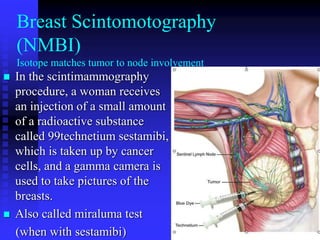
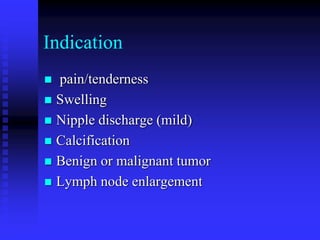
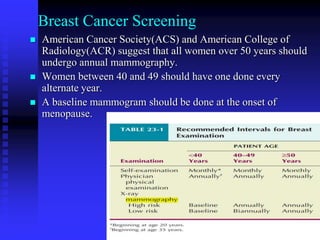
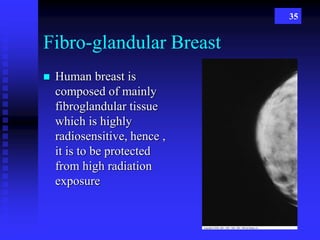
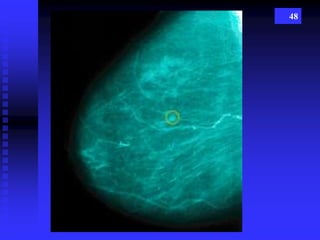
Mammography is a crucial radiographic technique for early detection of breast cancer, which affects 1 in 8 women in the U.S. Mammograms can identify cancers 2-3 years before they are palpable, with a detection rate of 85-90%. The document covers various mammographic techniques, patient preparation, risk factors, and technological advancements, emphasizing the importance of regular screenings for women over 40.


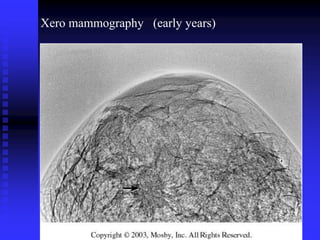
![Xeromammography
Xeromammography is a photoelectric method of
recording an x-ray image on a coated metal plate,
using low-energy photon beams, long exposure
time, and dry chemical developers.
It is a form of xeroradiography.[1]
This process was developed in the late 1960s by
Jerry Hedstrom, and used to image soft tissue, and
later focused on using the process to detect breast
cancer.](https://image.slidesharecdn.com/mammography-170203052838/85/Mammography-60-320.jpg)