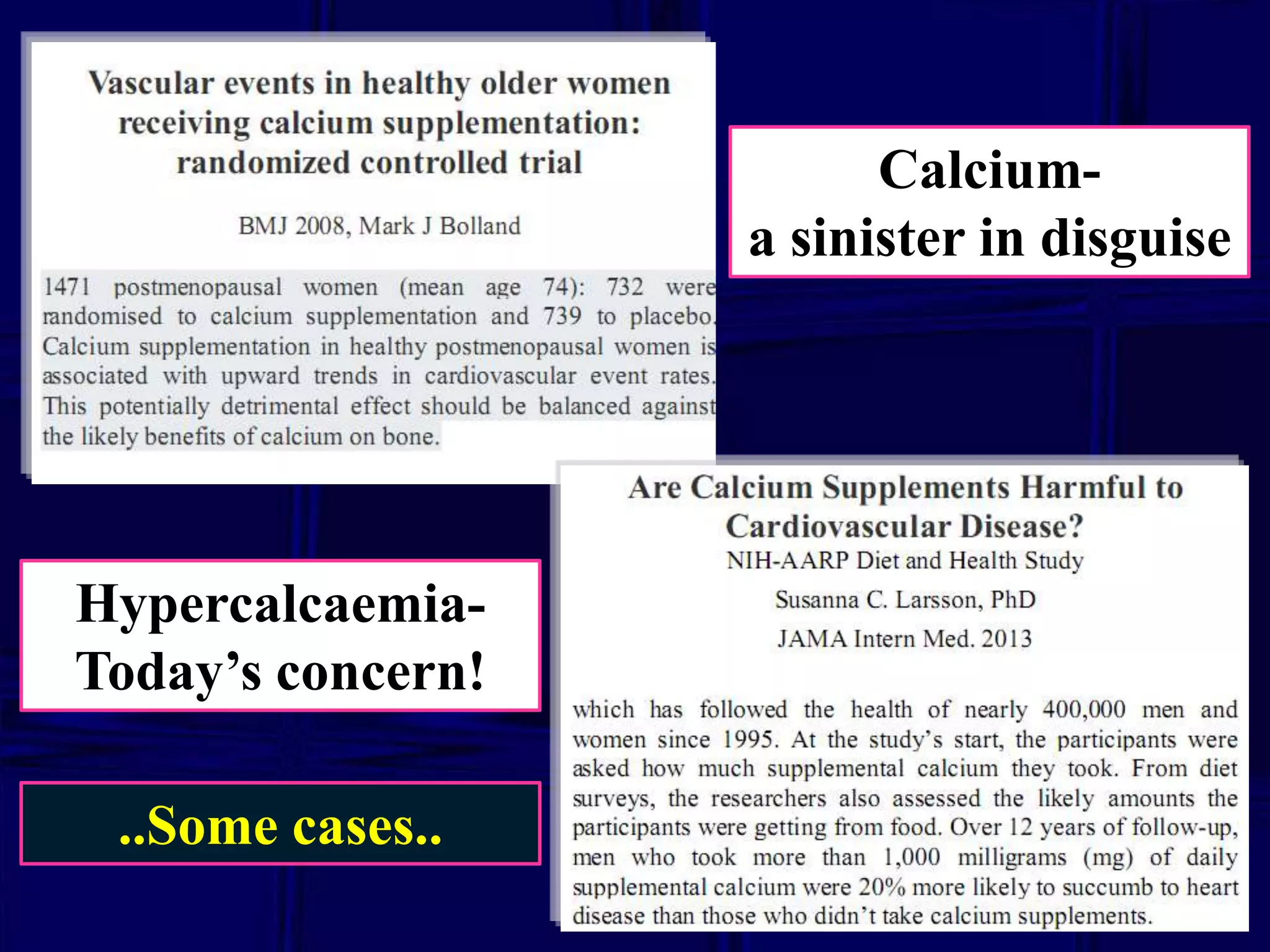
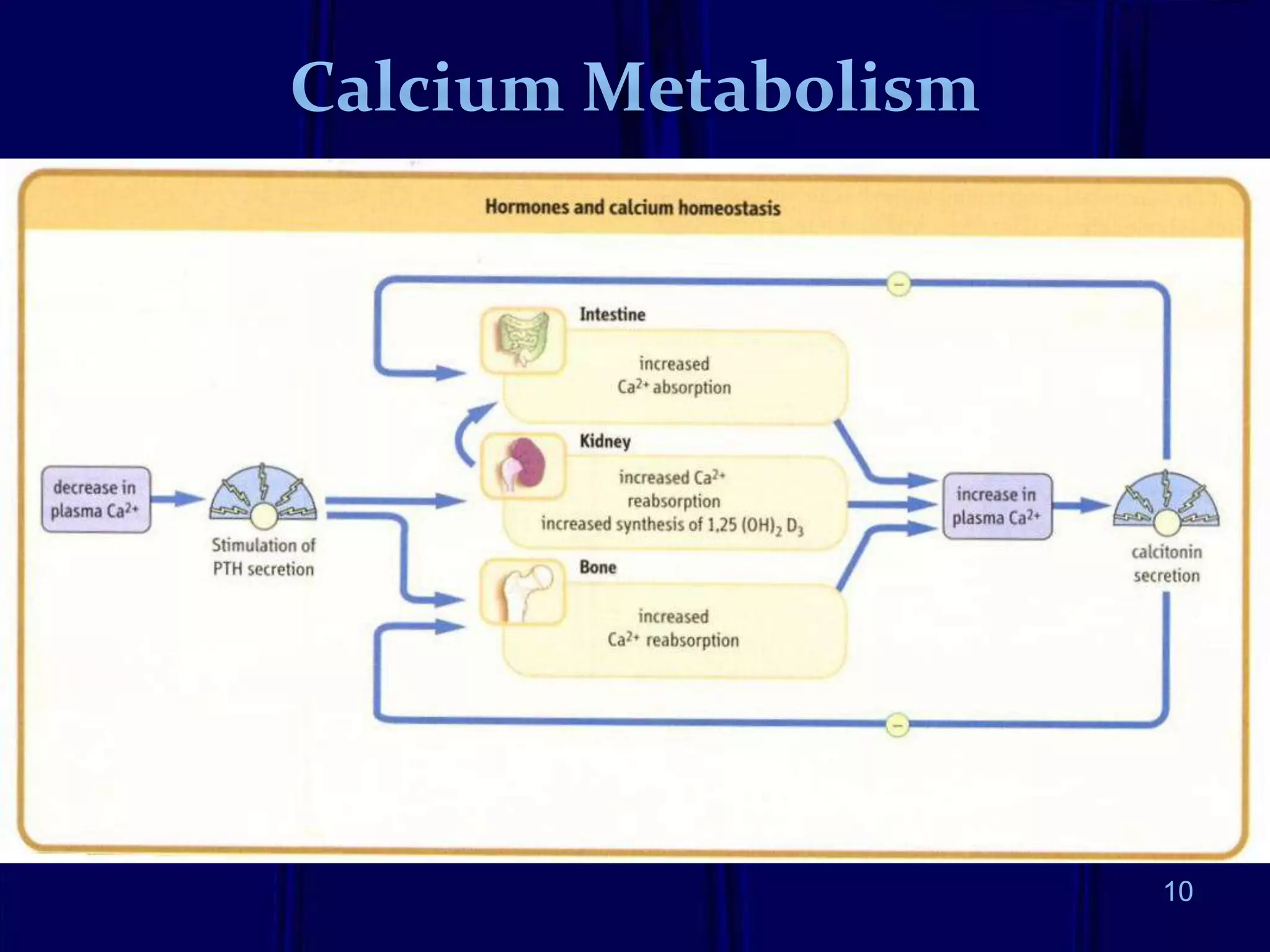
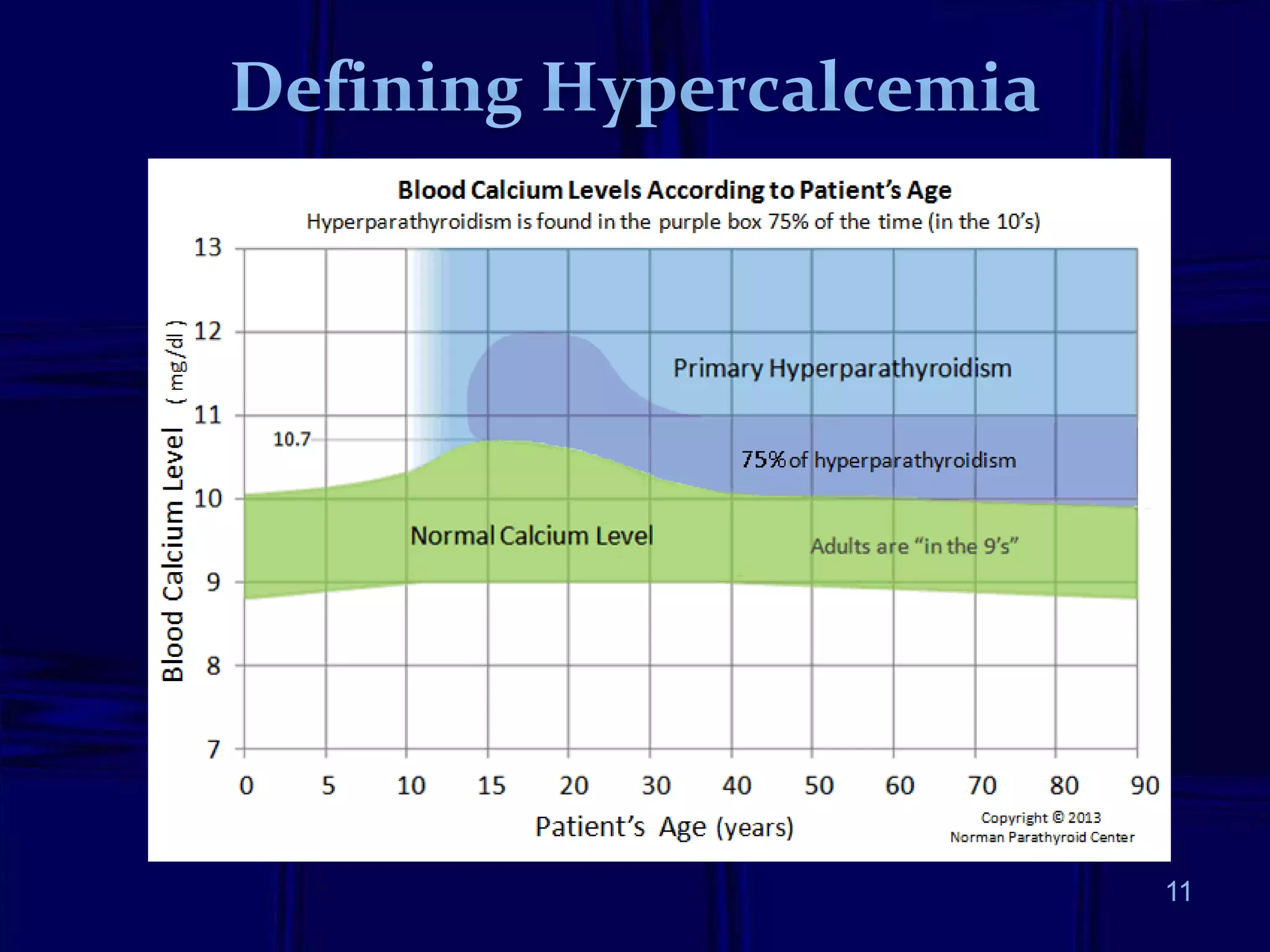
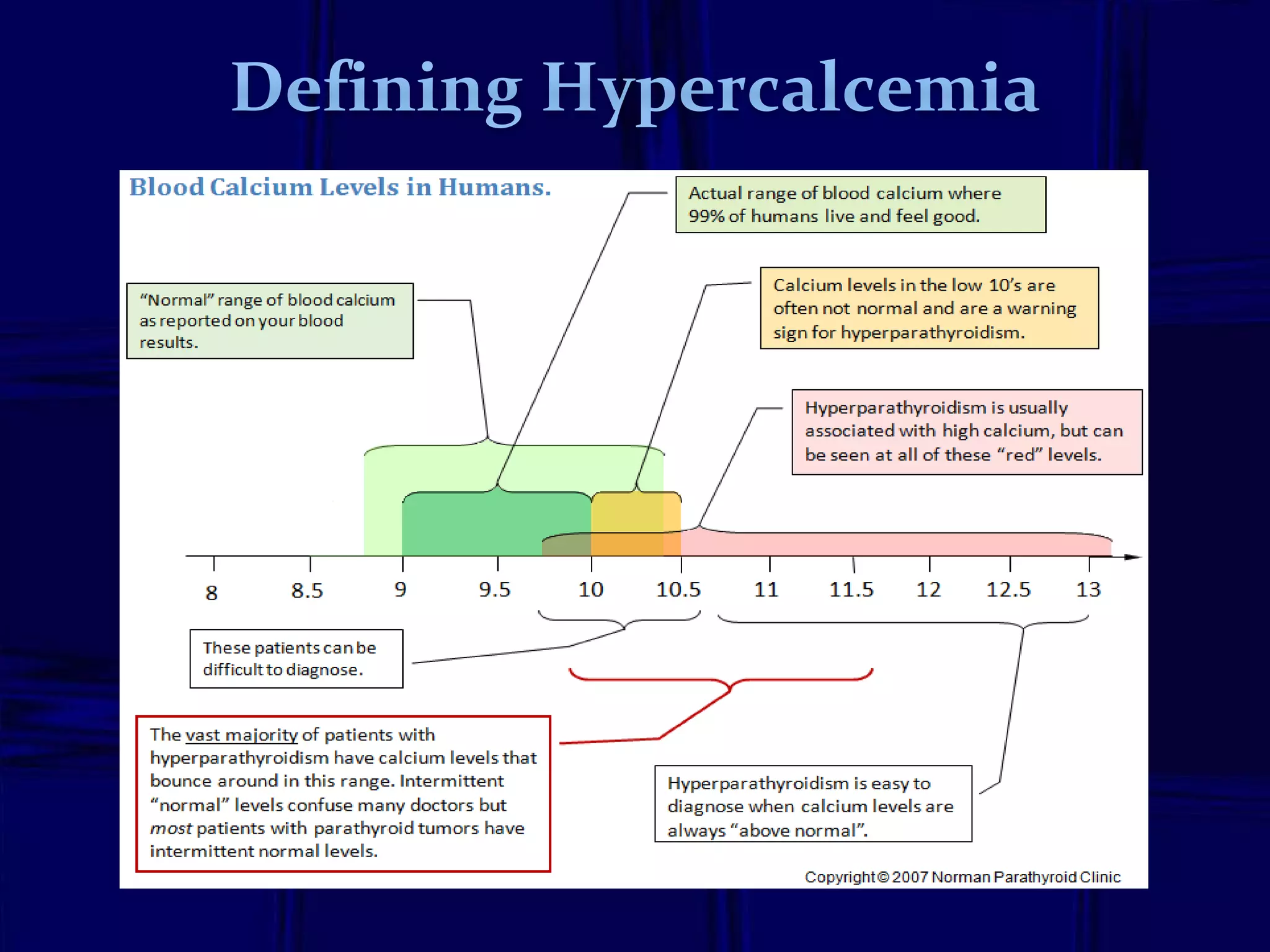
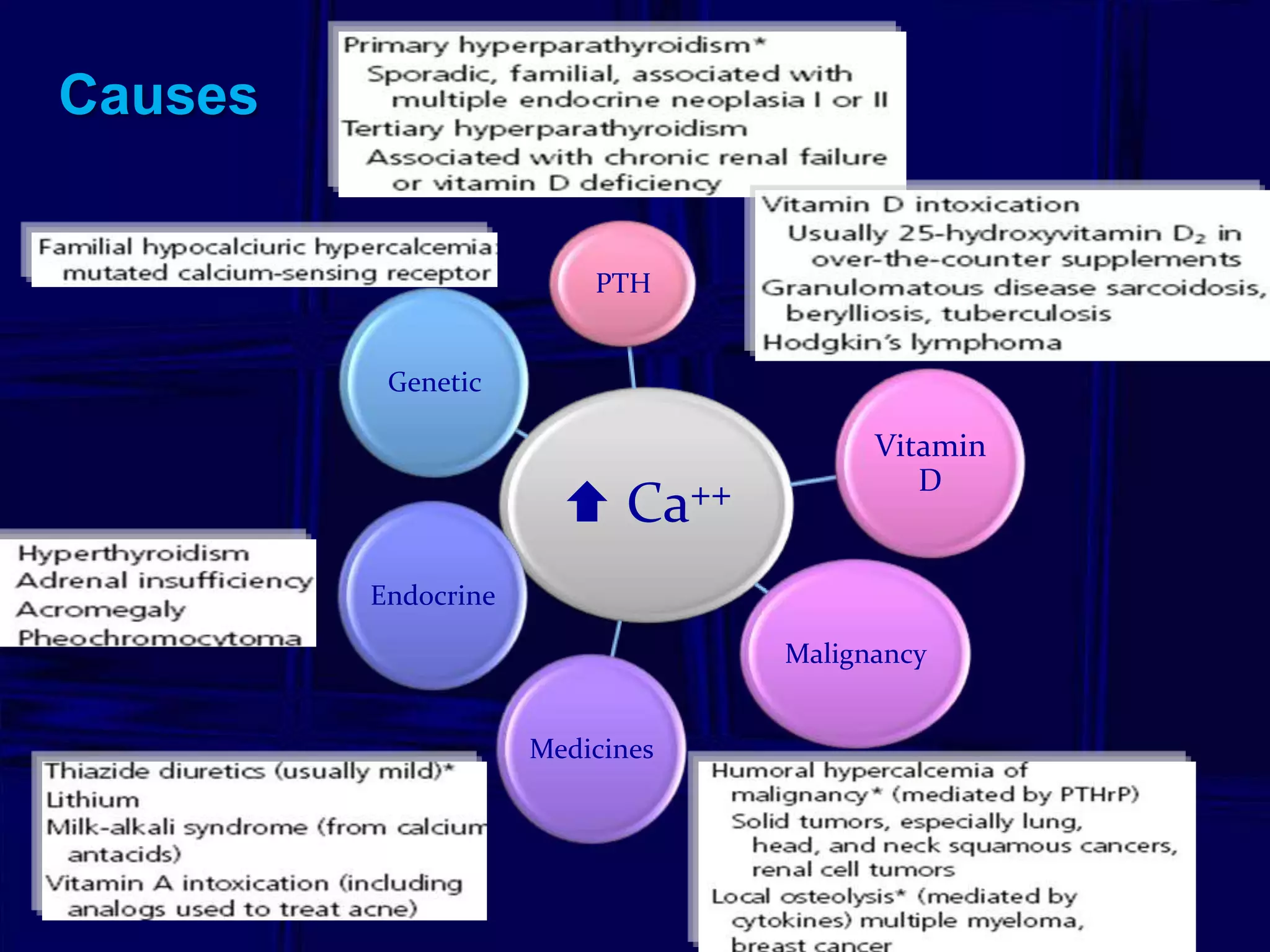
