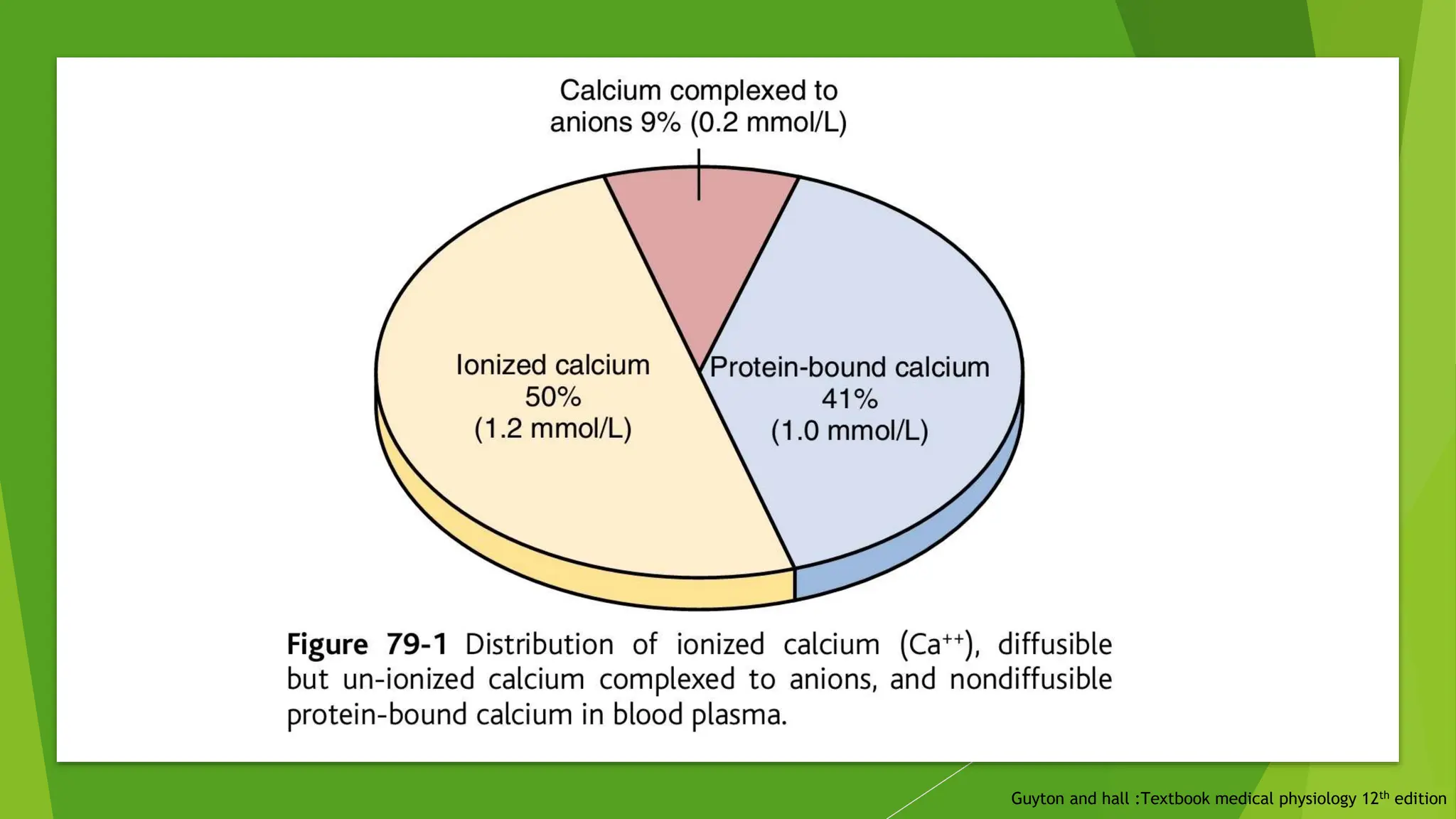
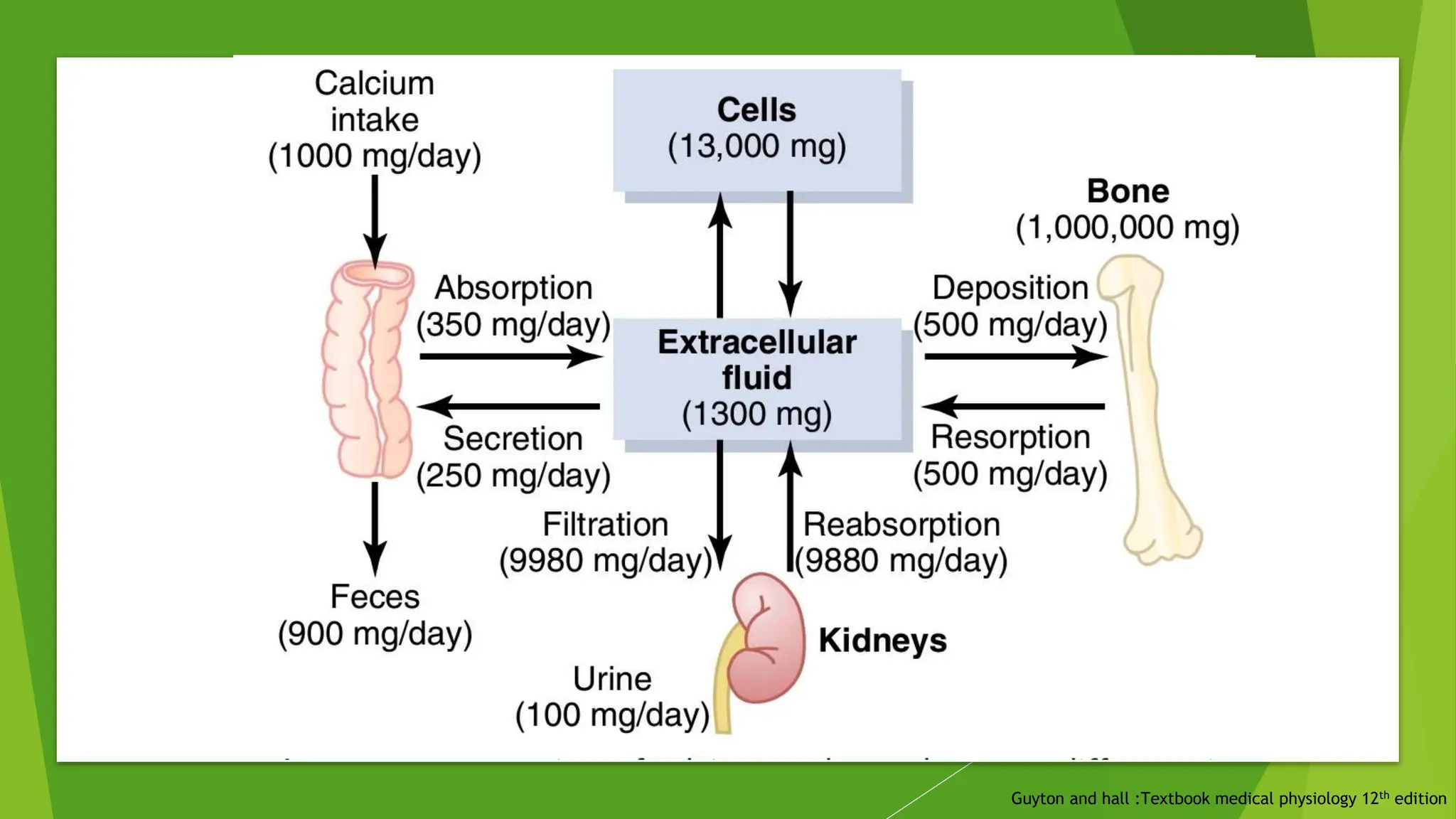
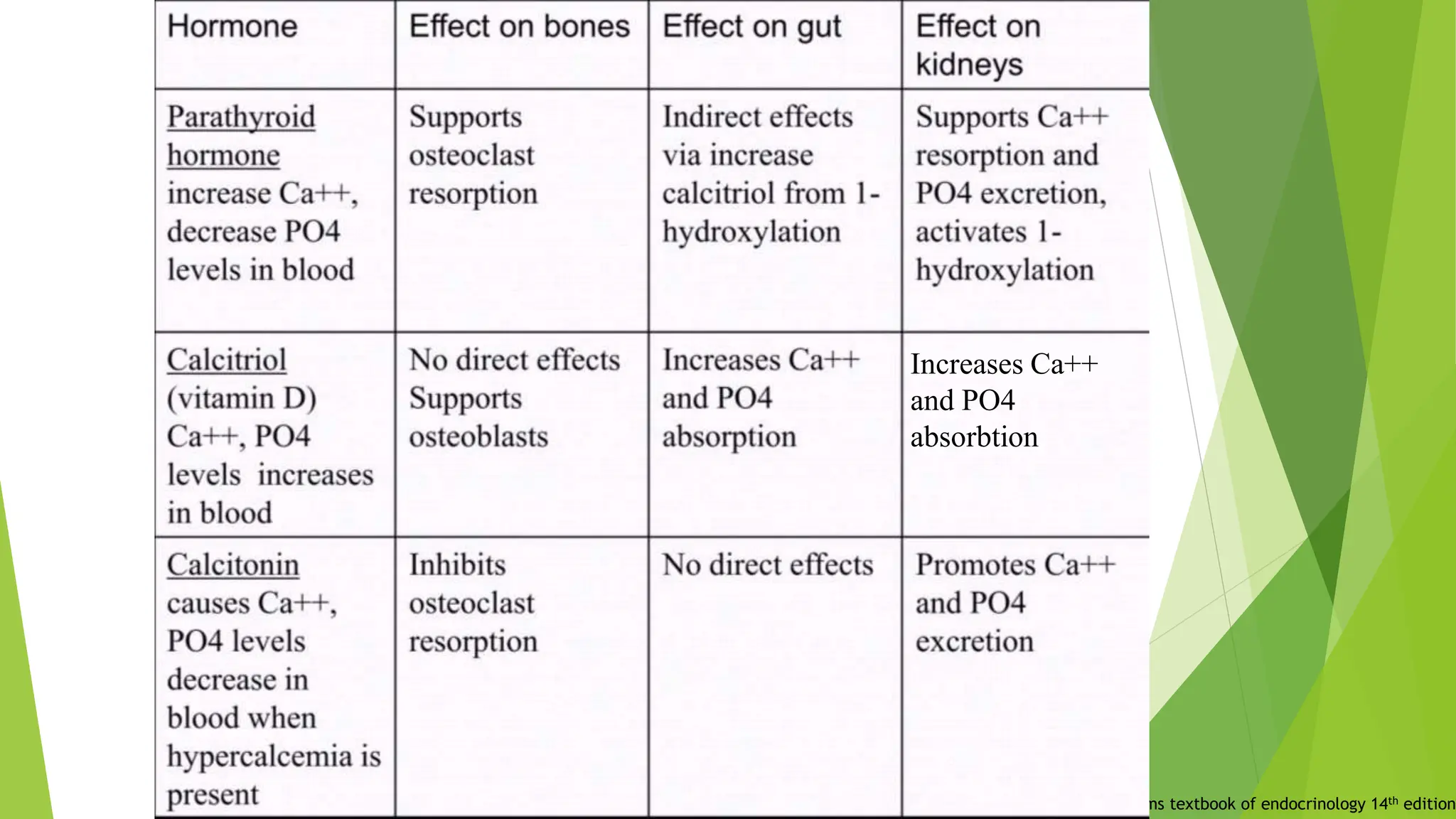
