discusses a massive transfusion protocol (MTP) for managing massive blood loss. It defines massive transfusion as replacing over half the total blood volume within 3 hours or transfusing more than 10 units in 24 hours. Massive bleeding can cause acidosis, hypothermia, and coagulopathy, known as the "lethal triad." MTPs are designed to interrupt this triad and improve outcomes. The protocol outlines assessing triggers, activating a response team, and proceeding through rounds of rapidly transfusing blood products like packed red blood cells, fresh frozen plasma, platelets and calcium while monitoring lab values to guide hemostatic resuscitation.