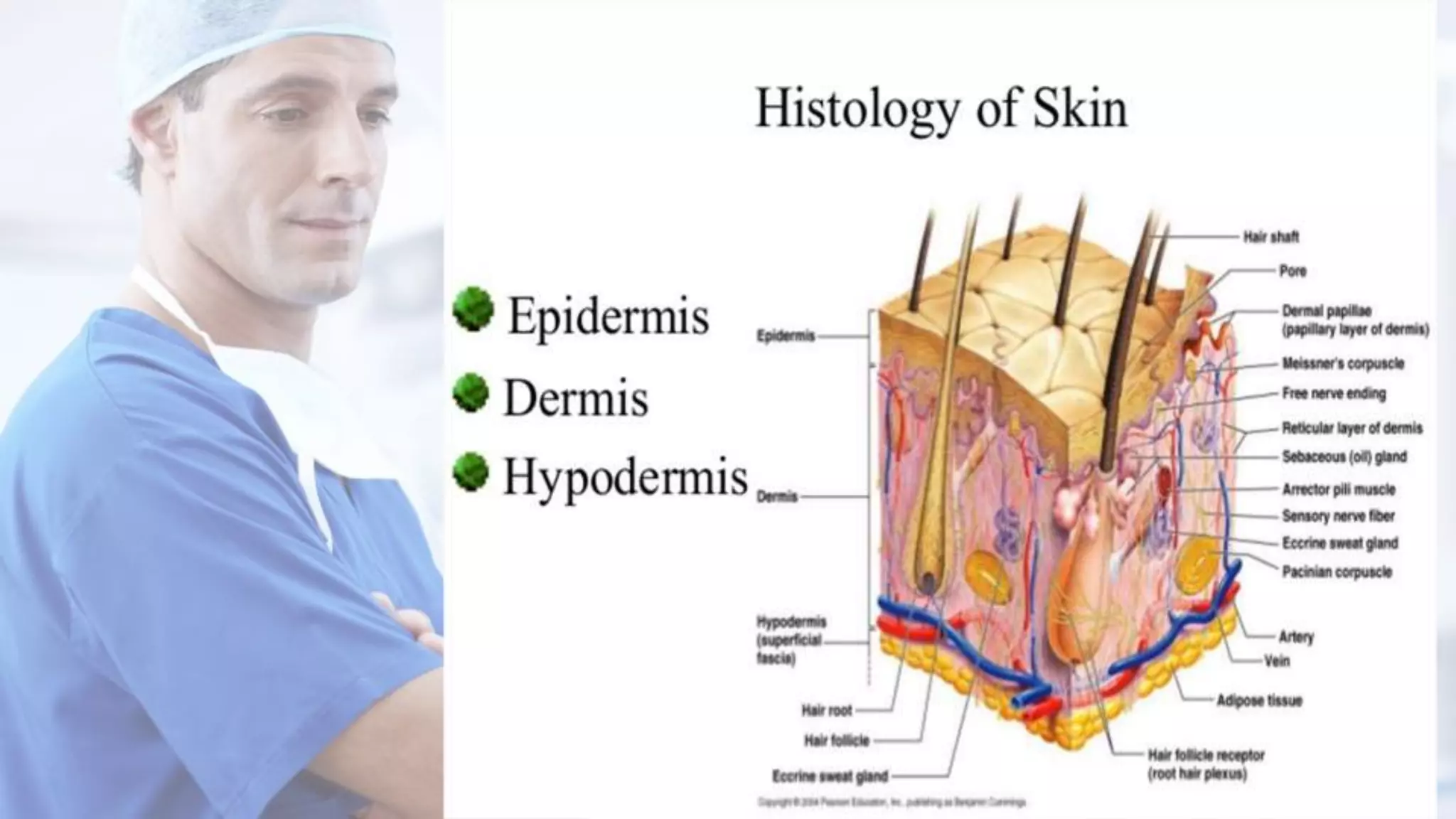
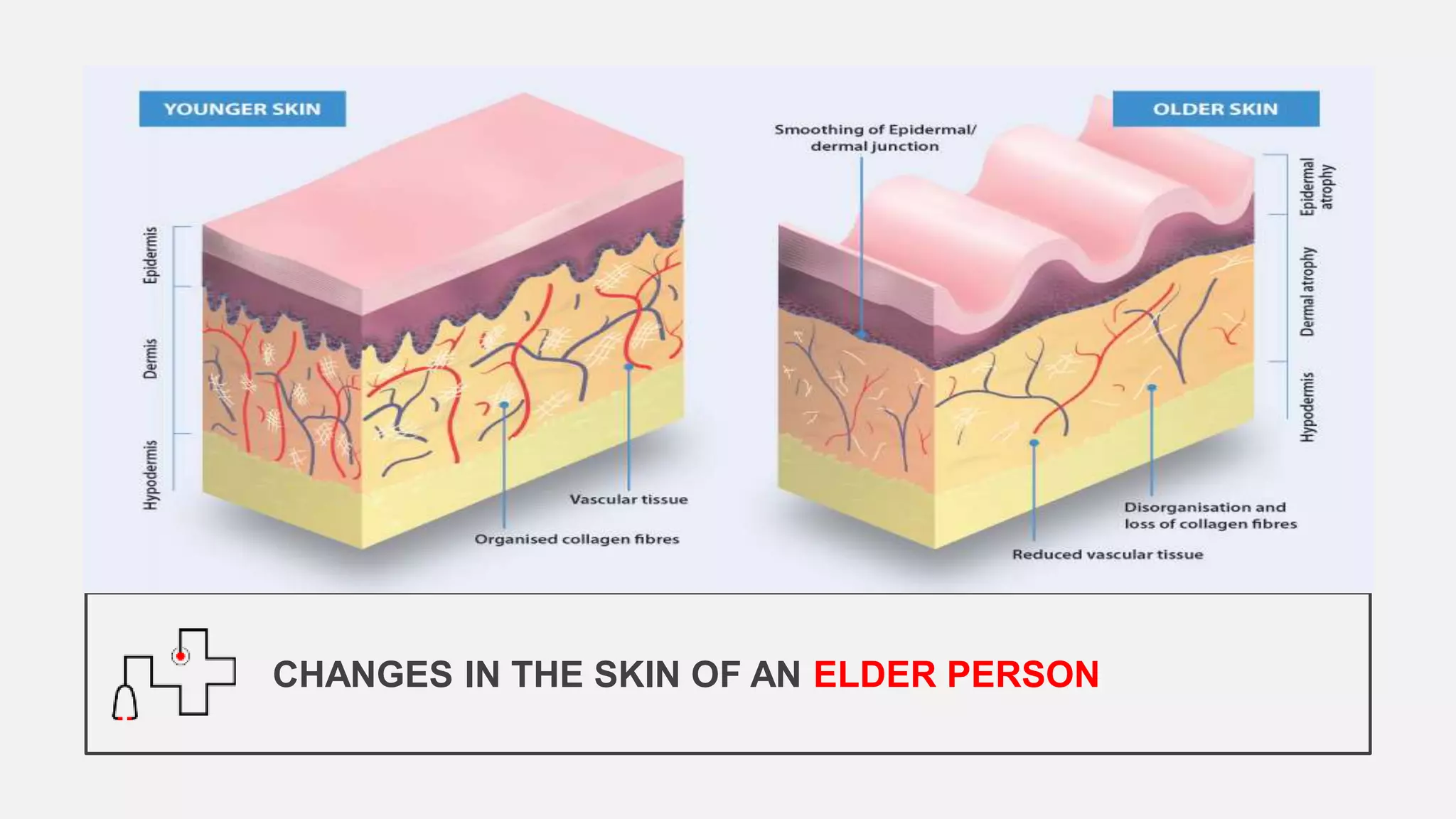
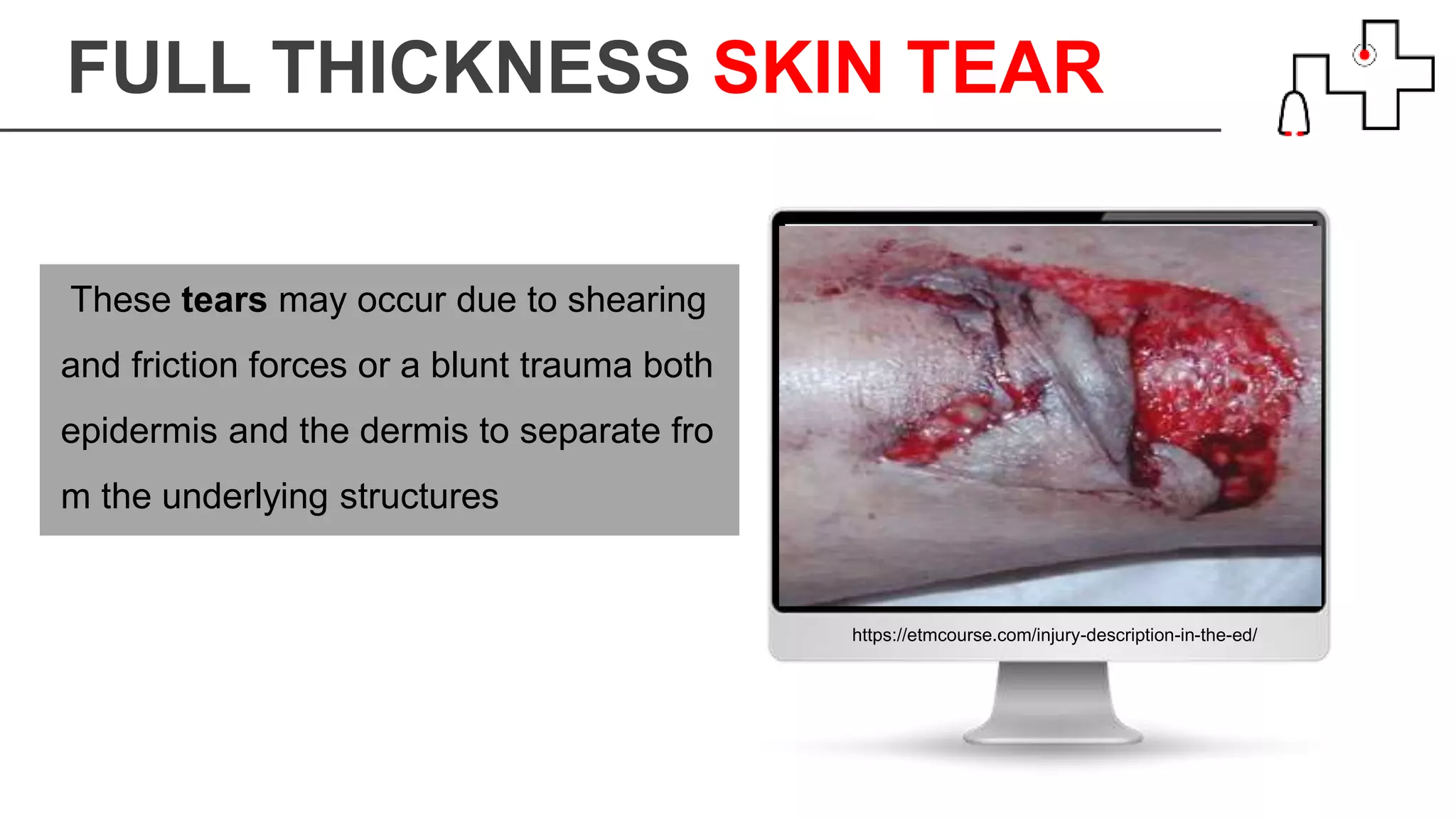
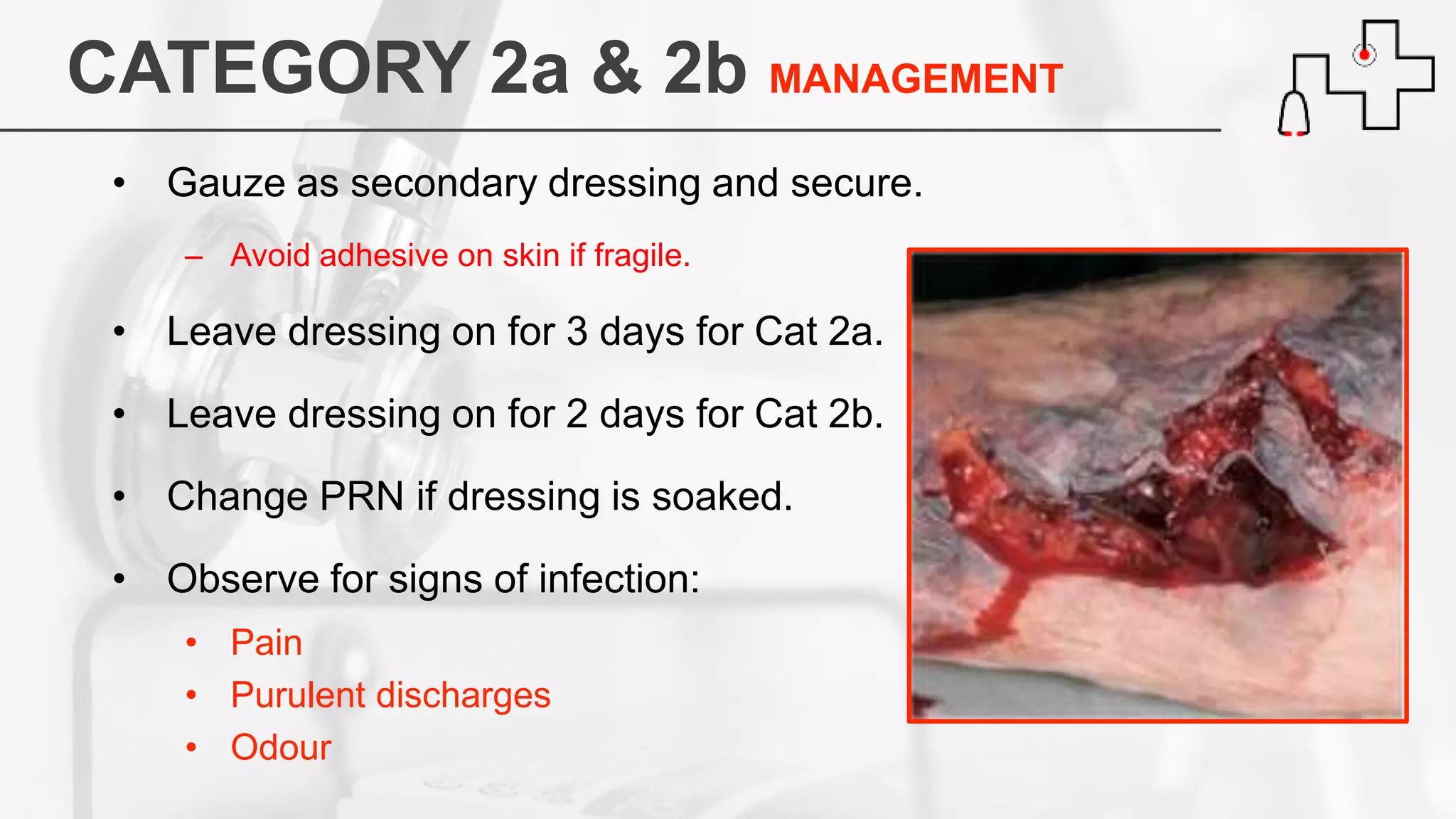