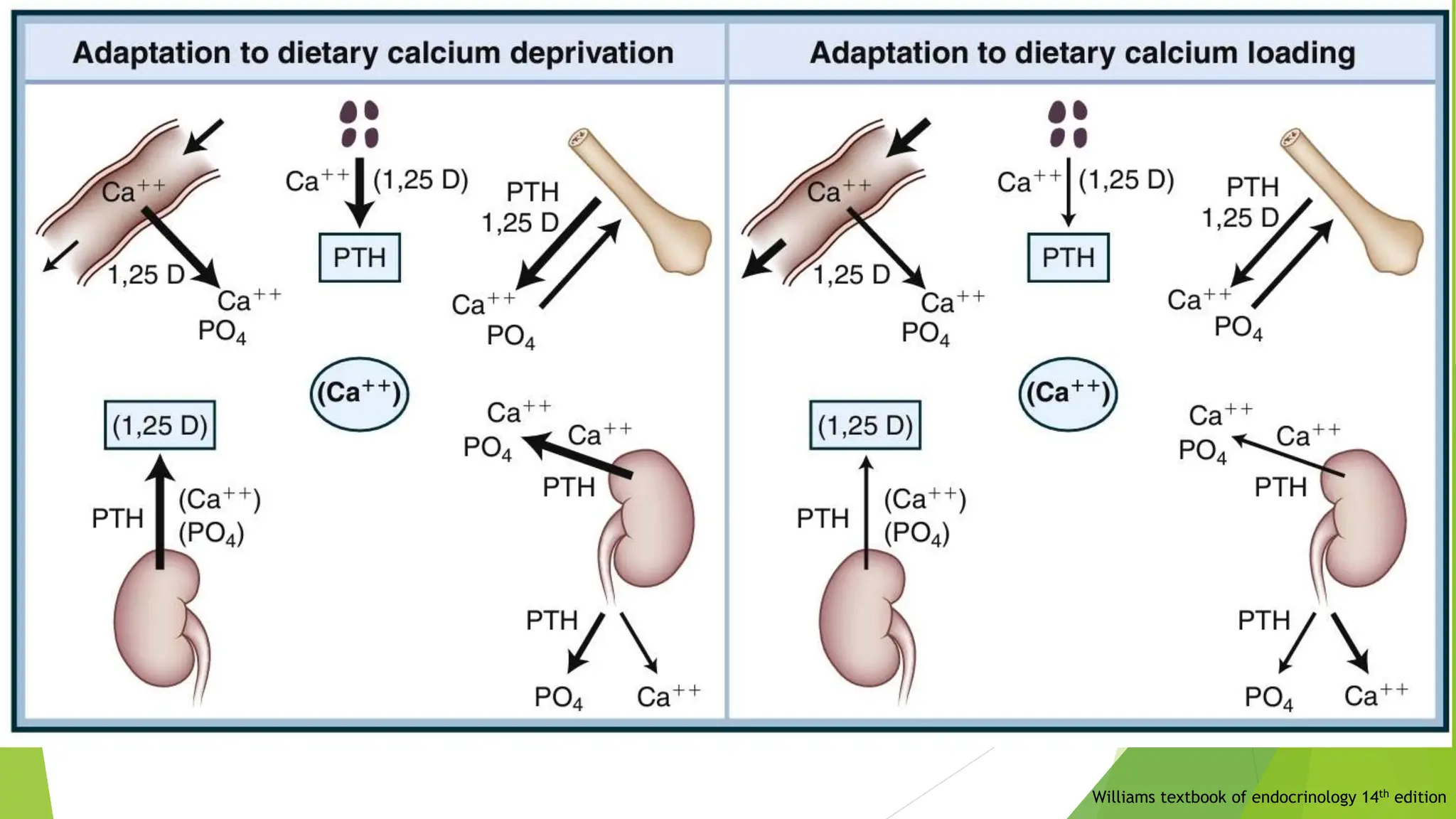
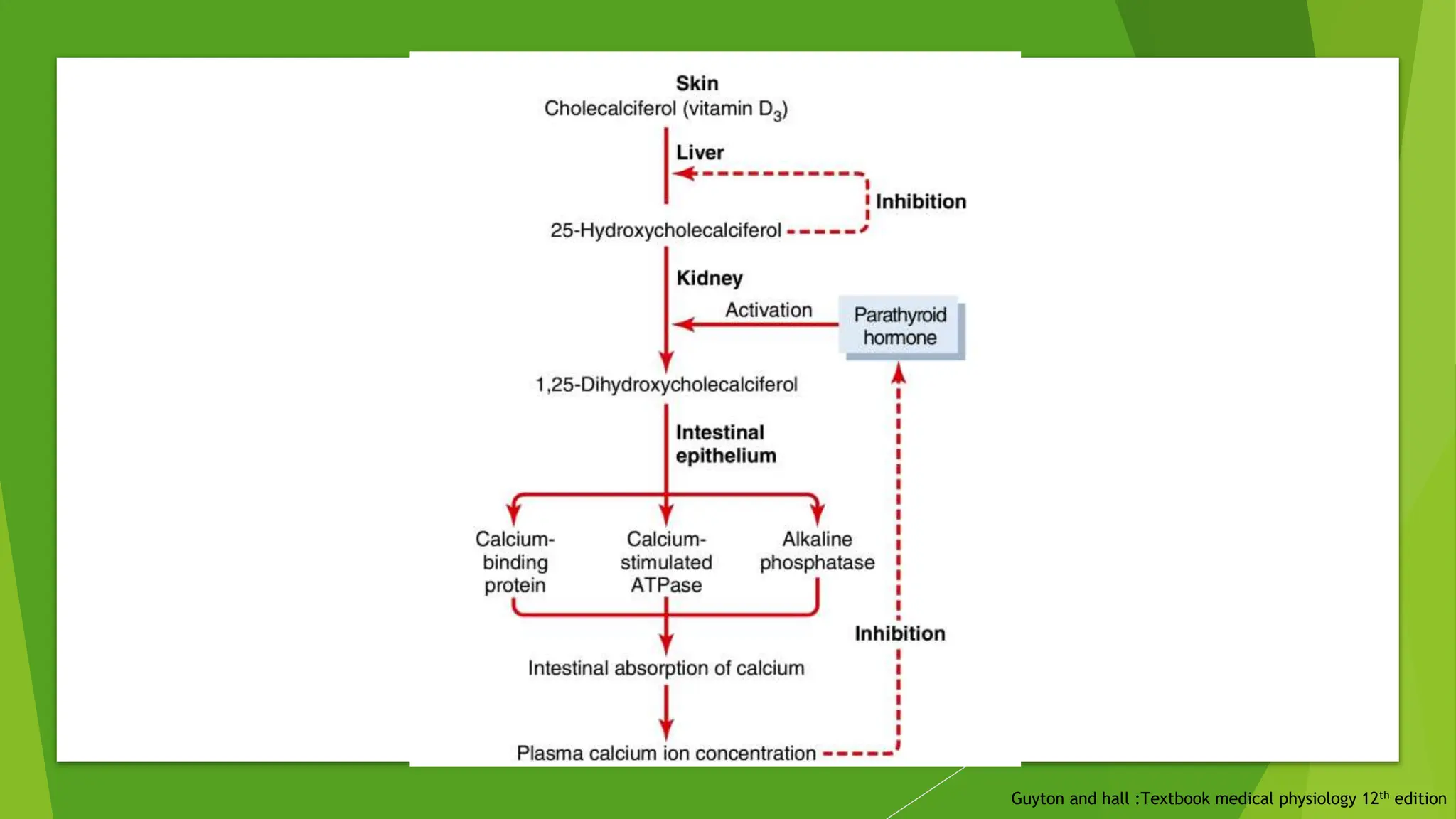
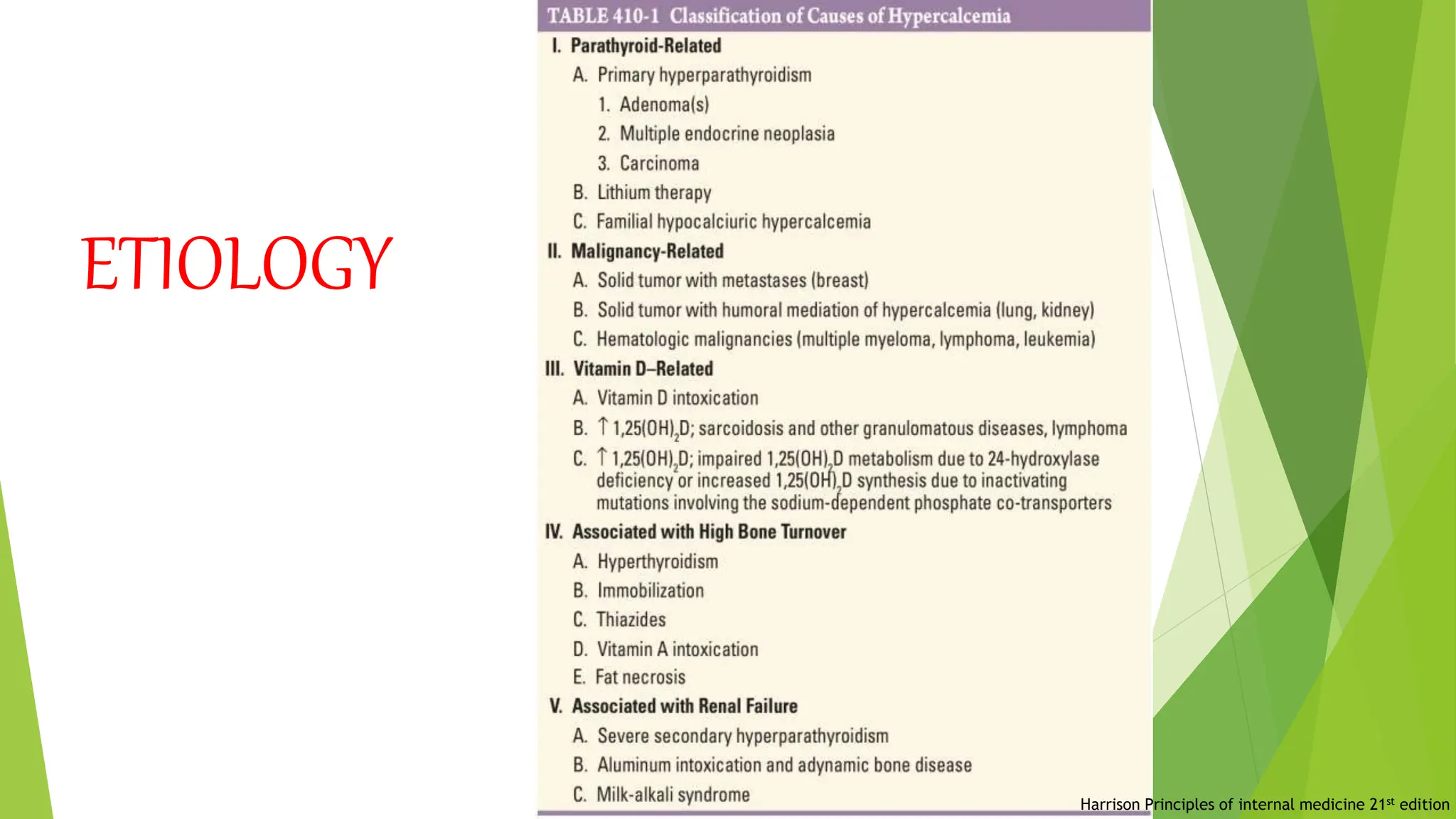