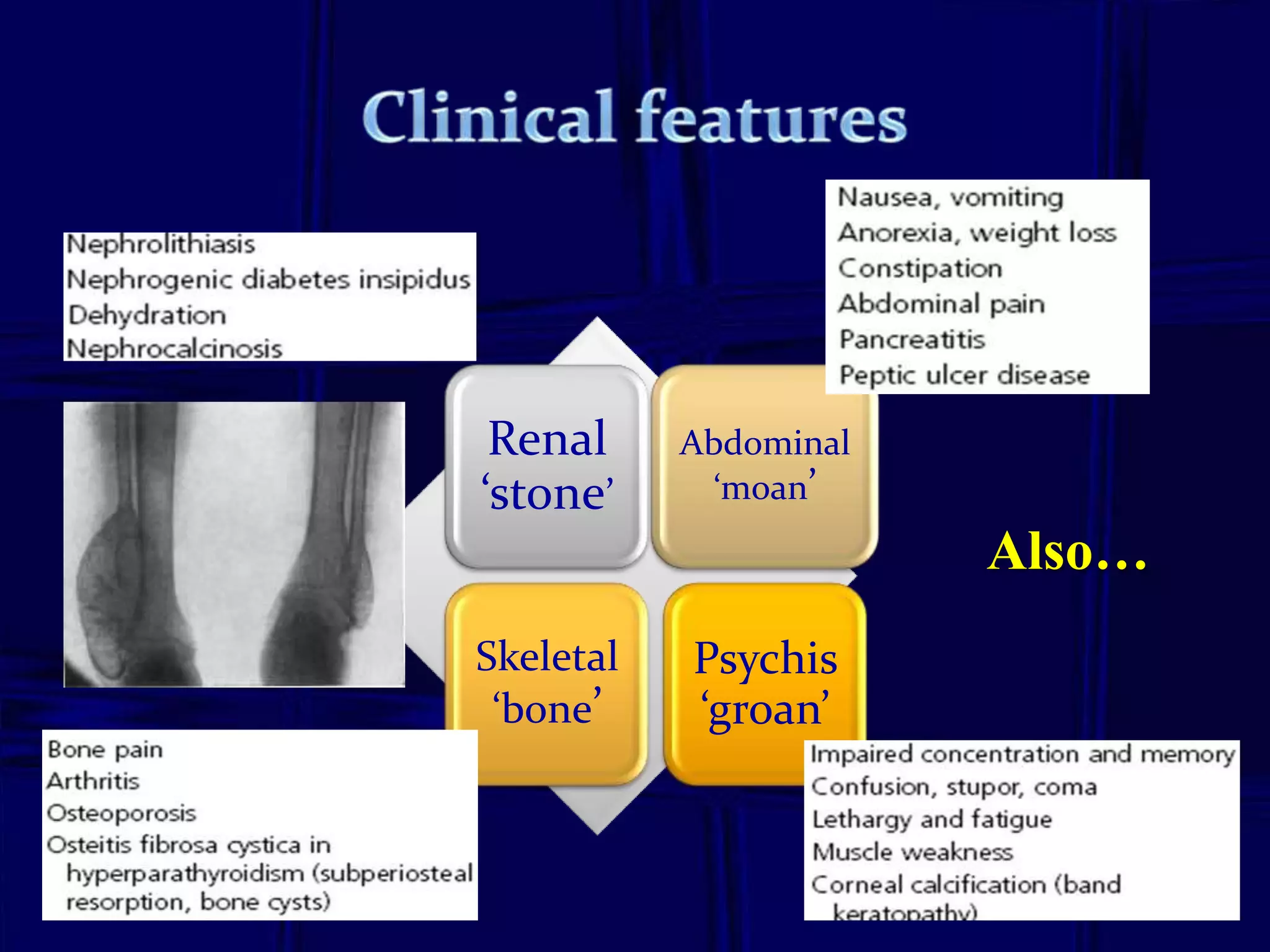
1. Calcium is essential for bone and muscle health but can become elevated, known as hypercalcemia, through various causes like primary hyperparathyroidism, vitamin D overdose, or malignancy.