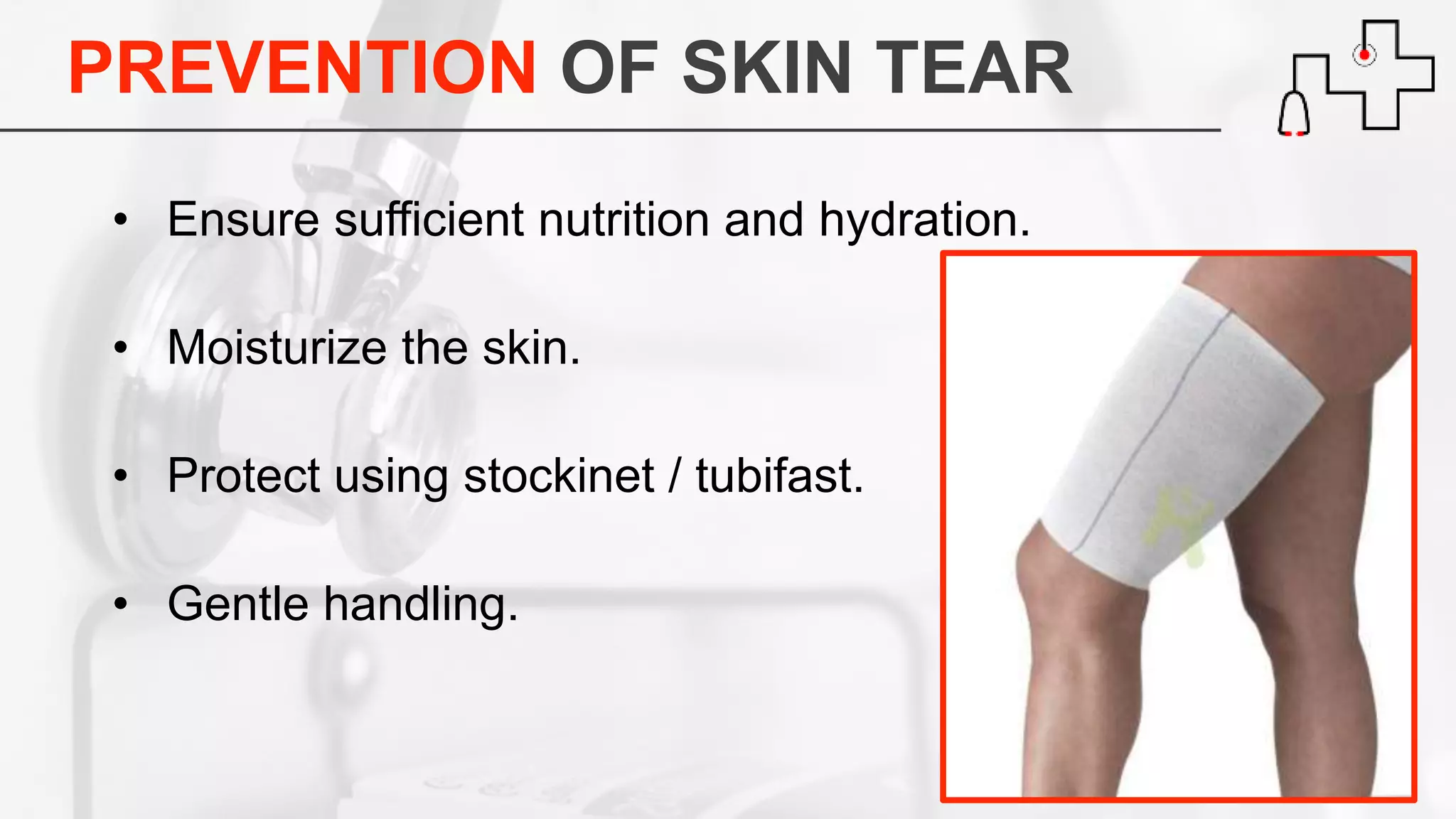
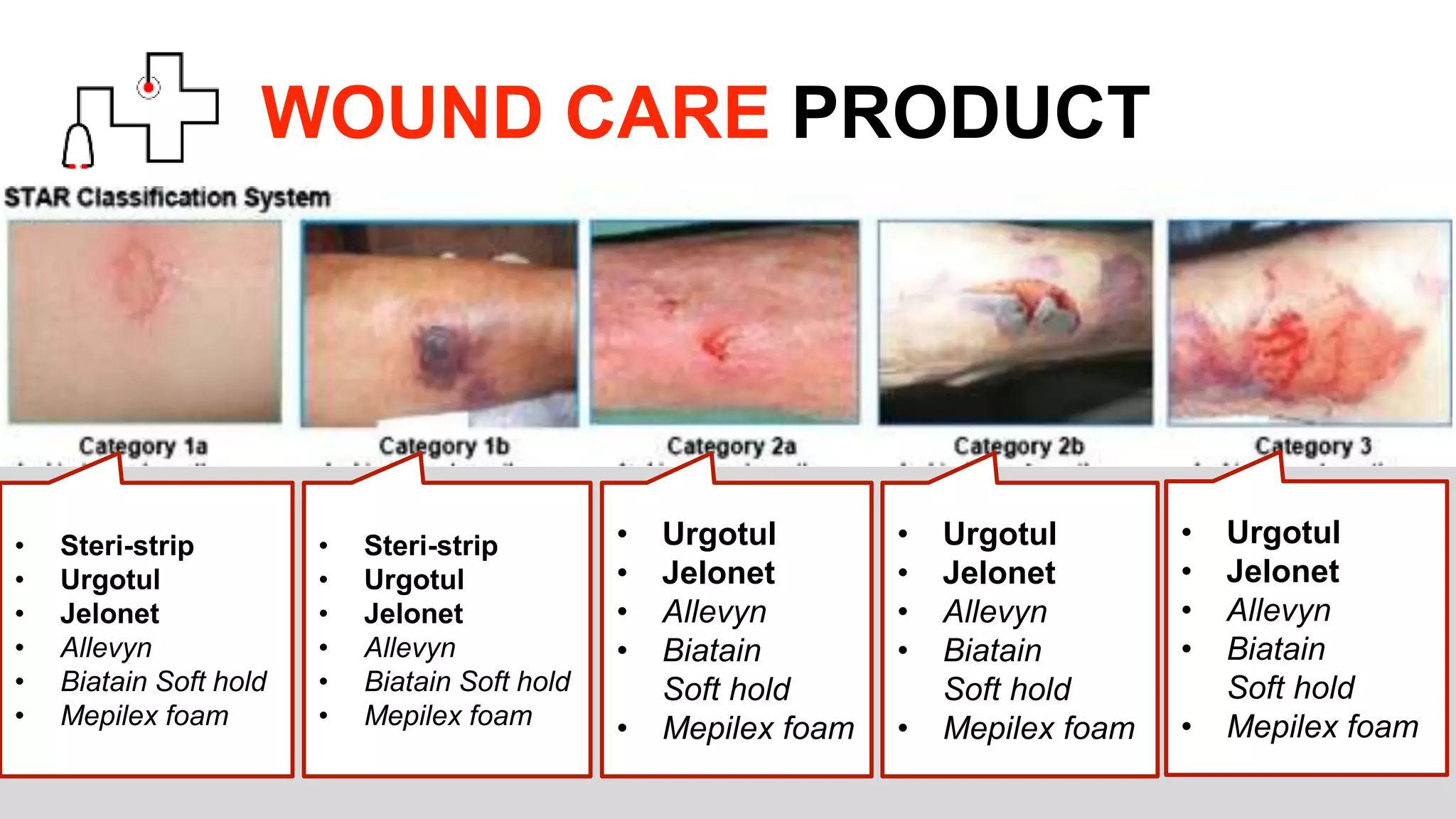
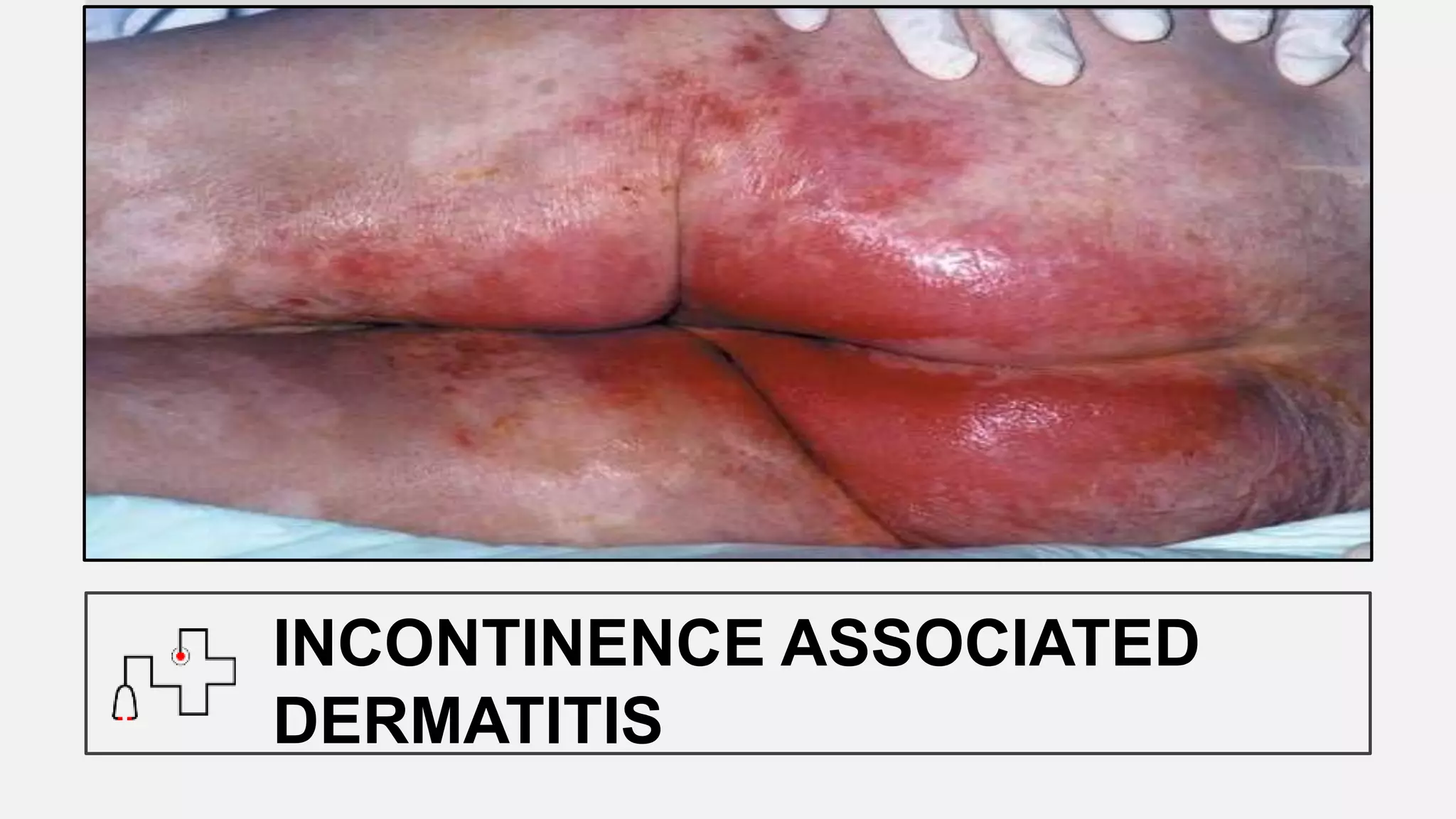
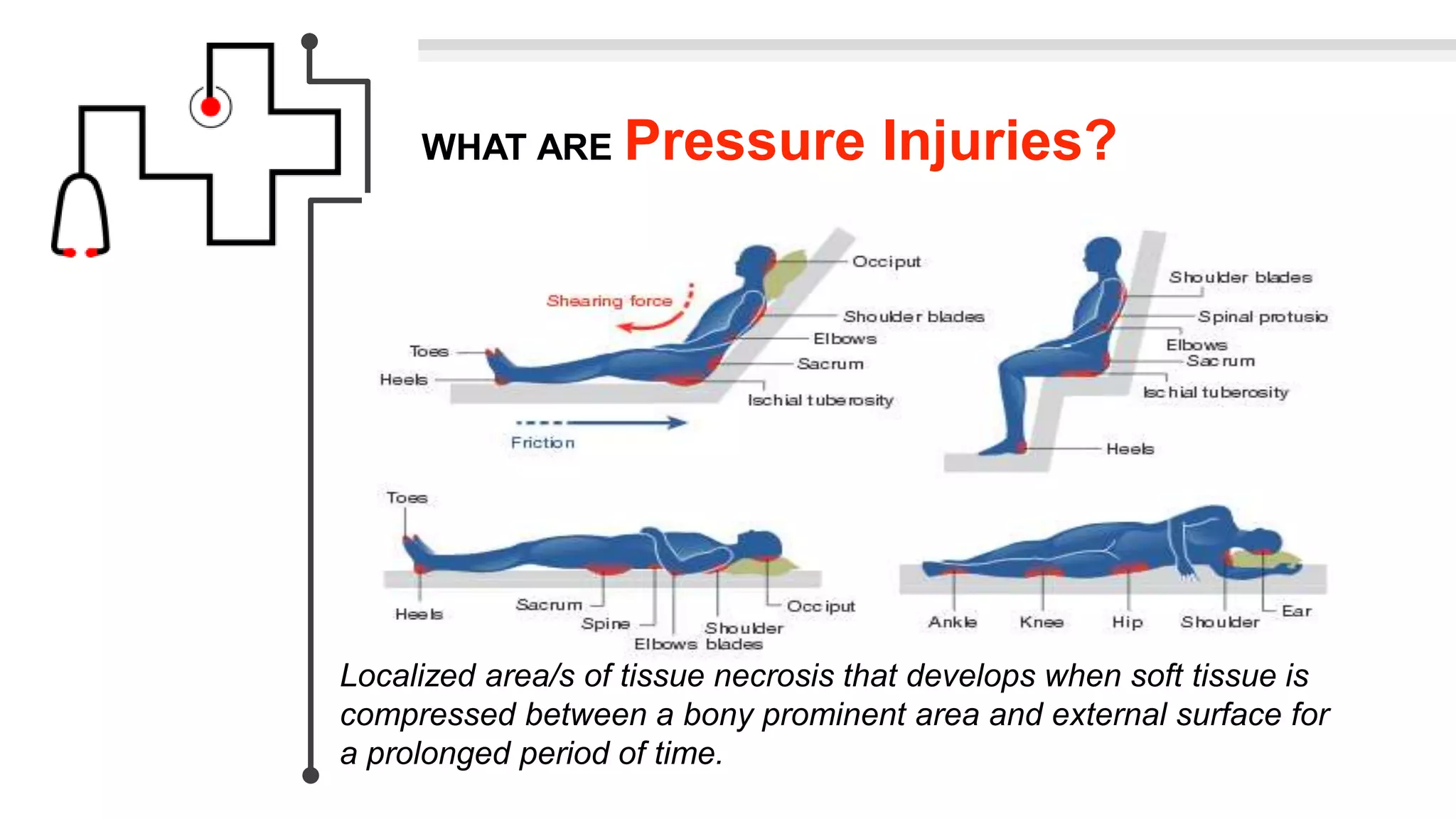