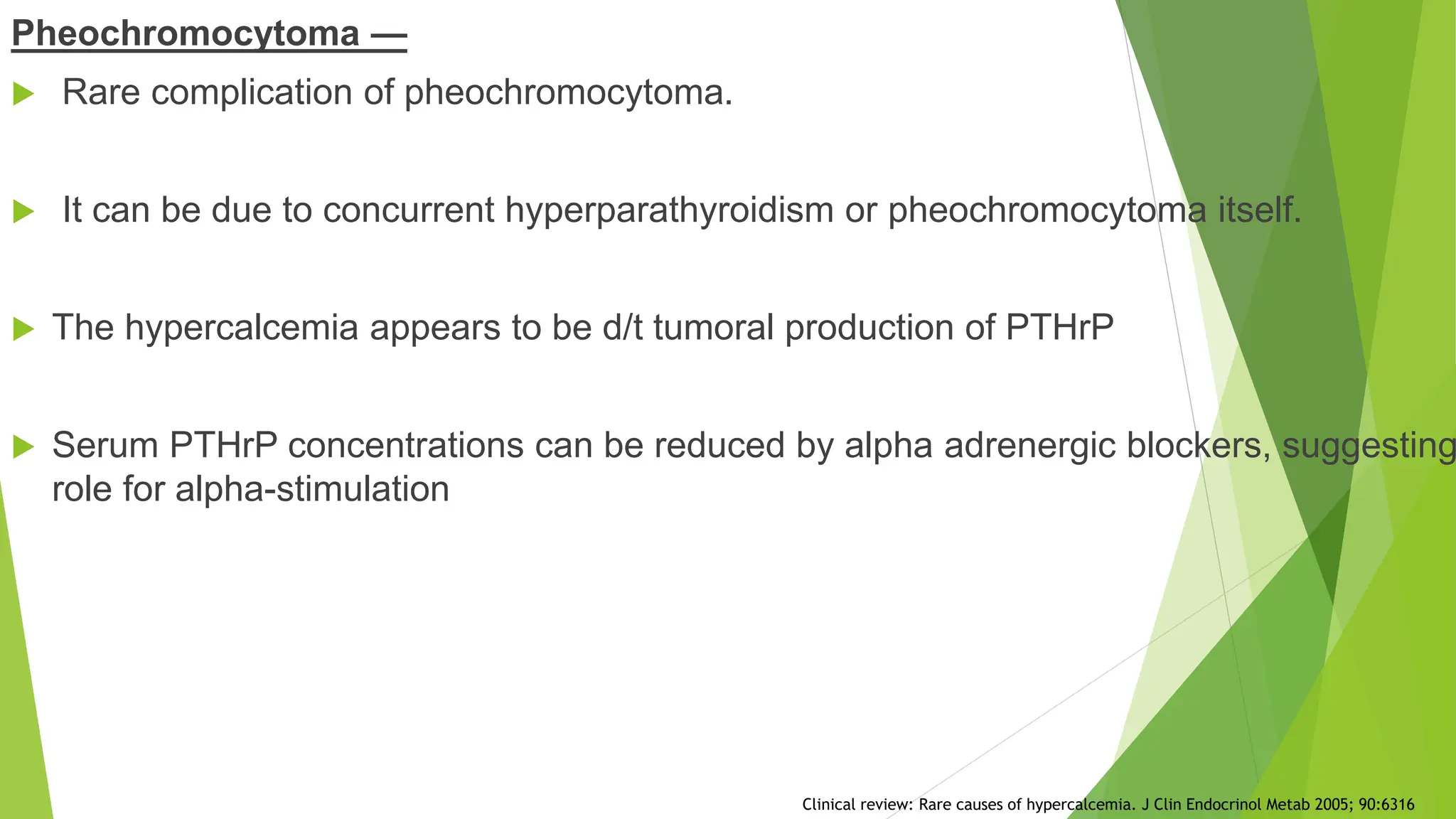
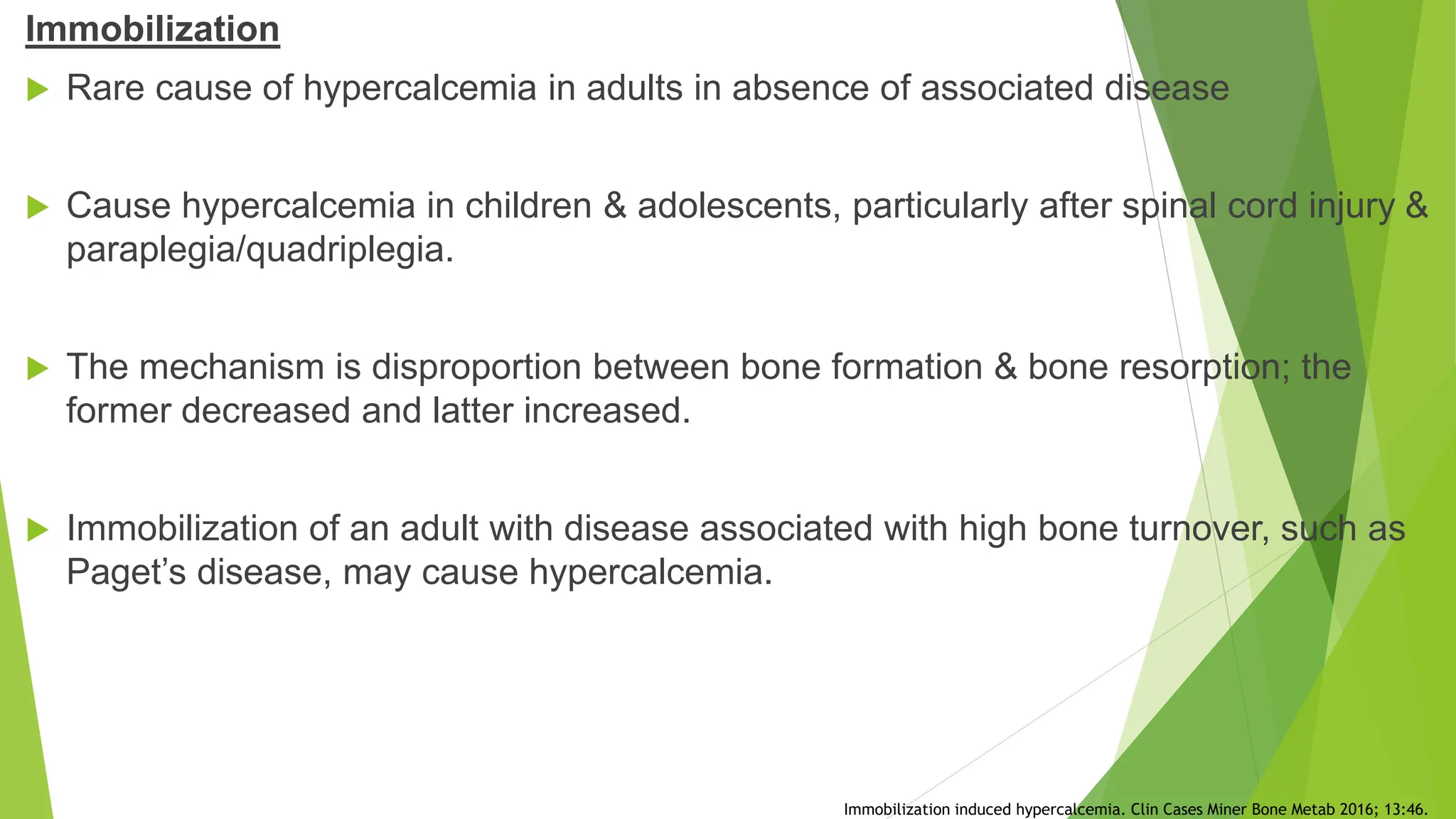
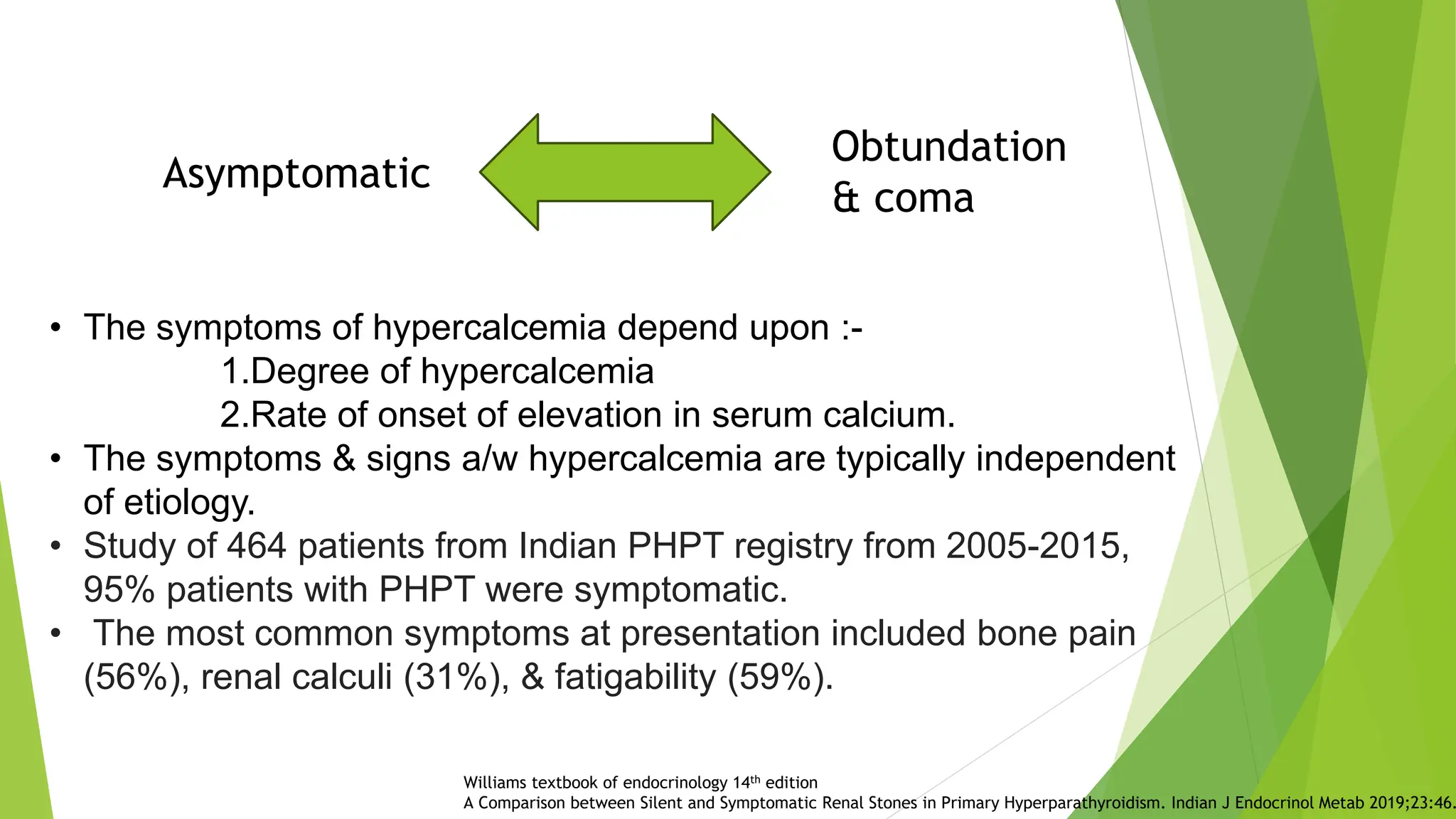
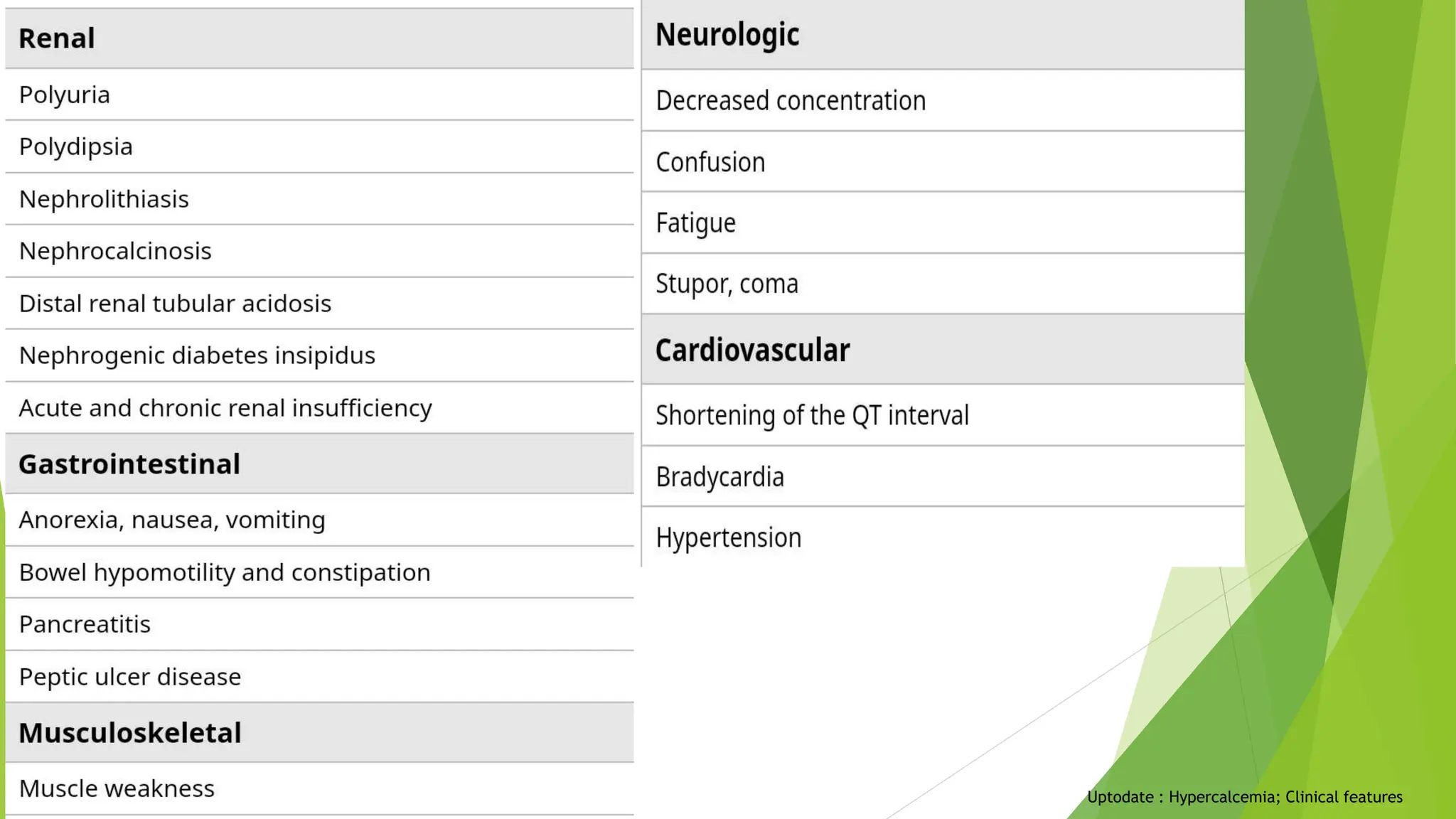