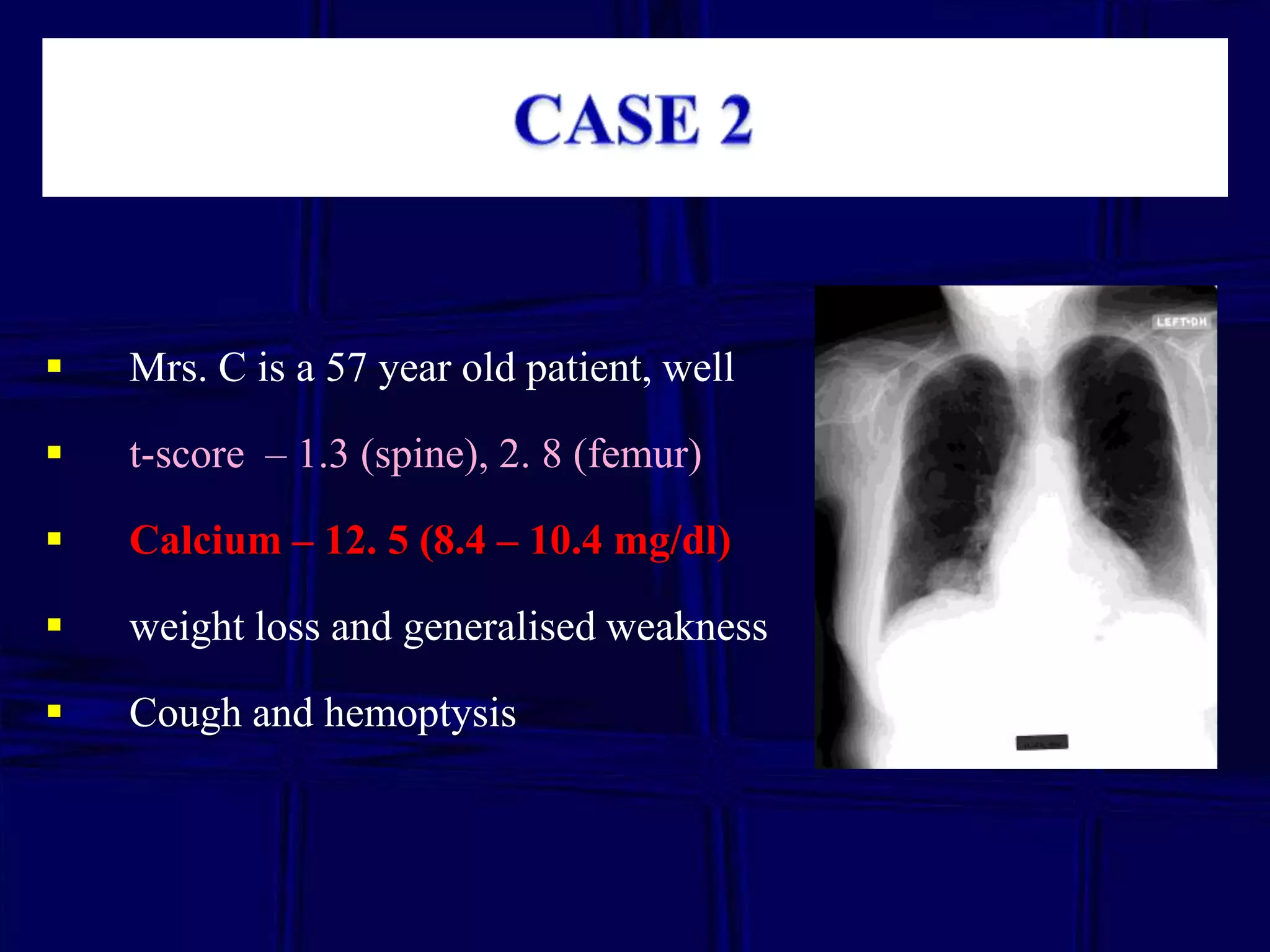
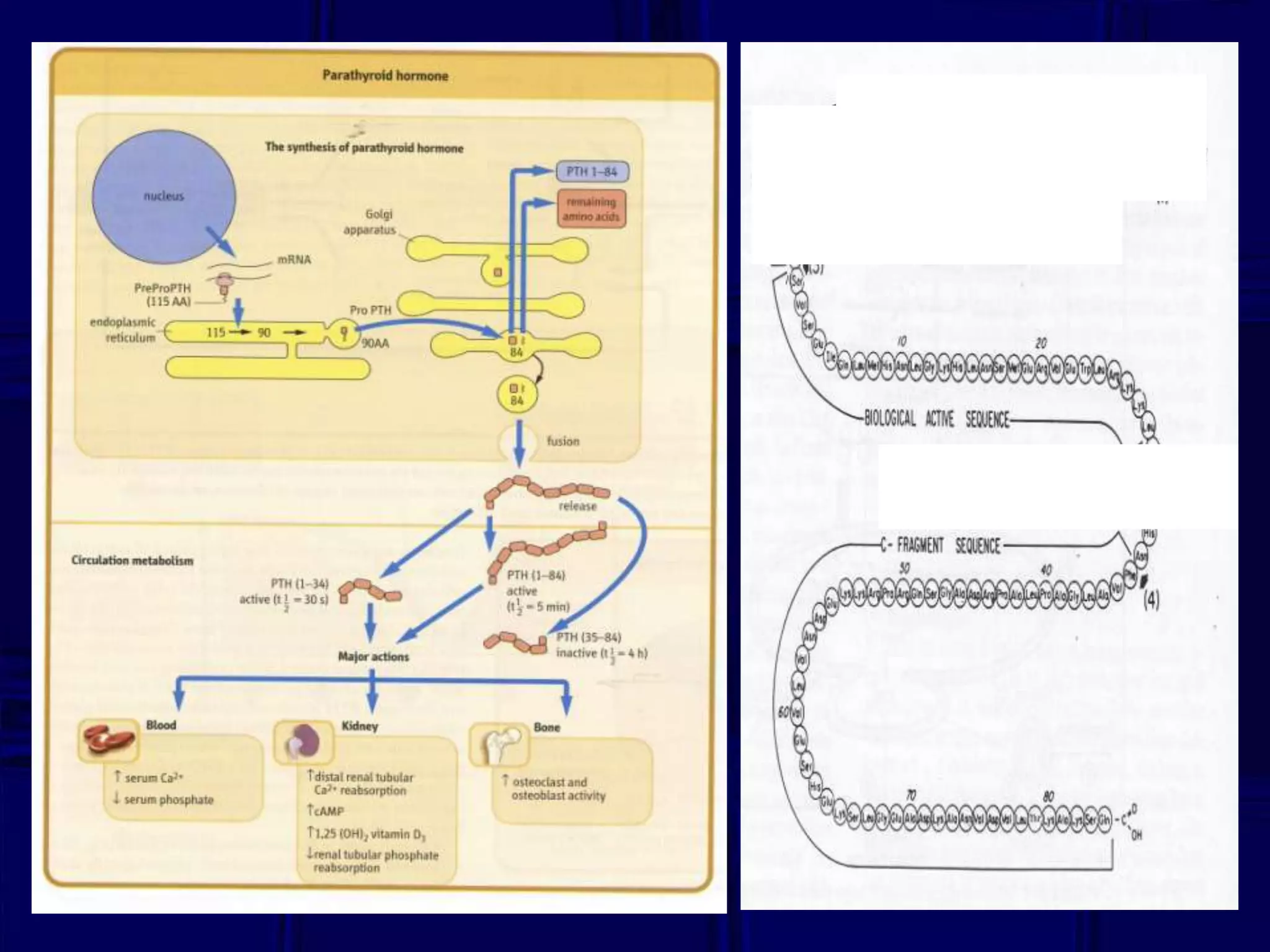
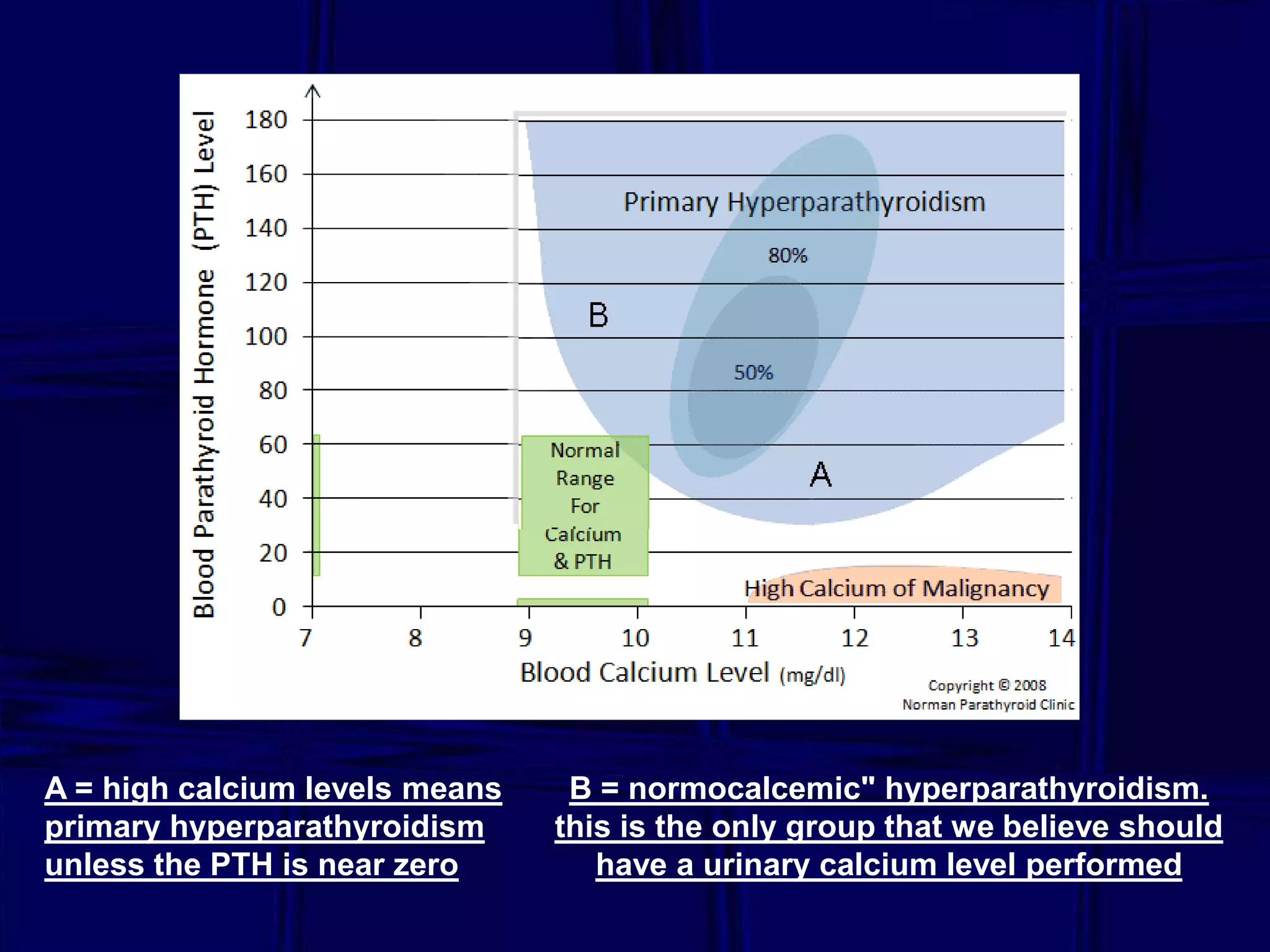
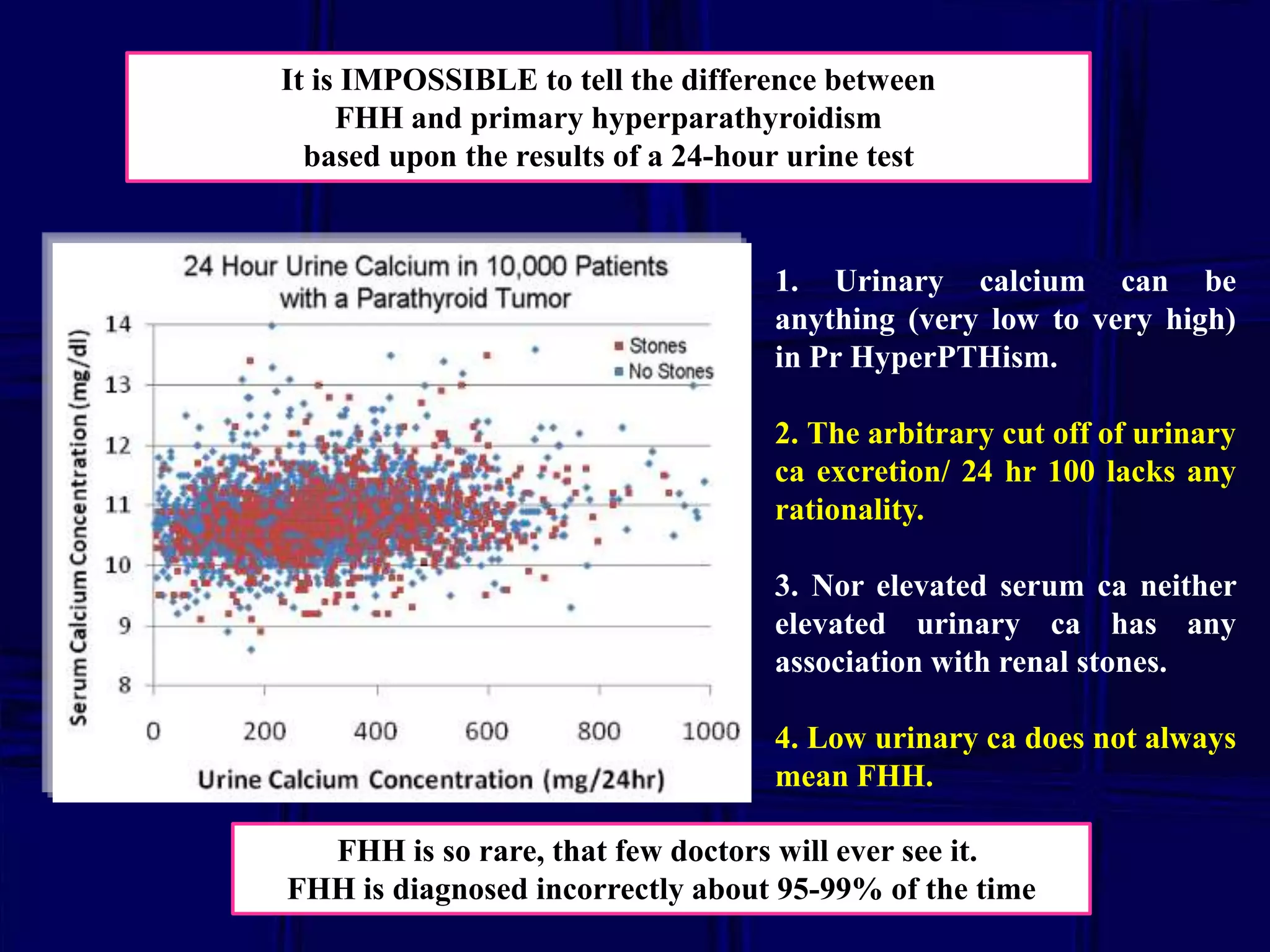
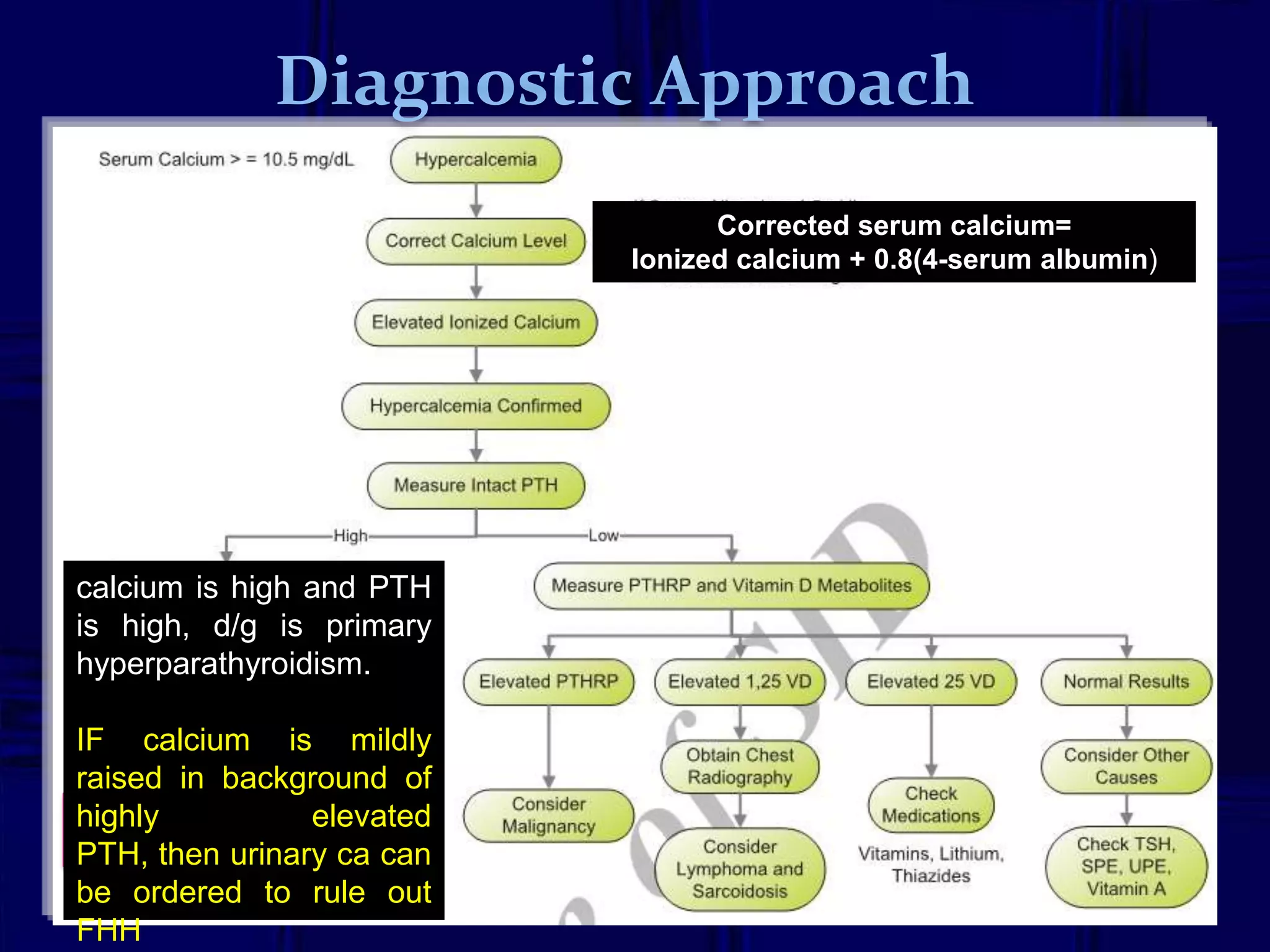
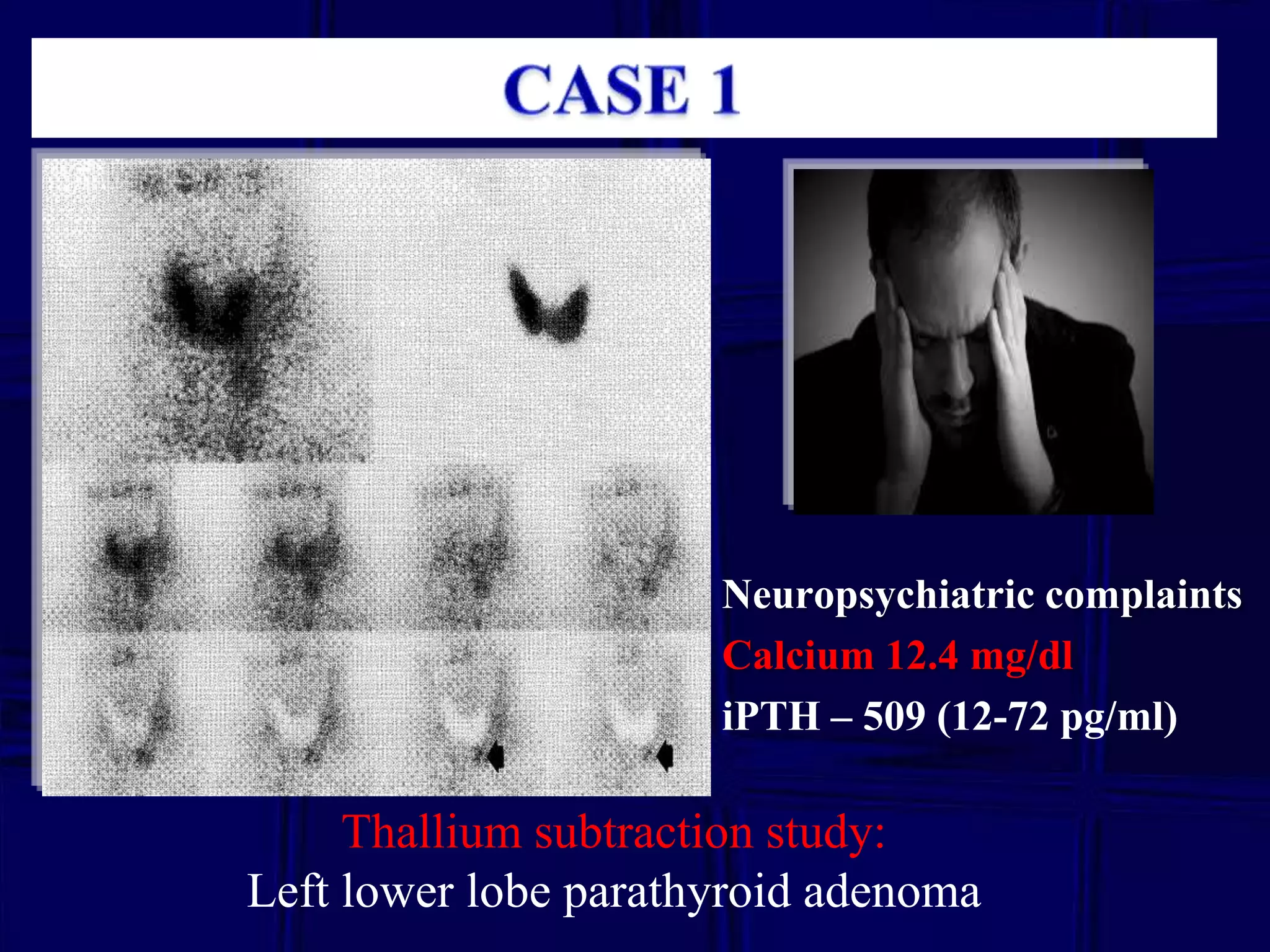