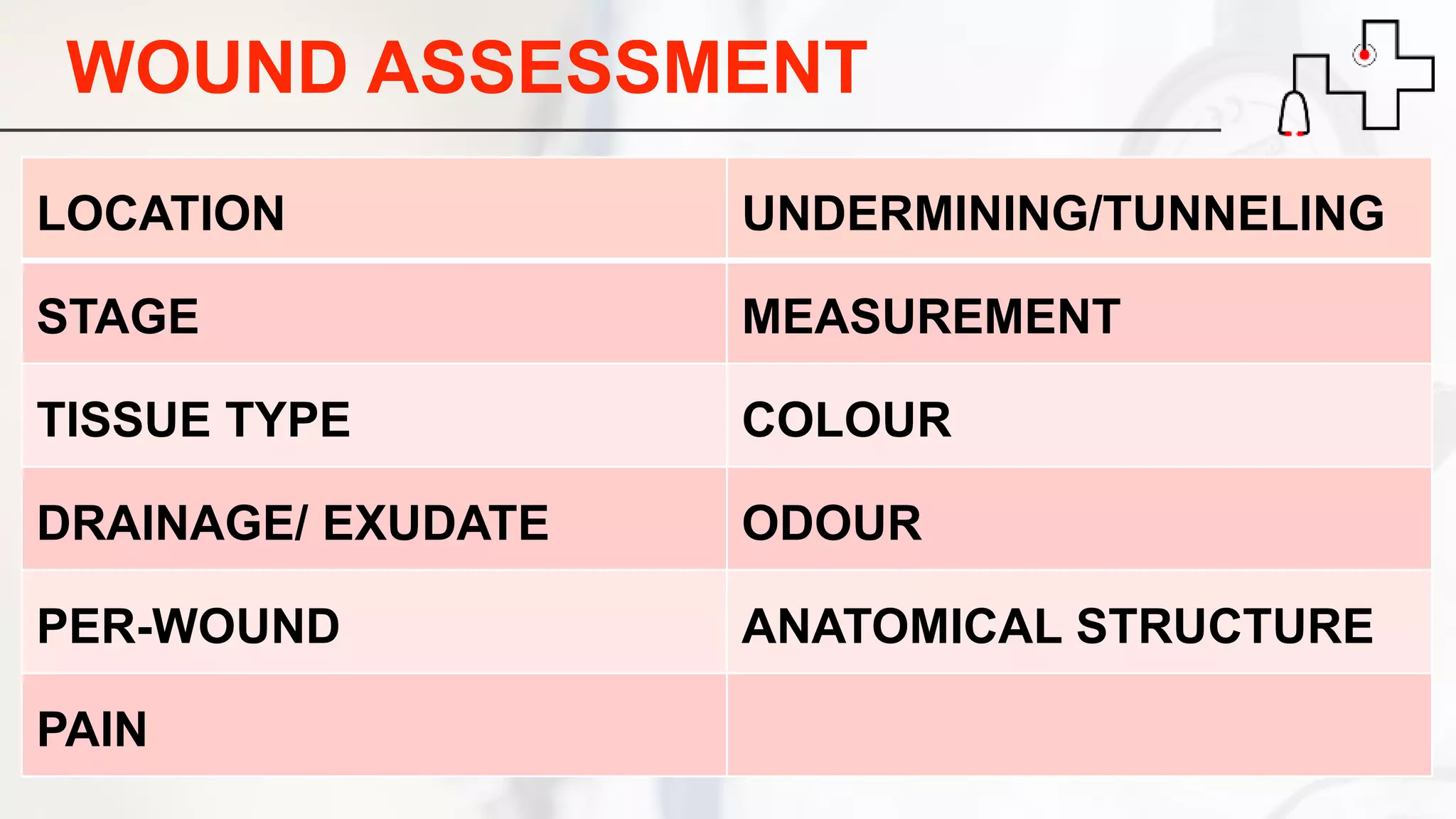
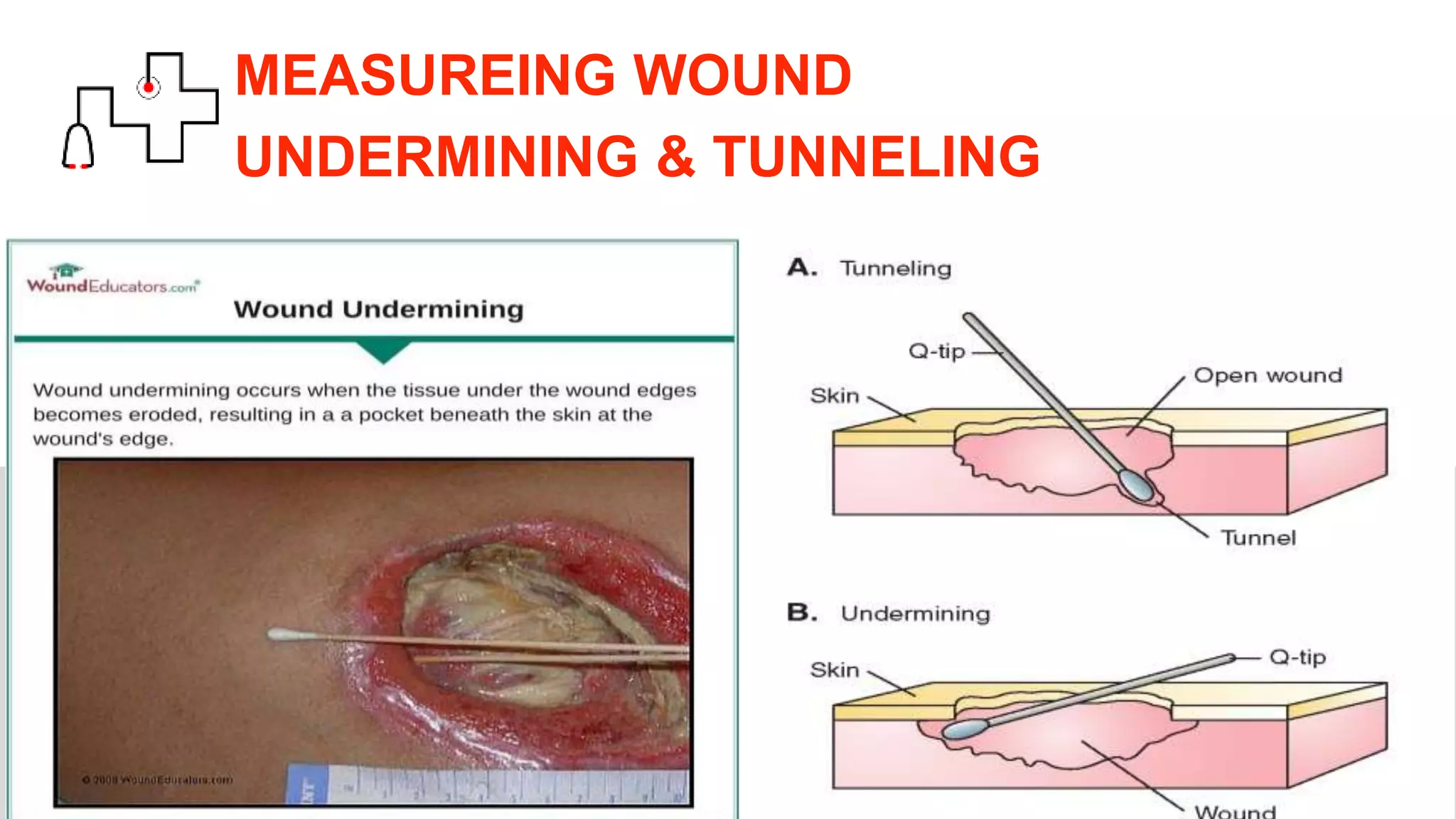
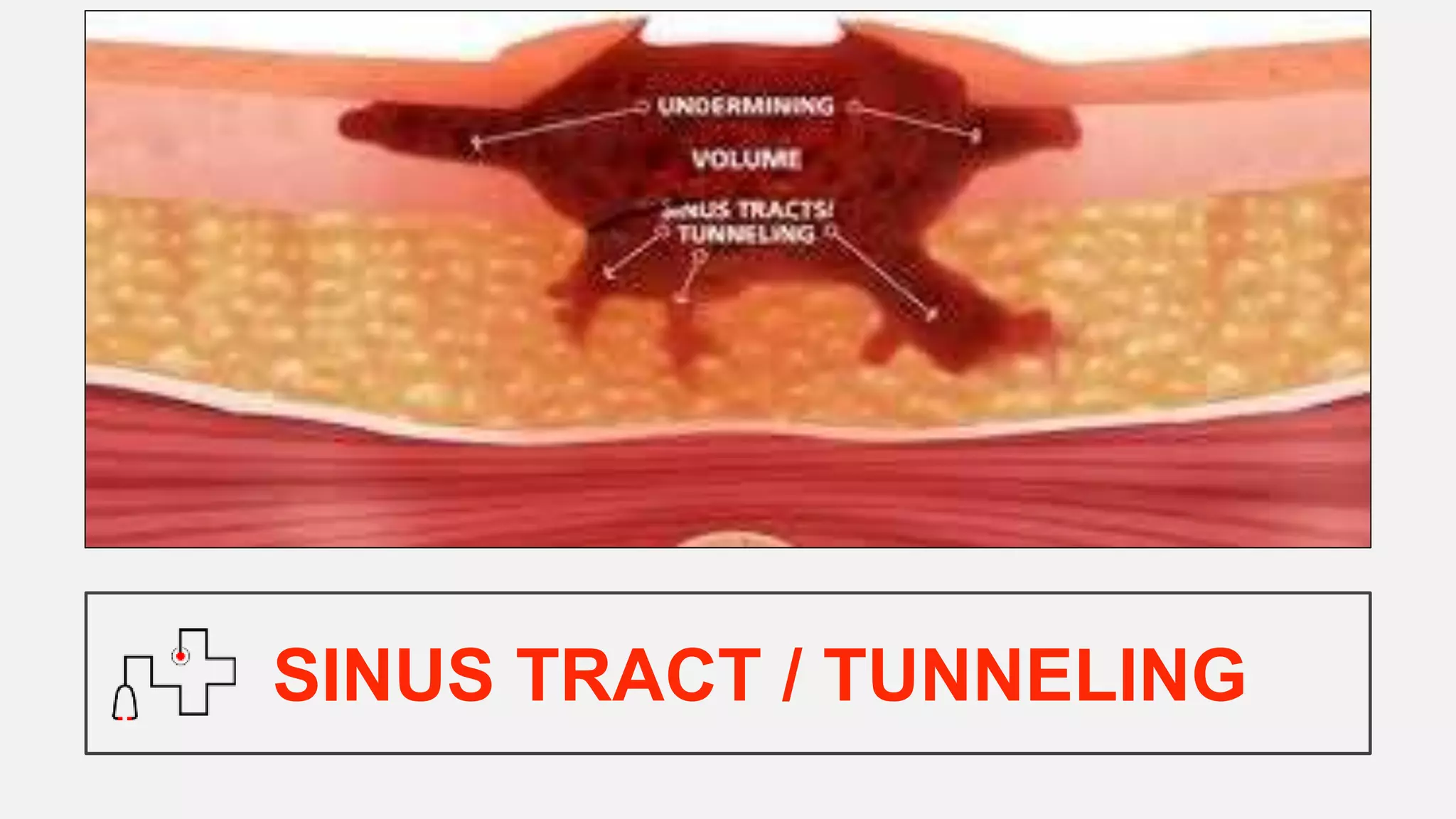