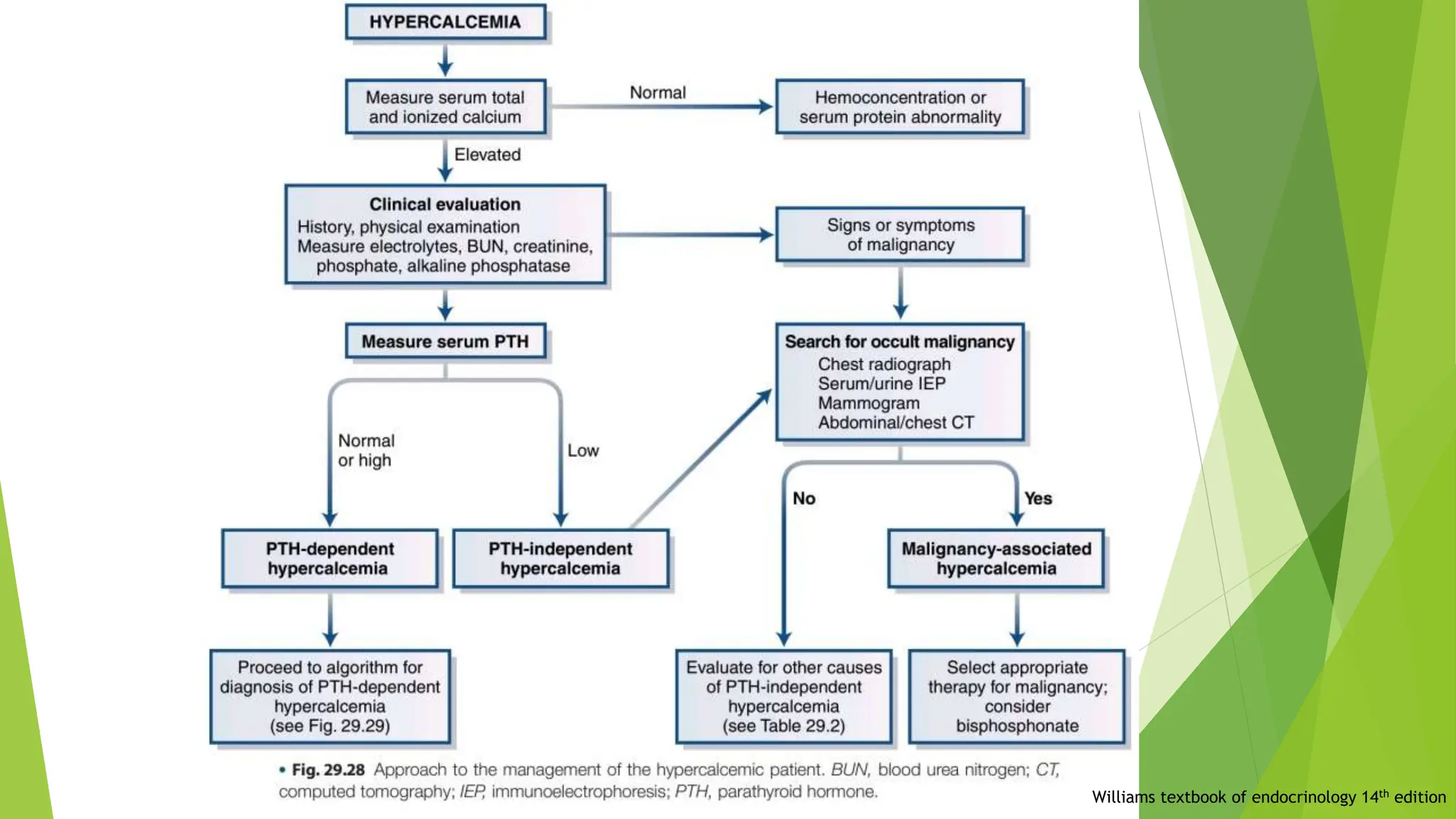
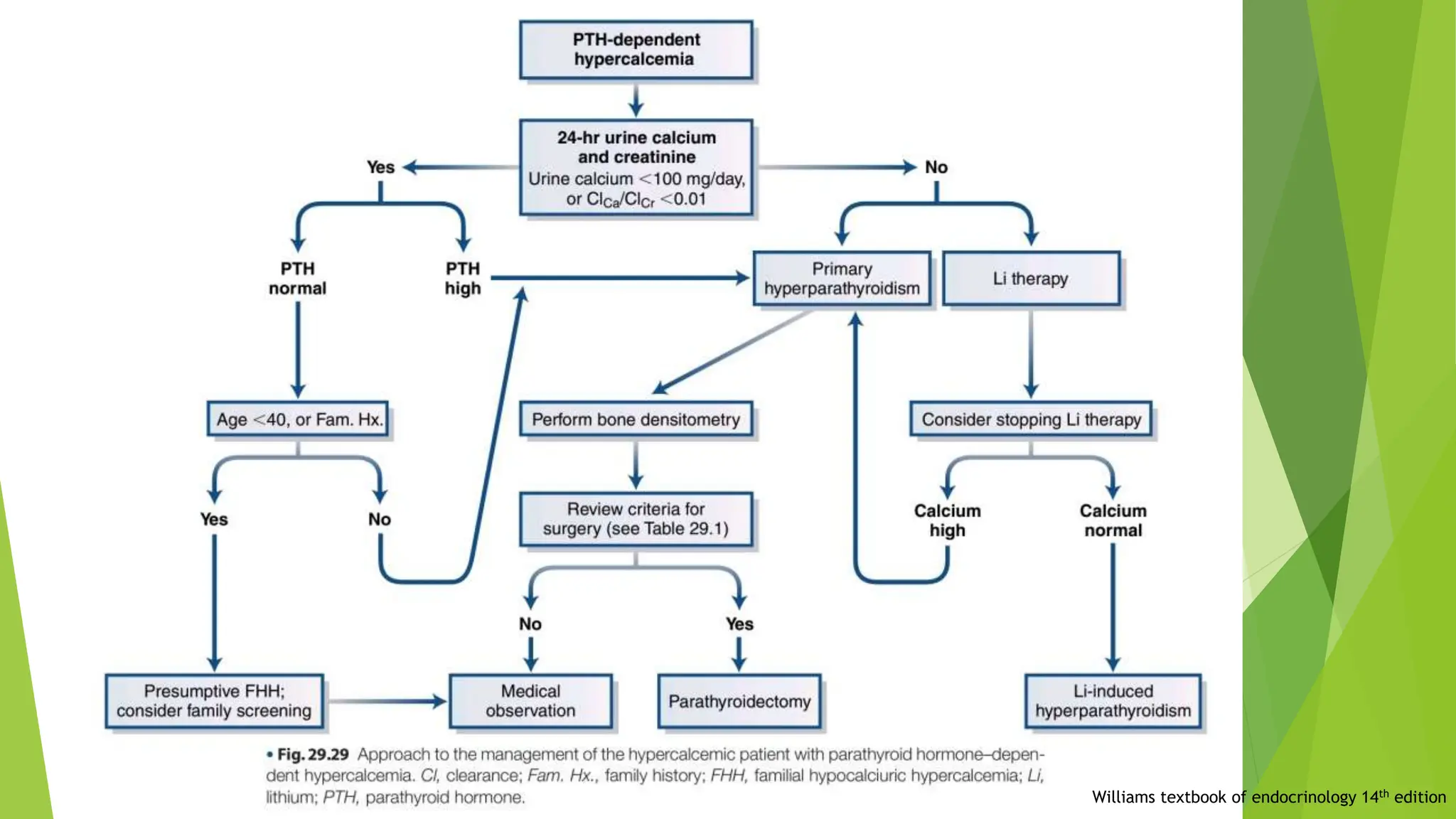
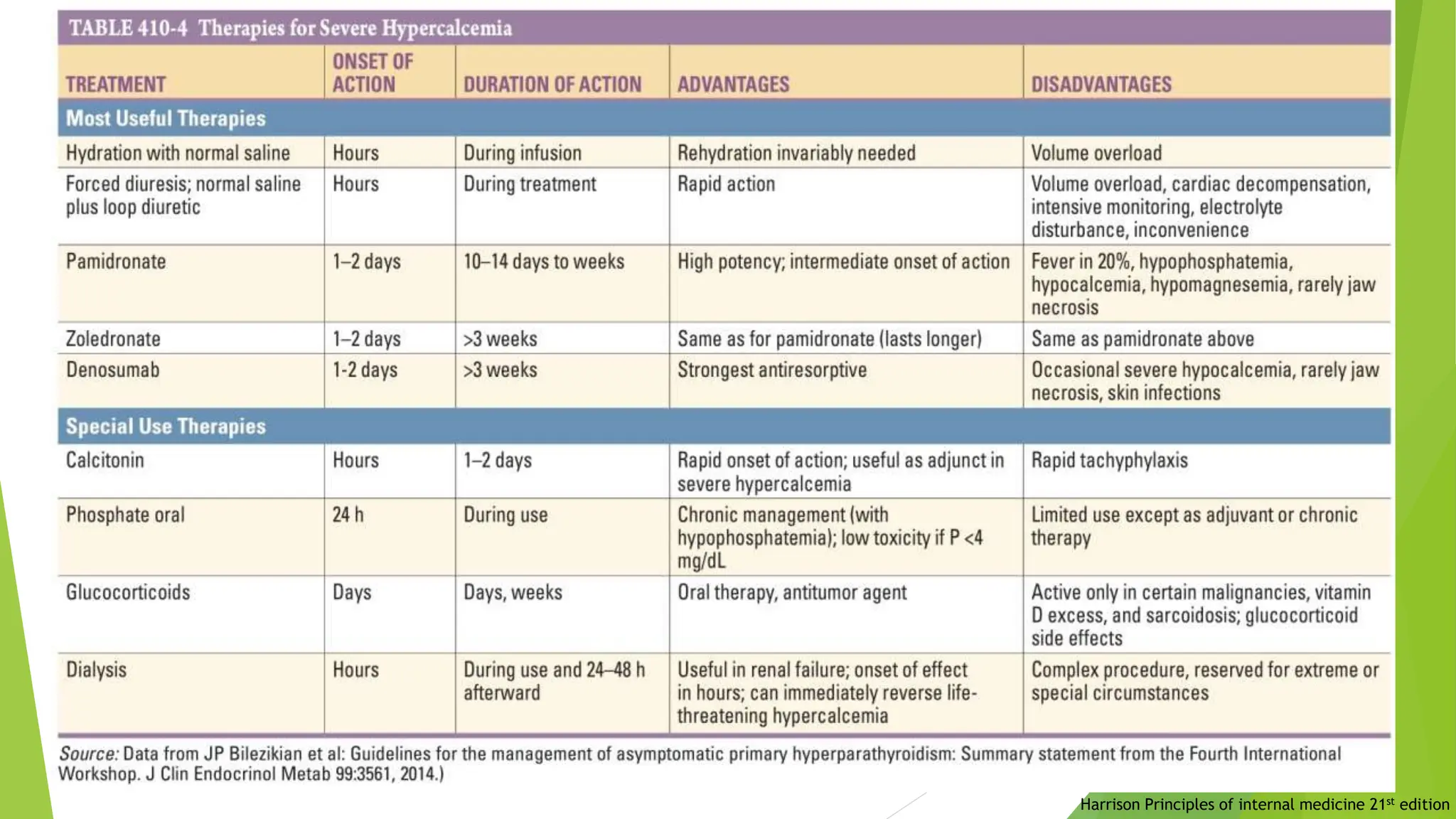