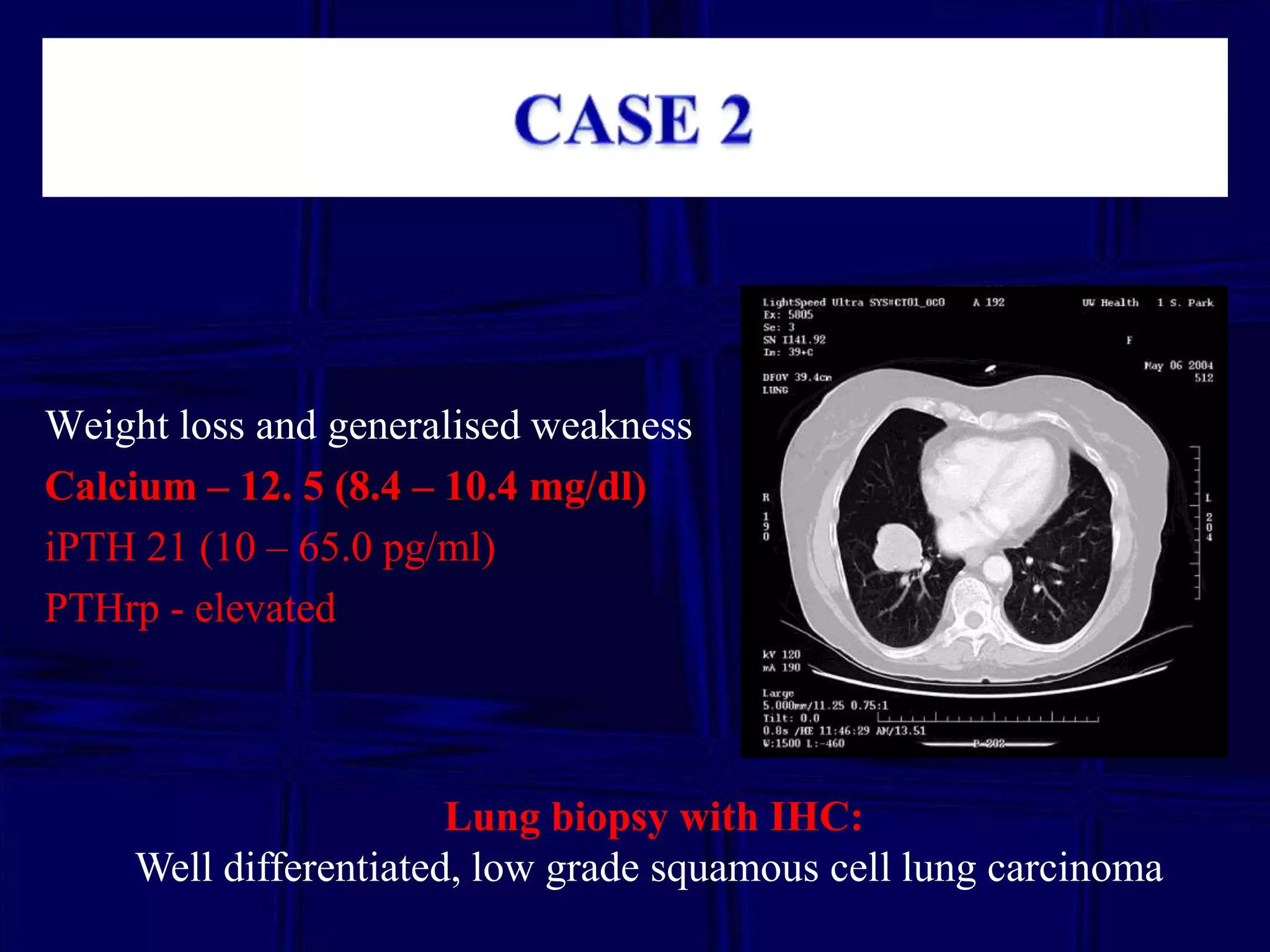
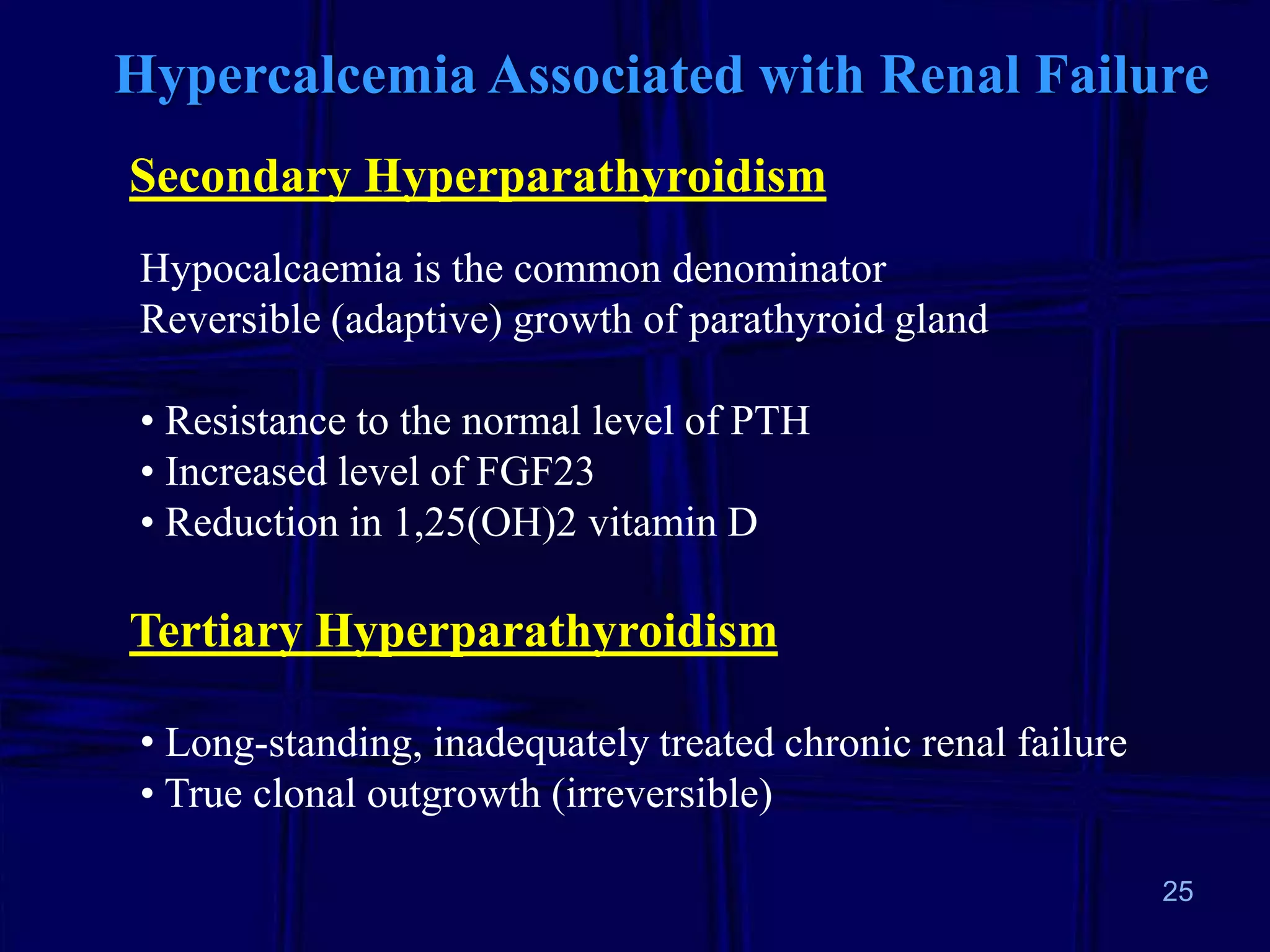
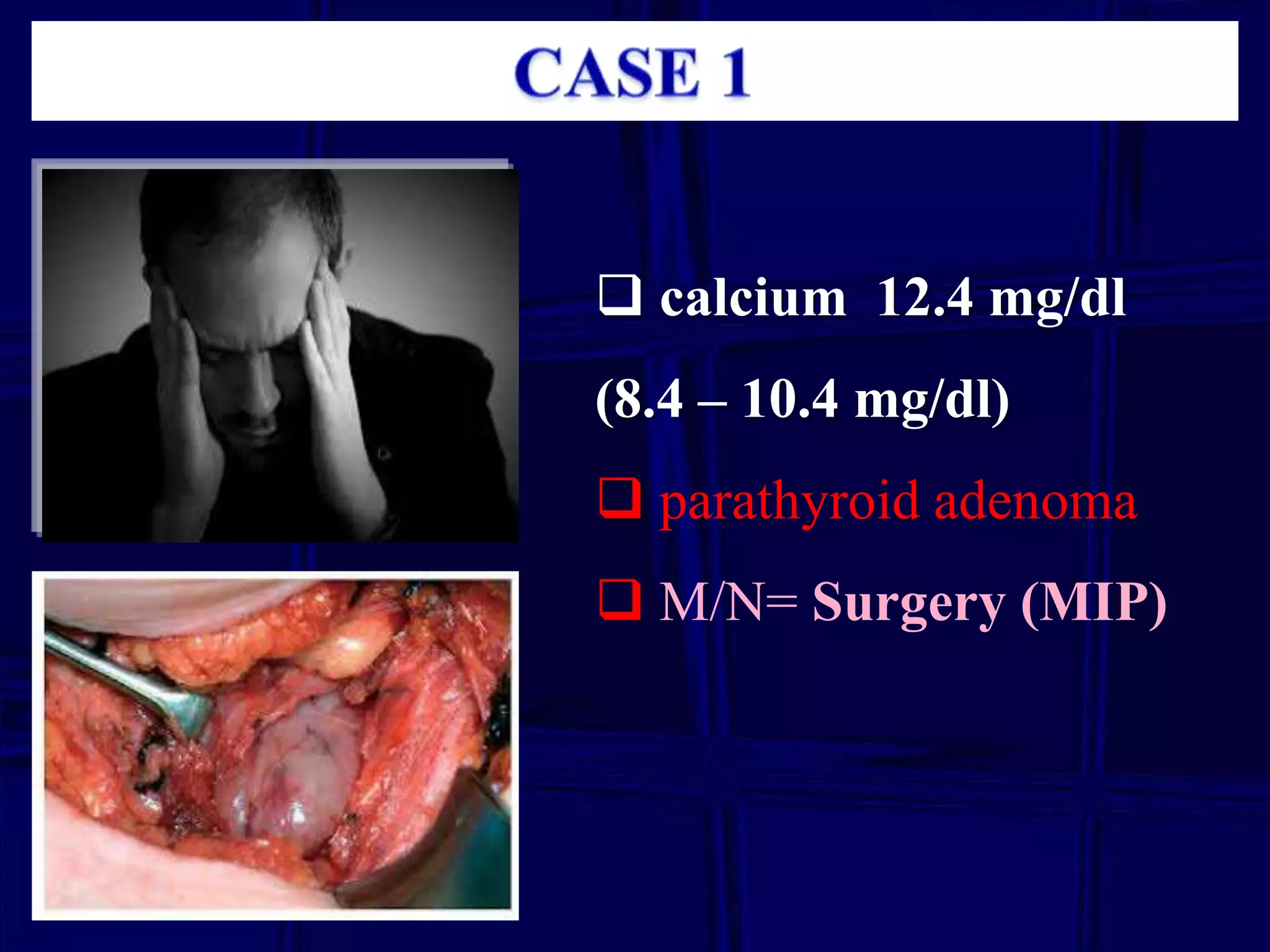
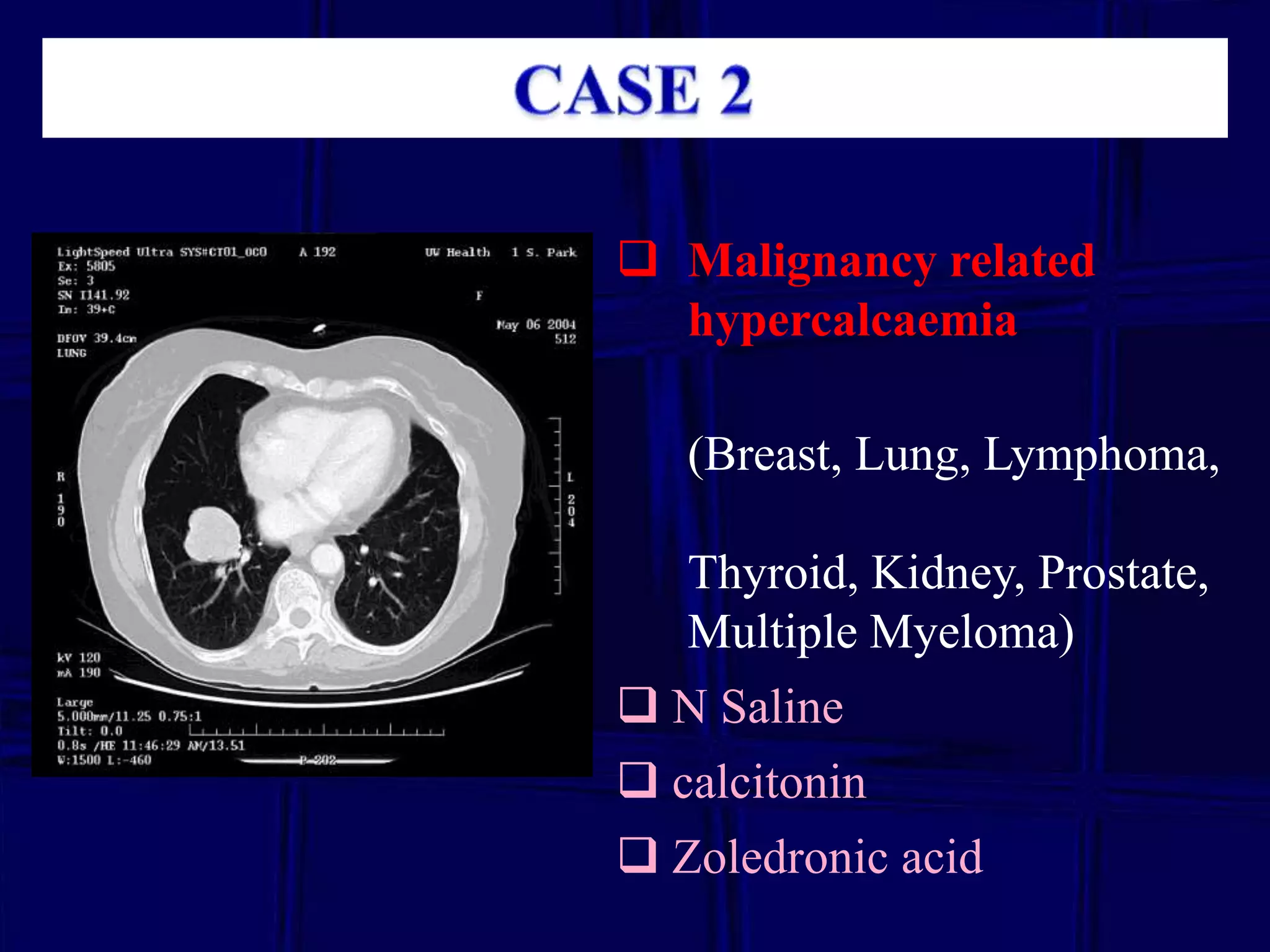
2. Evaluation of elevated calcium includes measuring PTH