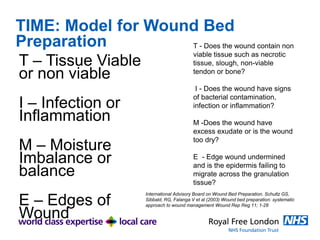
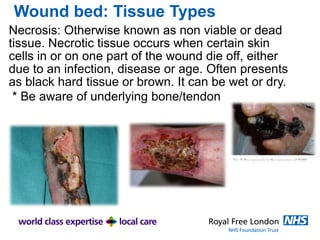
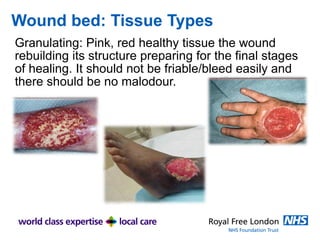
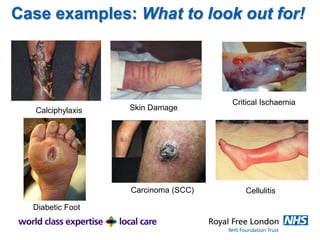
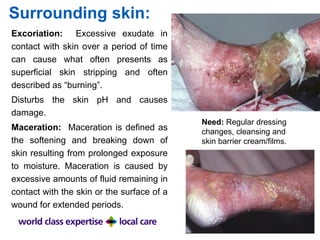
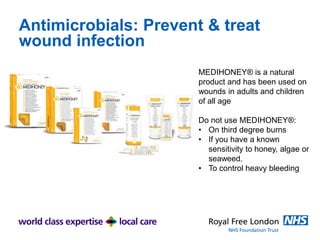
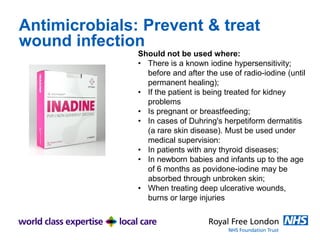
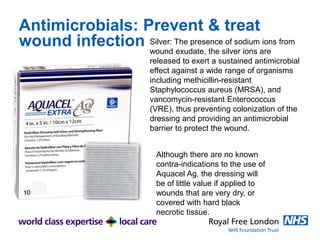
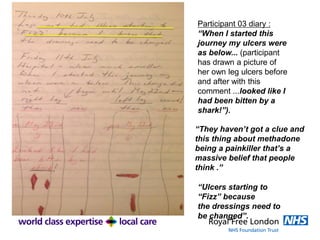
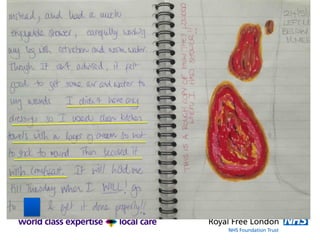
The document discusses the challenges of wound care for homeless individuals, including difficulties in accessing healthcare and types of wounds they face. It emphasizes the importance of proper wound assessment, management, and self-care techniques while outlining specific strategies to improve client experiences in general practice. Additionally, it provides guidance on wound bed preparation, antimicrobial use, and promoting self-care and independence in wound healing.