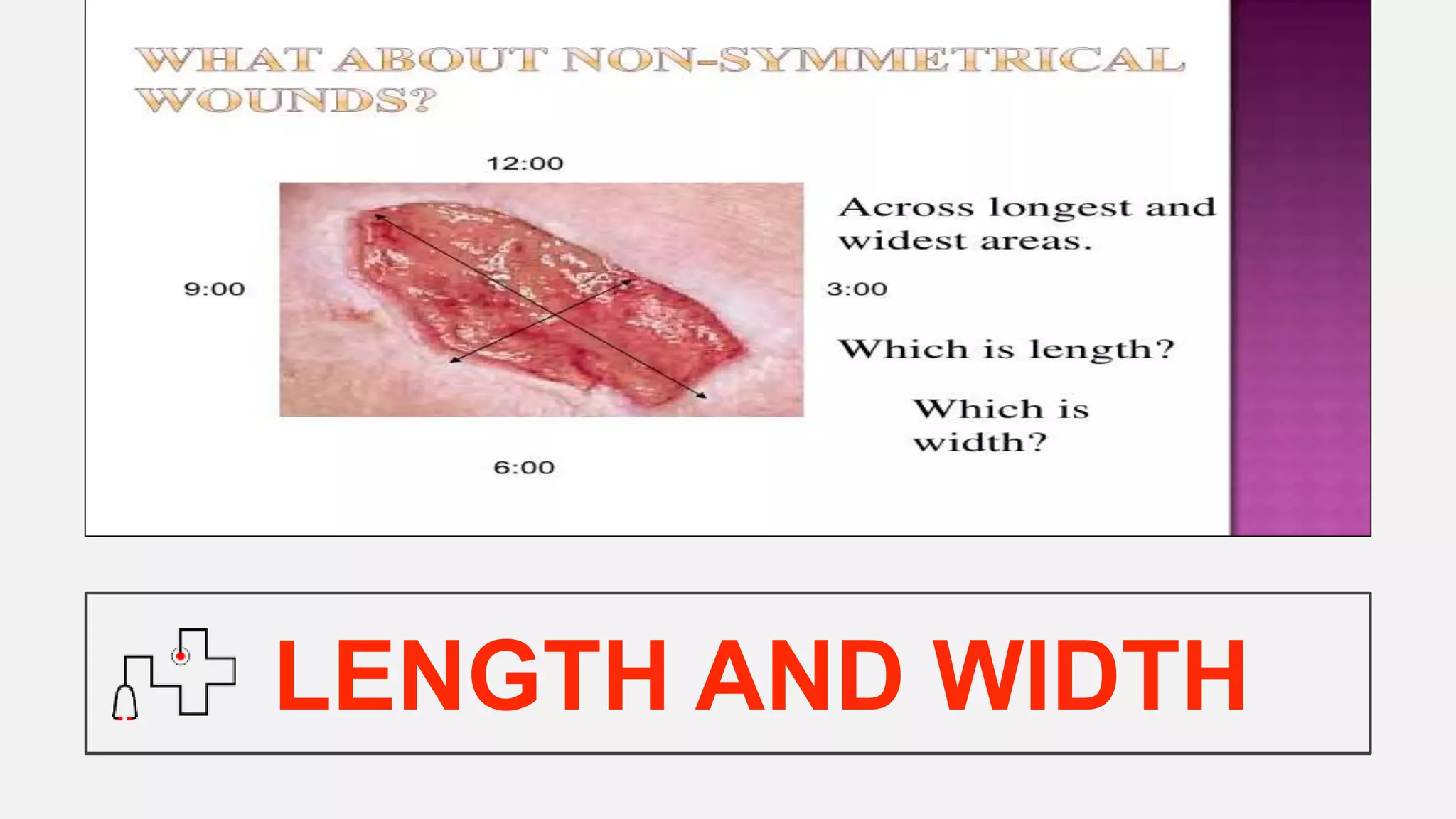
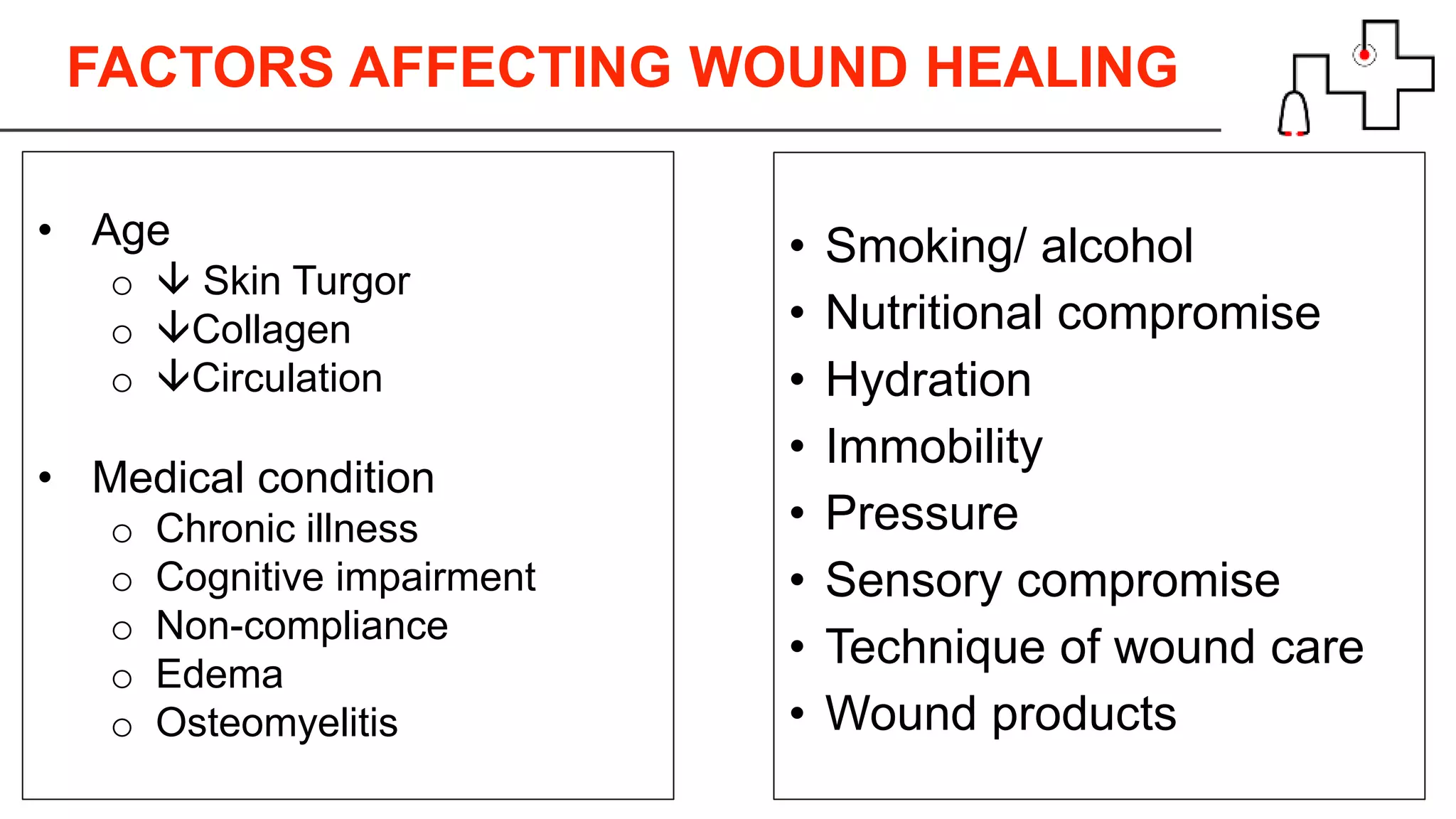
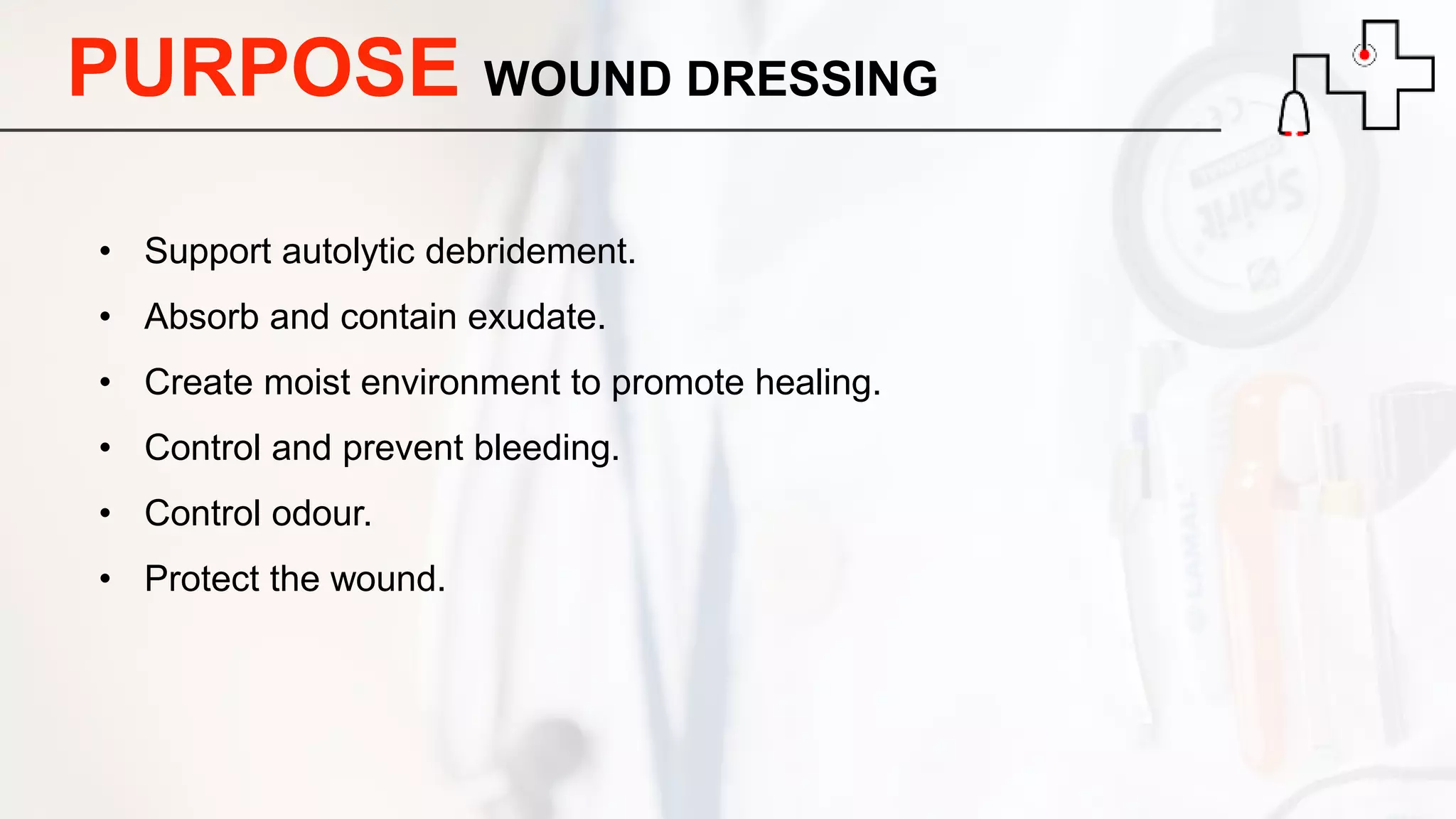
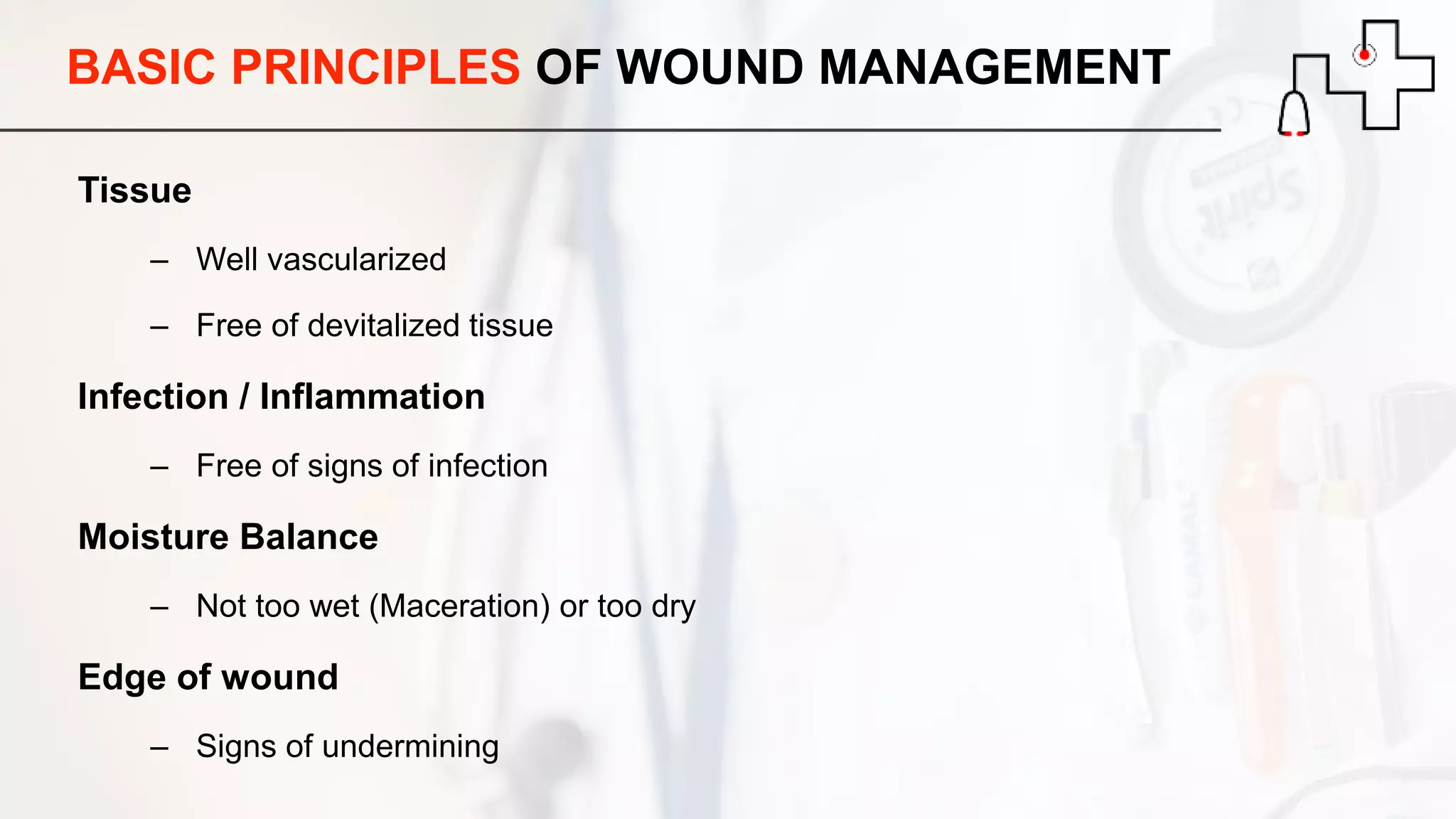