levels to determine the cause, and cases presented demonstrate workup and management of different hypercalcemia etiologies.
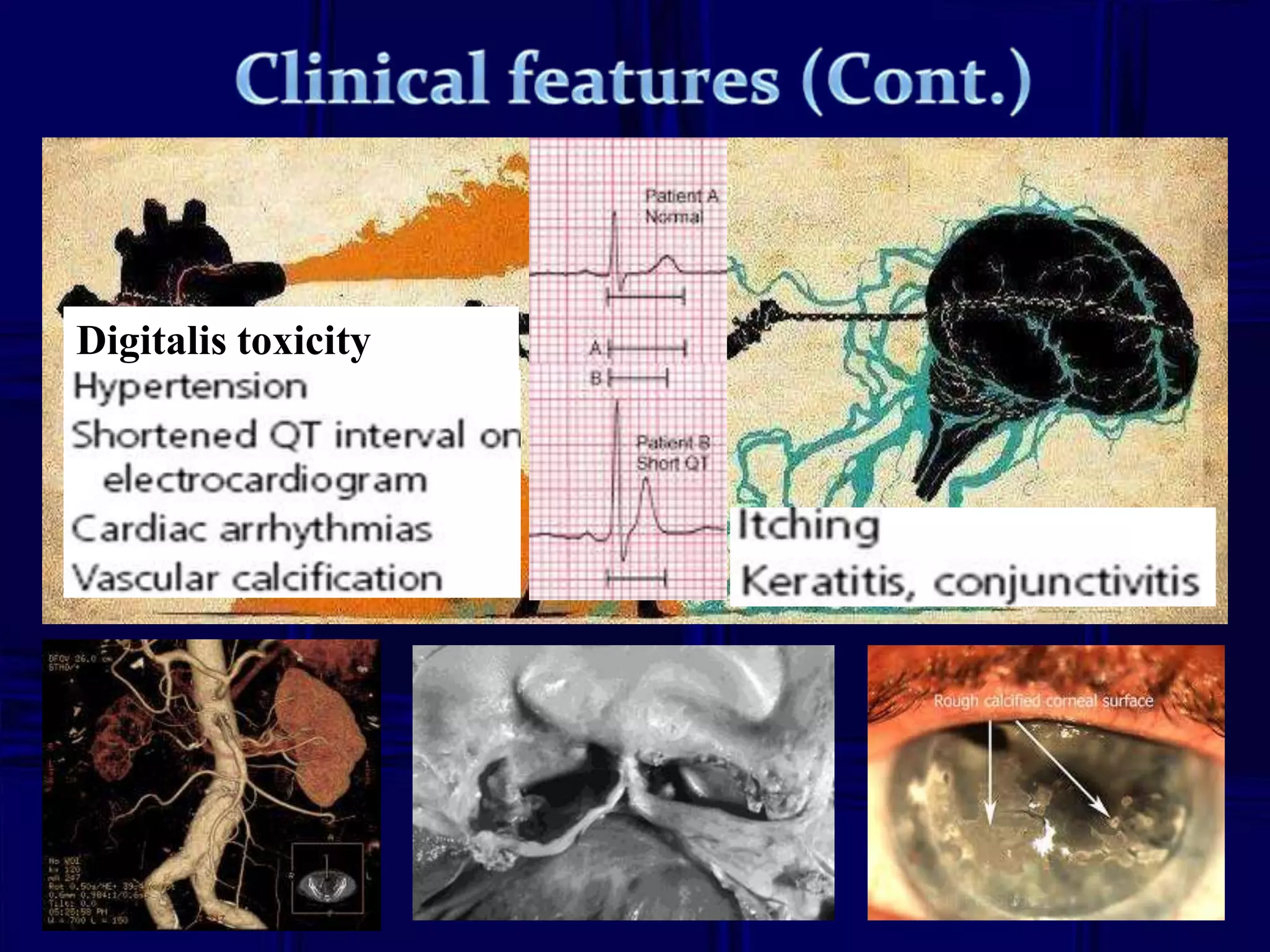
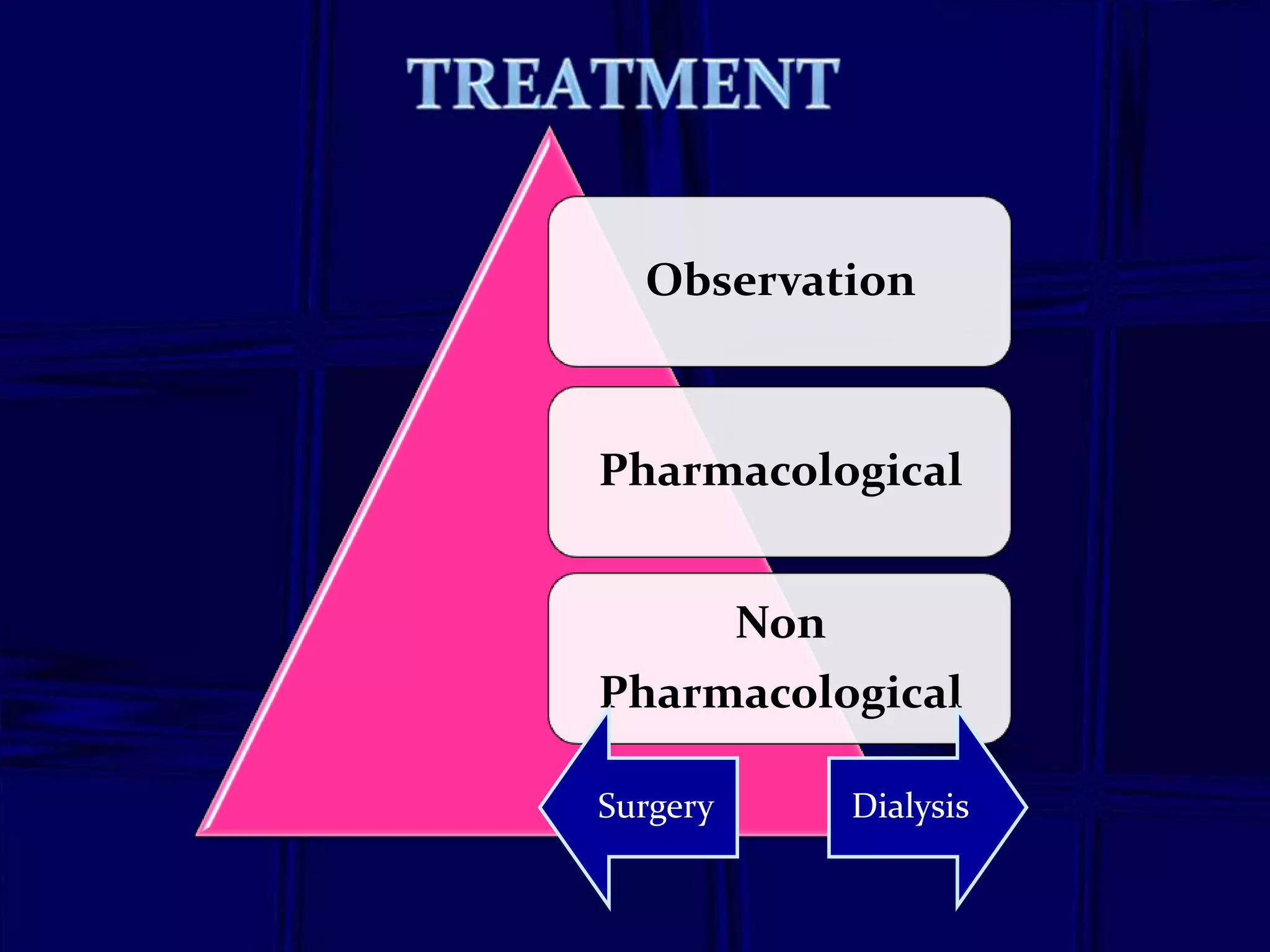
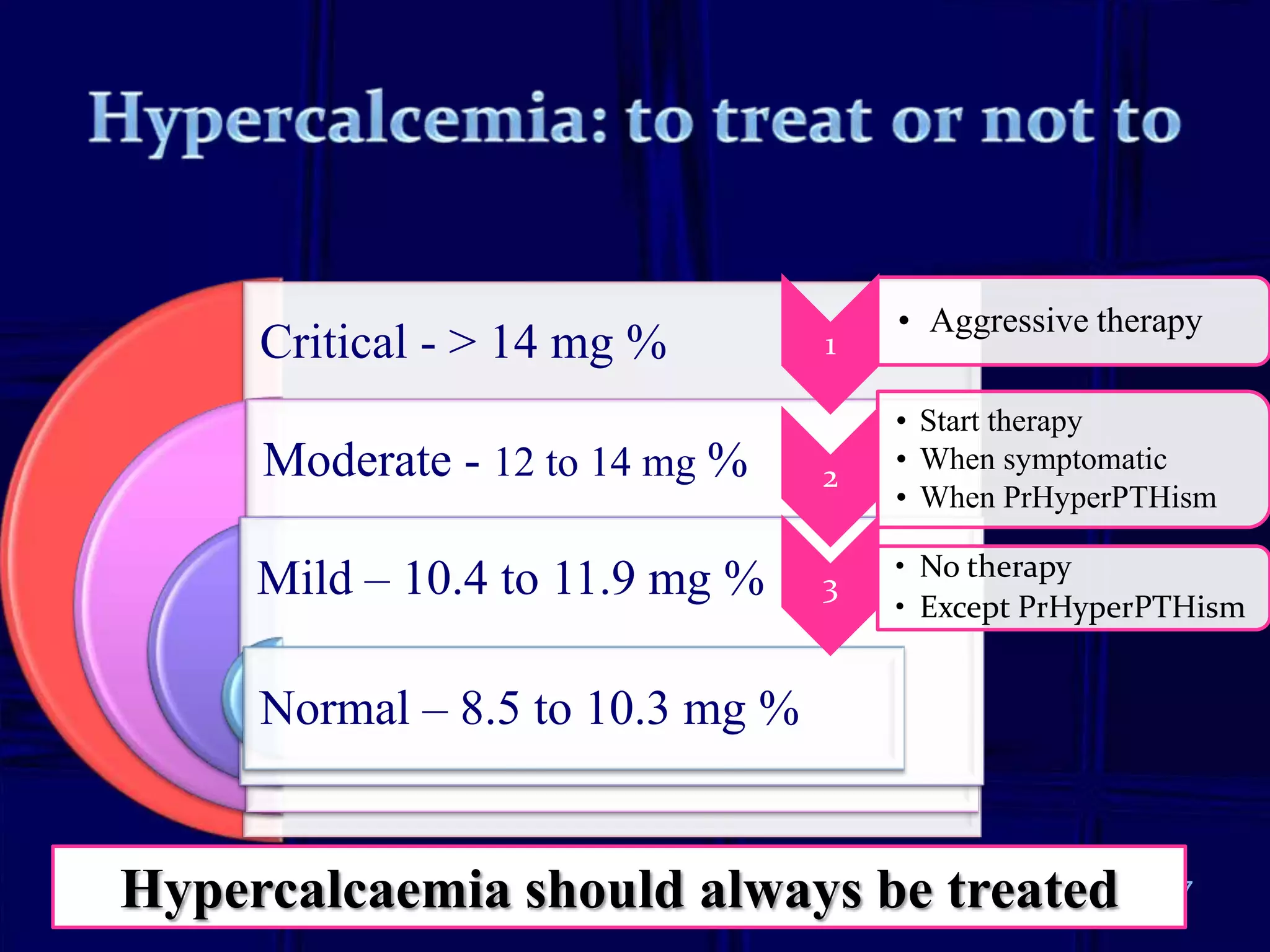