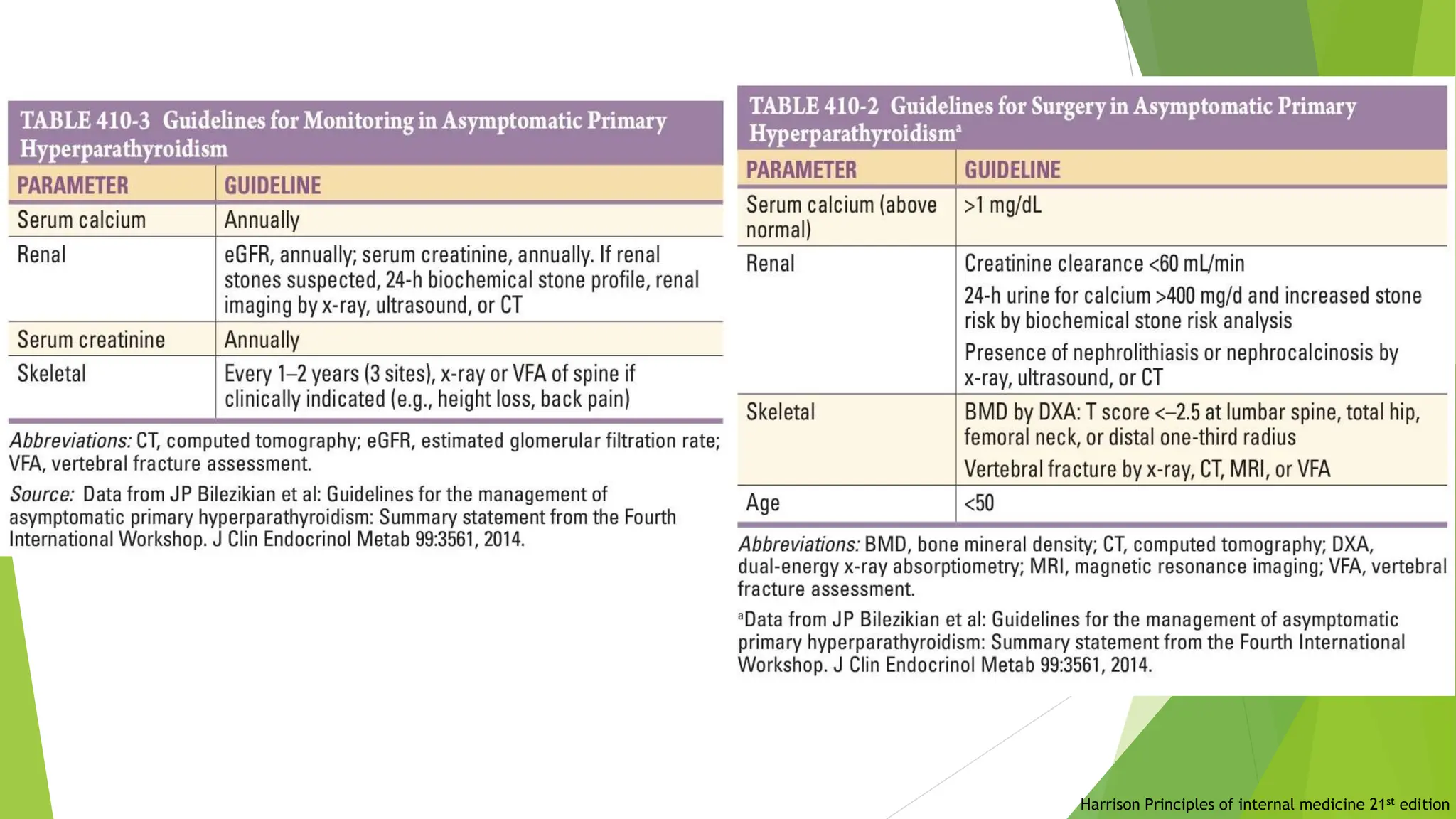
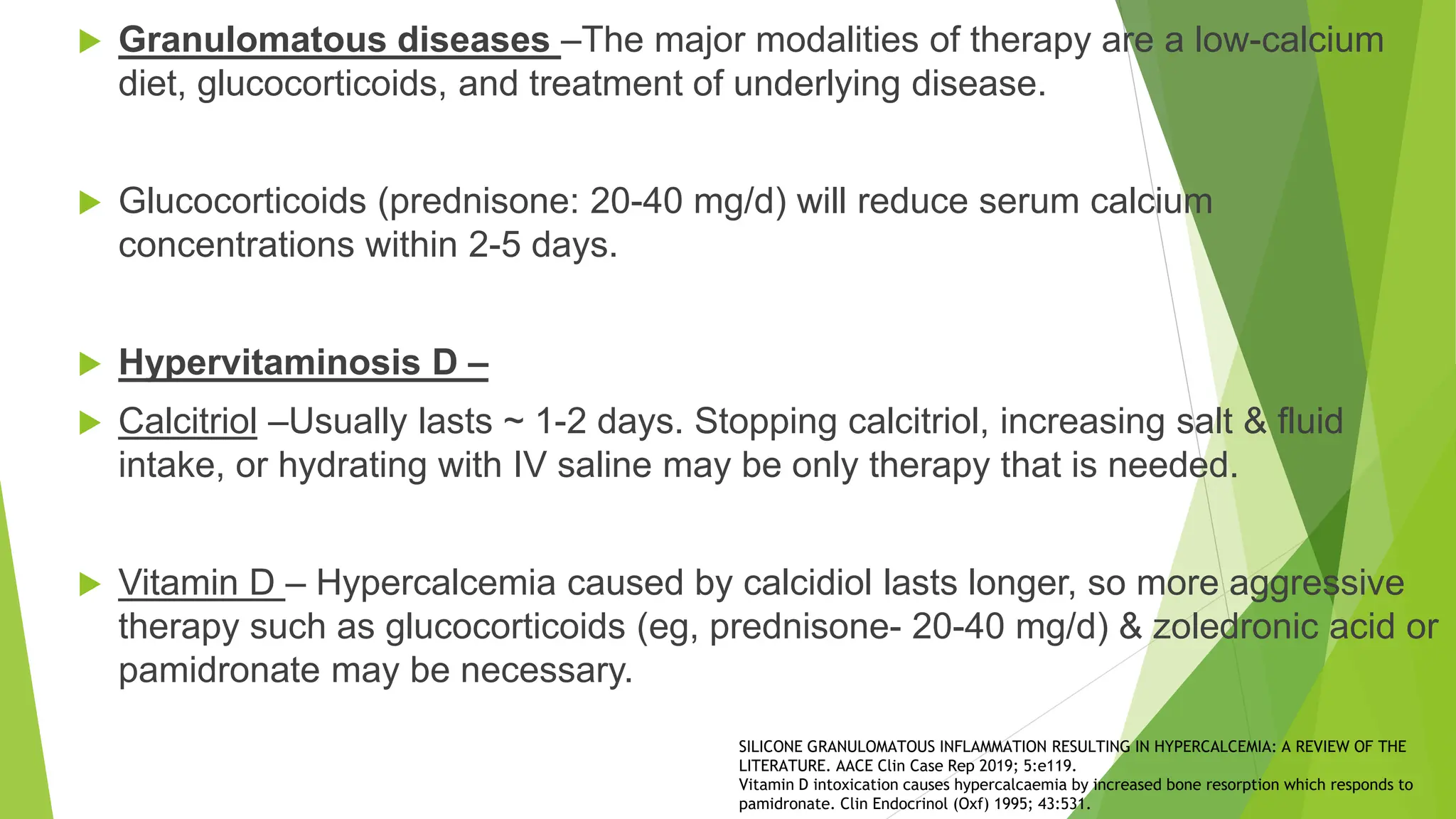
This document discusses hypercalcemia, its causes, clinical features, and management strategies. It highlights the role of calcium in physiological functions, common etiologies like primary hyperparathyroidism and malignancy, and various treatment options including hydration, medications, and surgical interventions. Additionally, it emphasizes the importance of evaluating symptoms and individual patient factors for effective treatment.