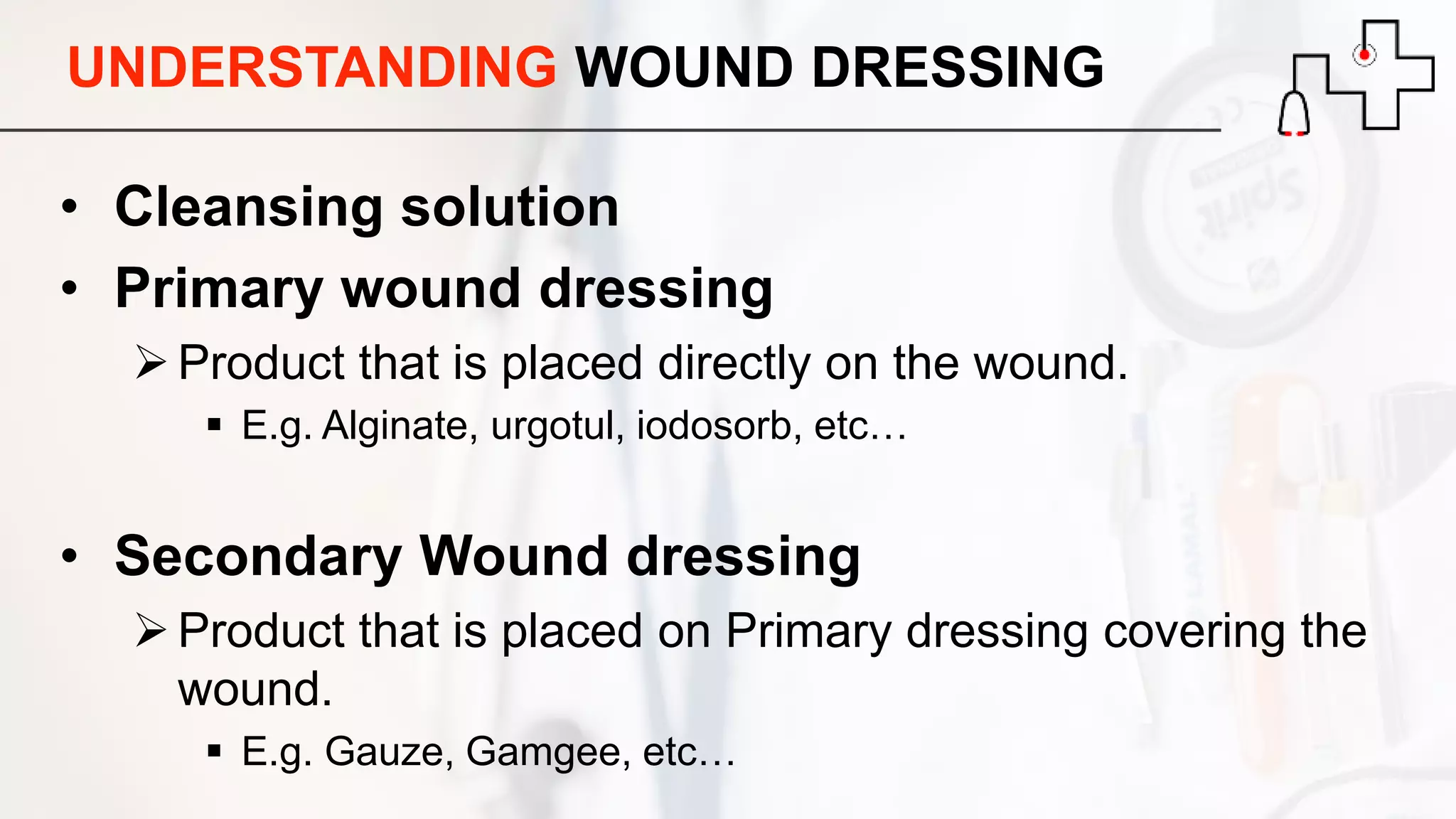
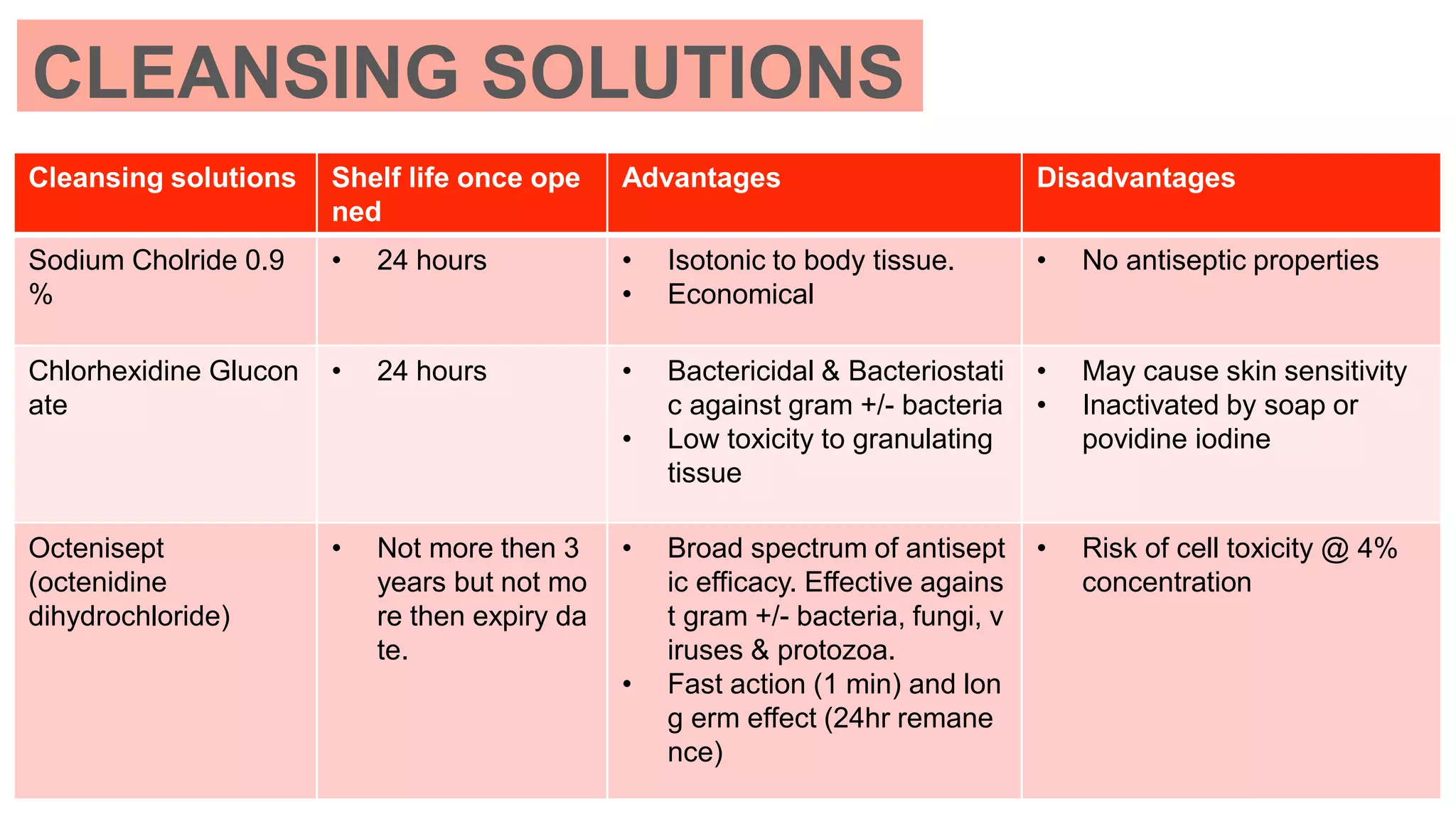
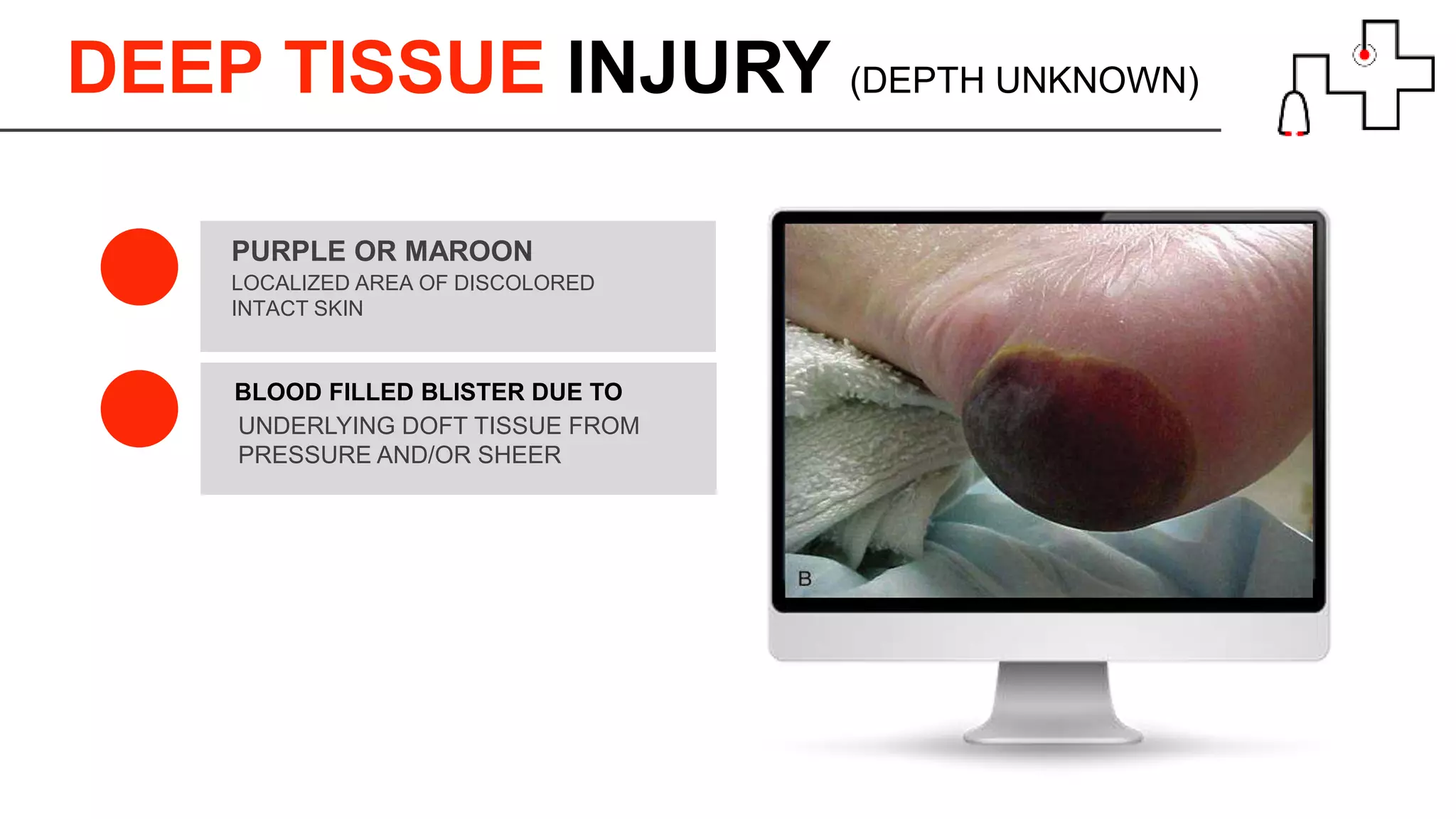
This document outlines key concepts in managing wound care for elderly individuals in nursing homes, focusing on skin tear classifications, incontinence-associated dermatitis, and pressure injuries. It details the characteristics of skin changes in older adults, assessment procedures, wound management techniques, and various wound care products available. Additionally, it emphasizes the importance of prevention strategies and the appropriate nursing interventions to enhance wound healing.