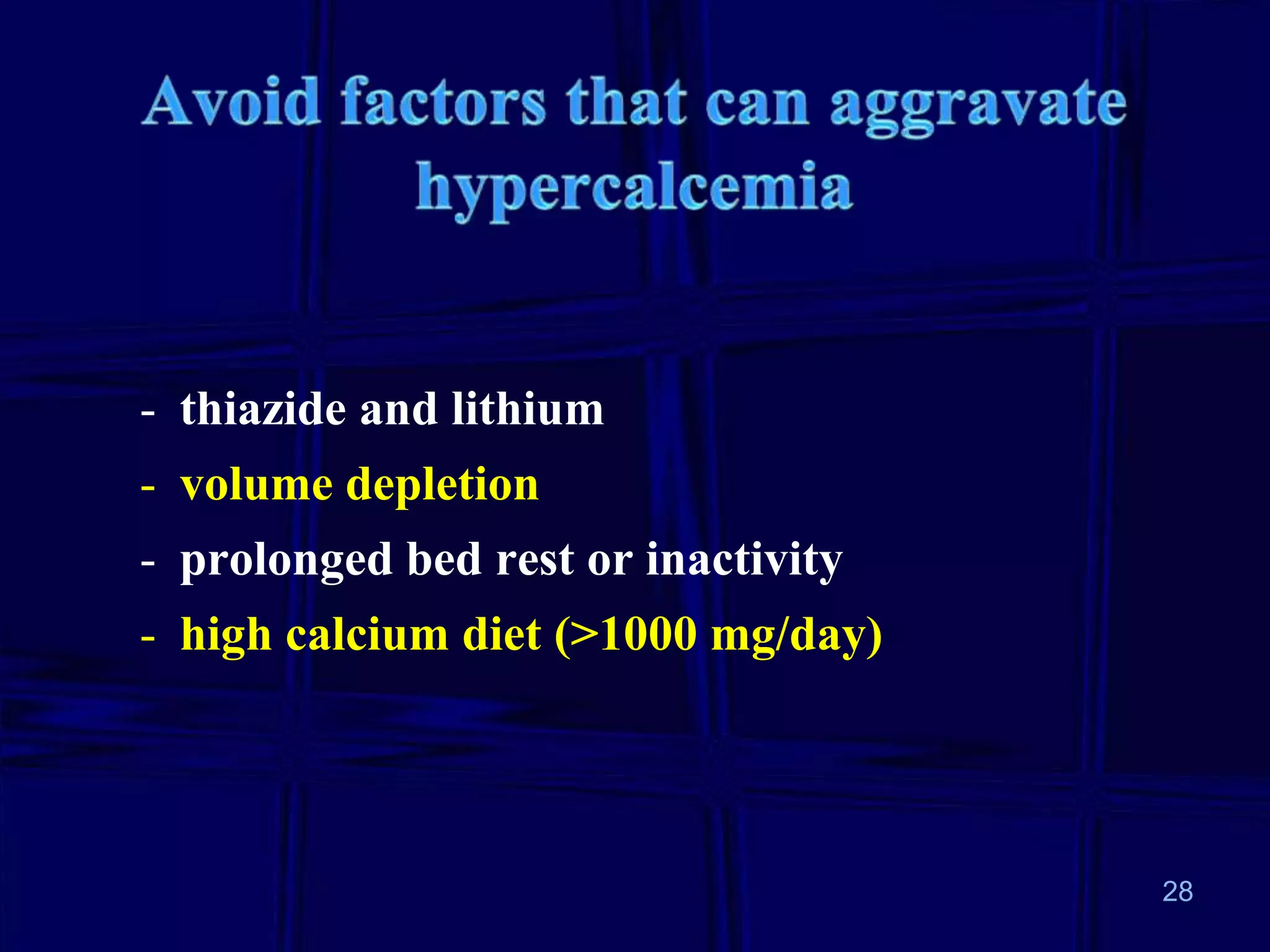
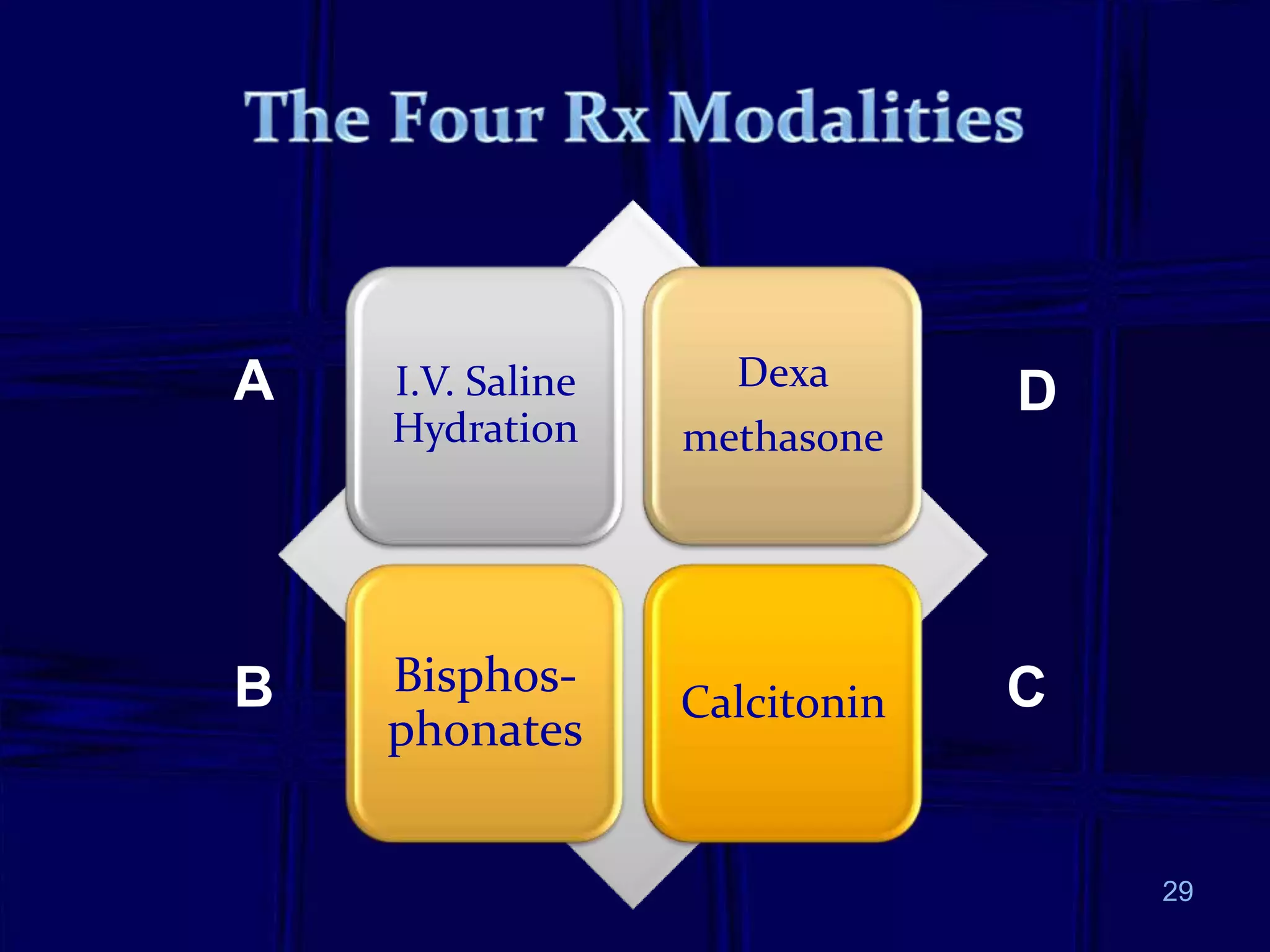
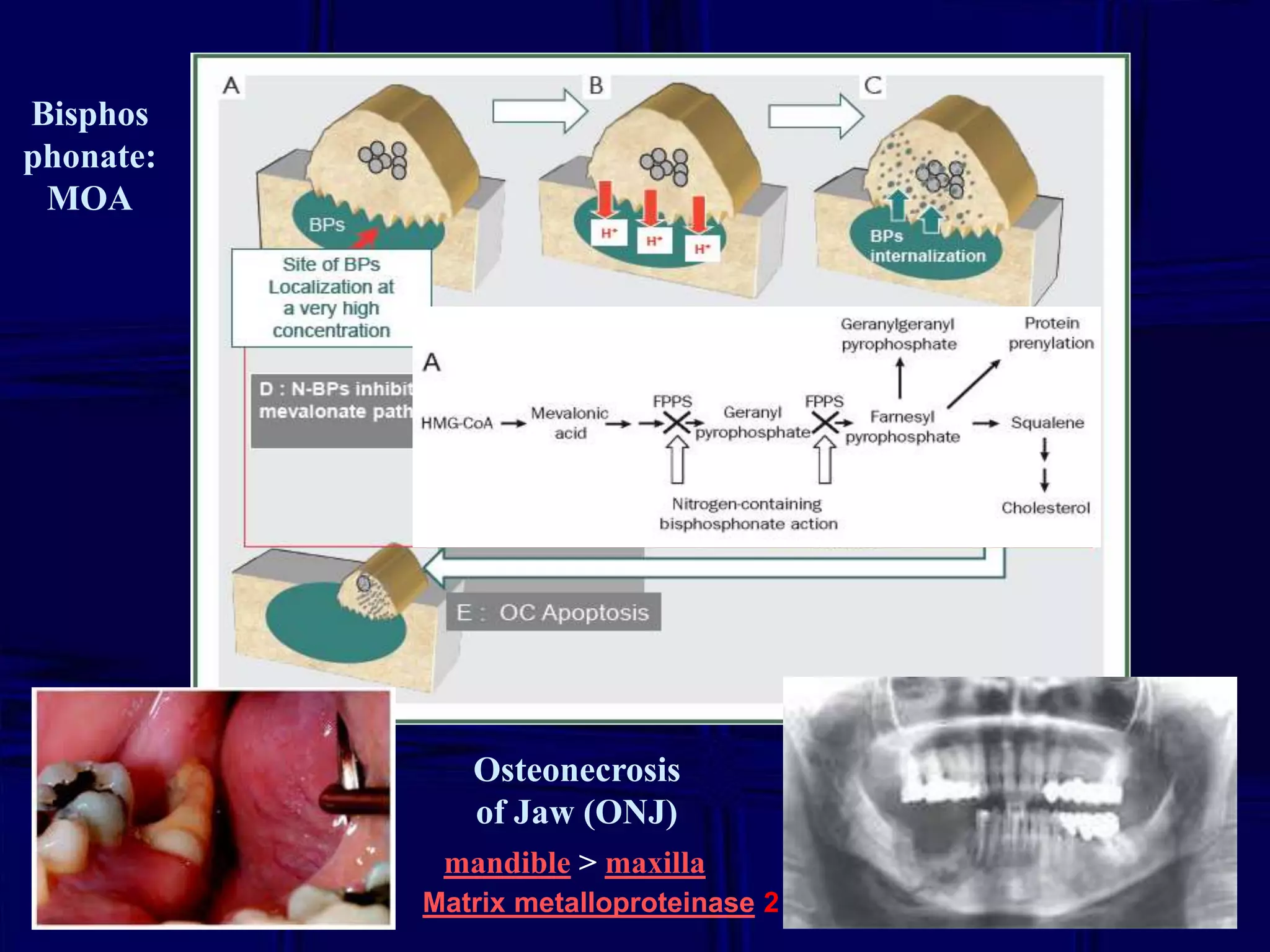
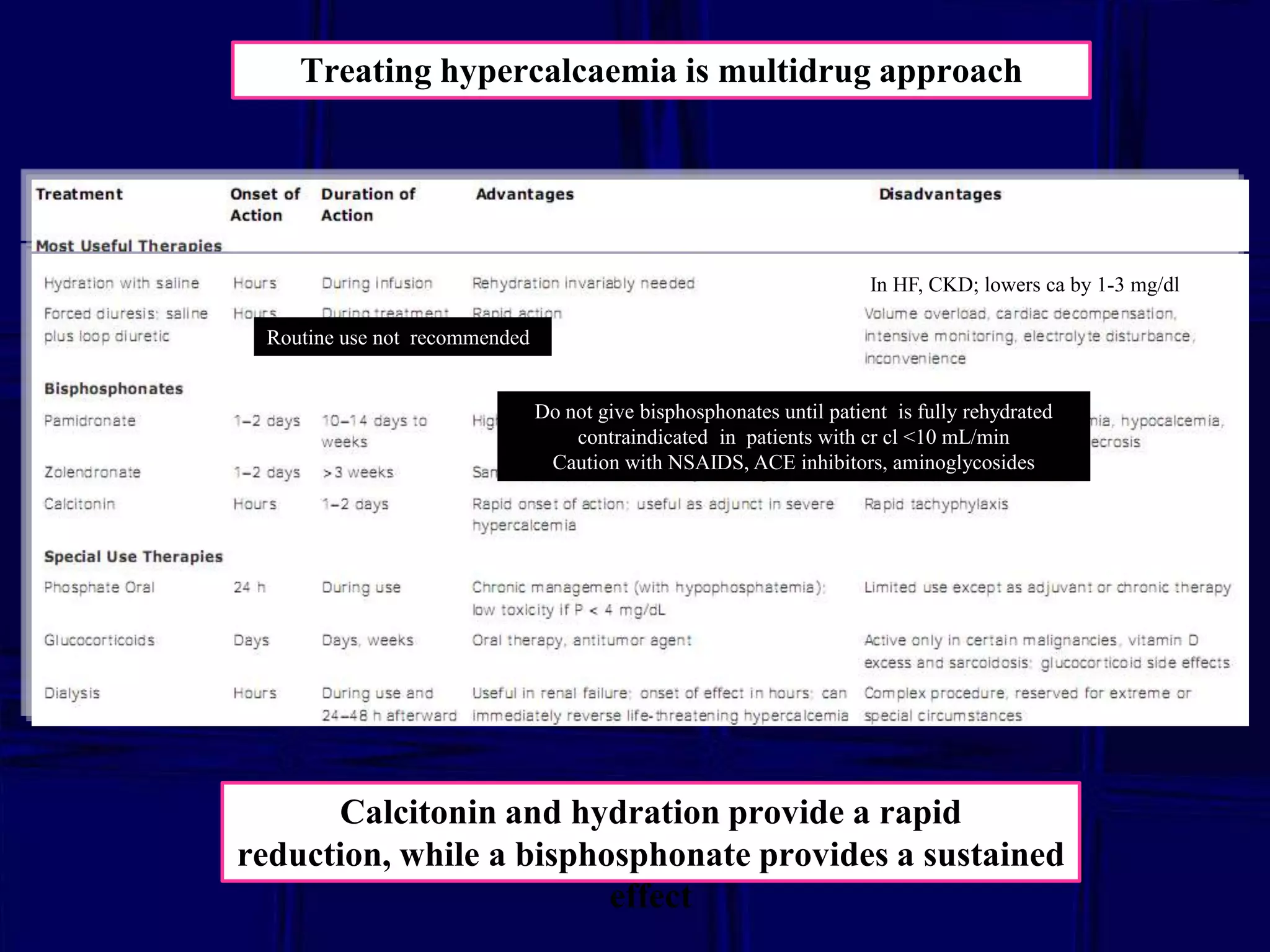
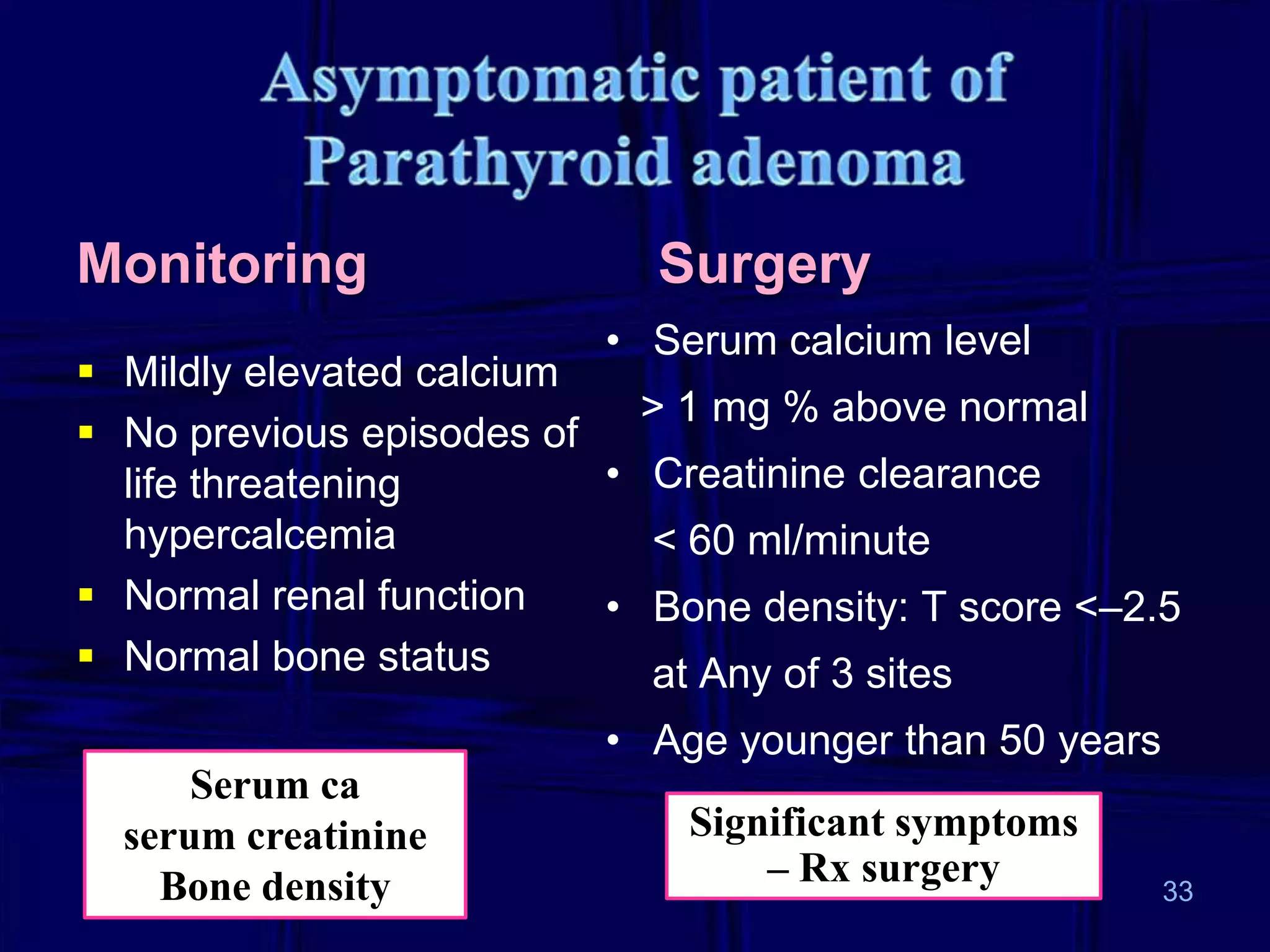
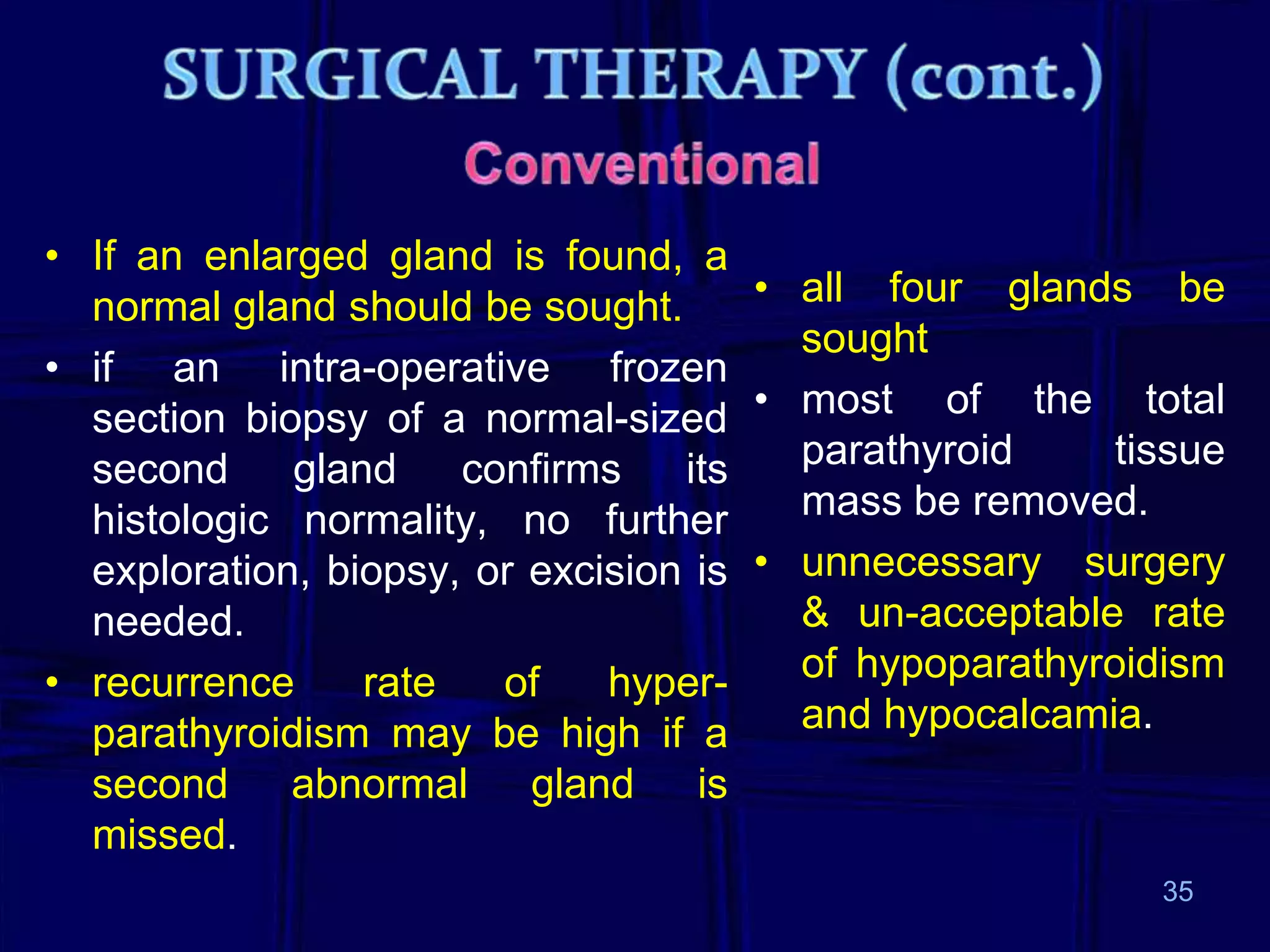
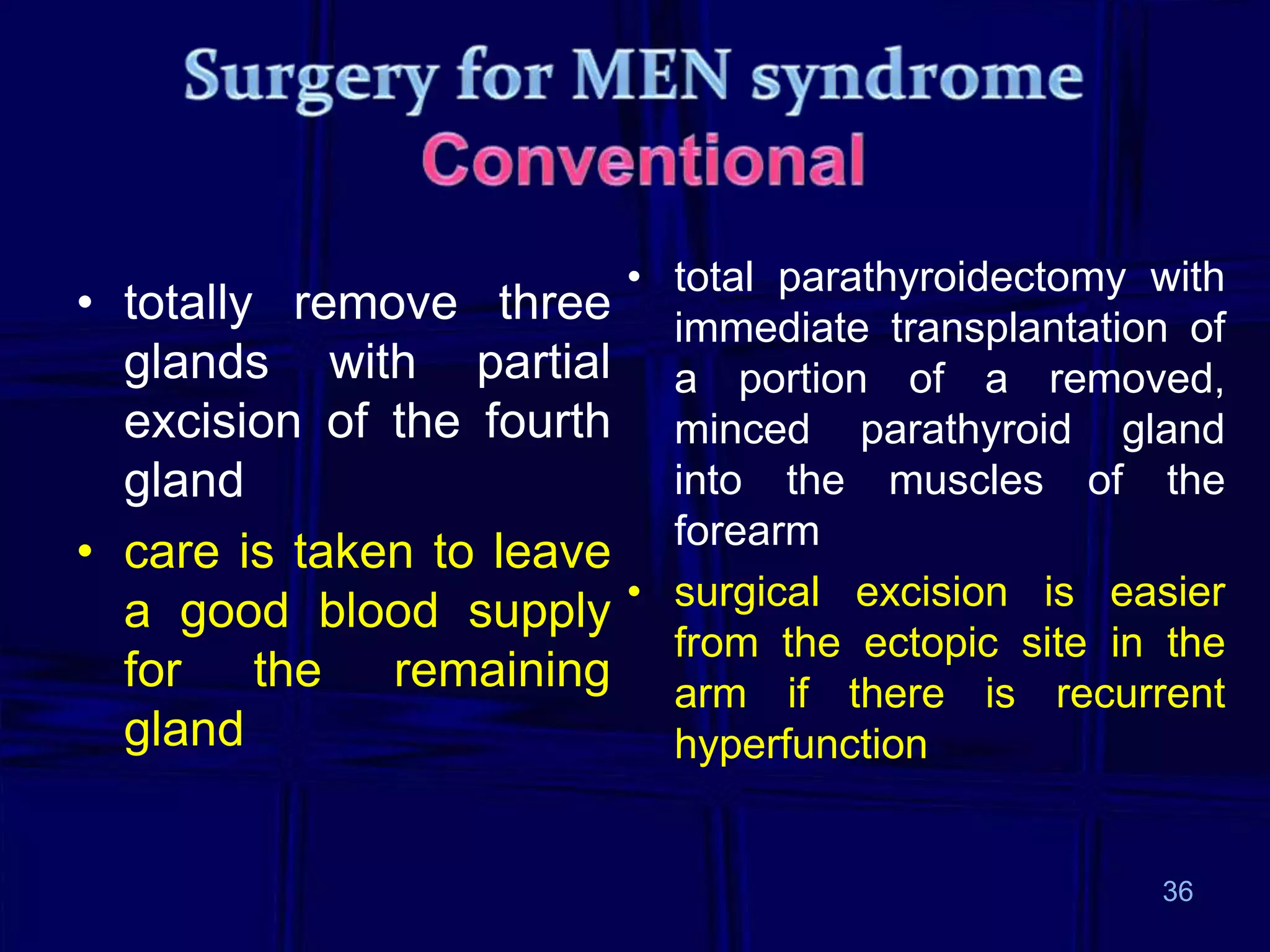
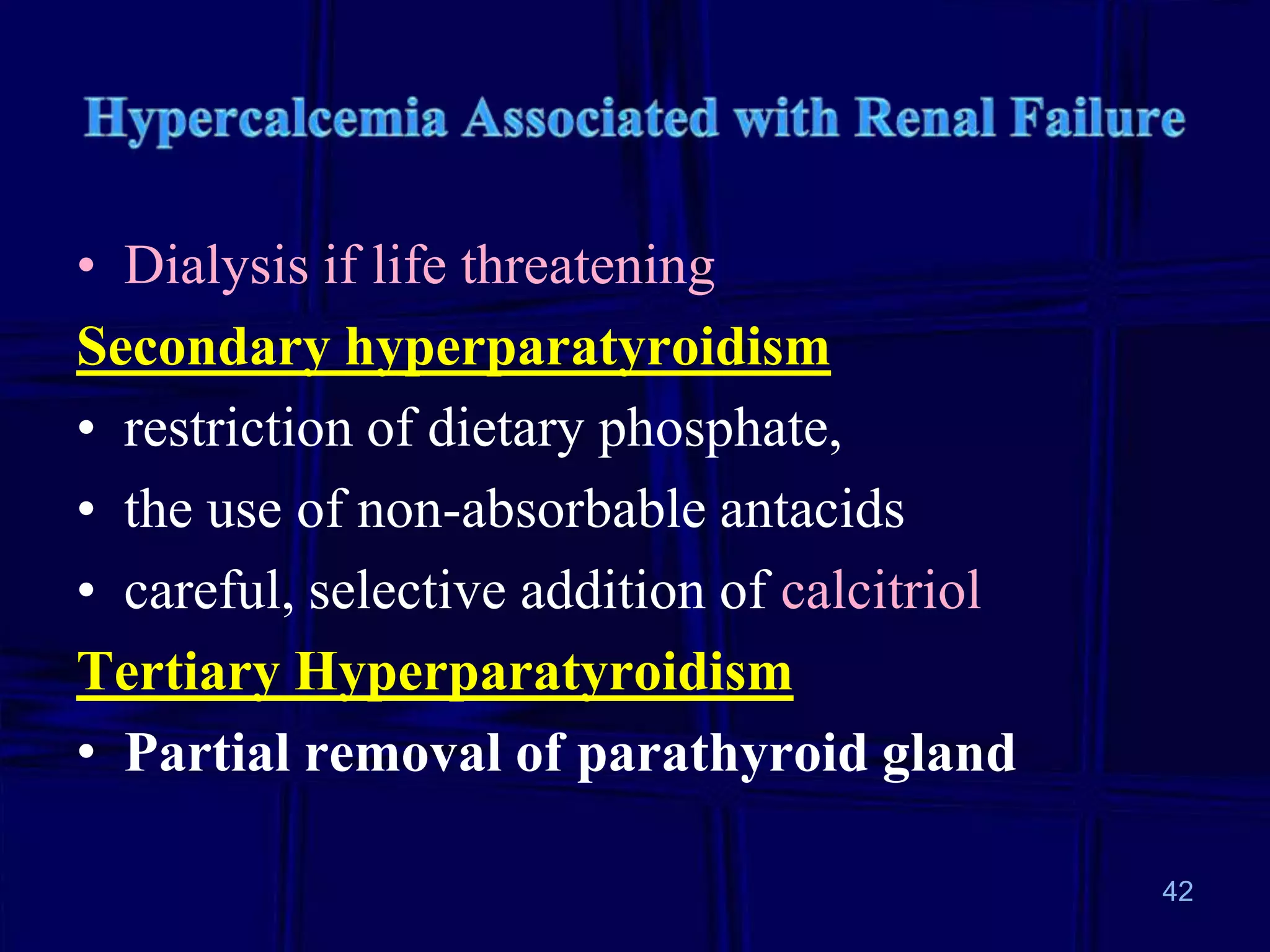
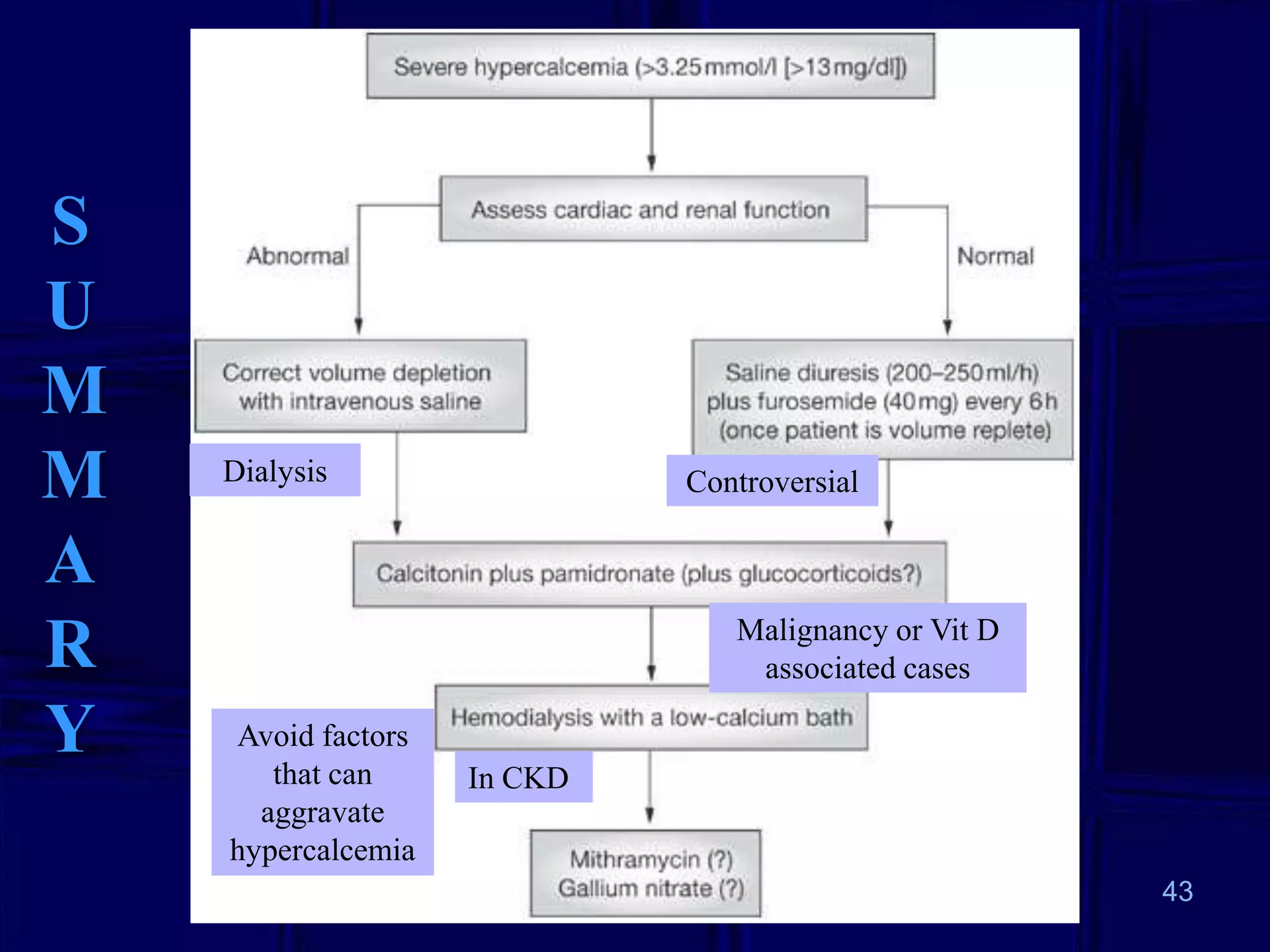
3. Treatment depends on the underlying cause but often involves rehydration, medications like bisphosphonates or calcitonin for acute reduction, and surgery for conditions like parathyroid adenoma causing primary hyperparathyroidism. Management seeks to address the cause and lower calcium levels to avoid complications.