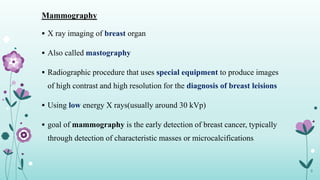
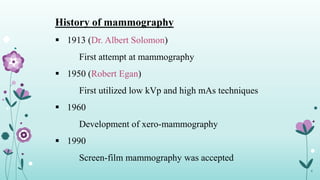
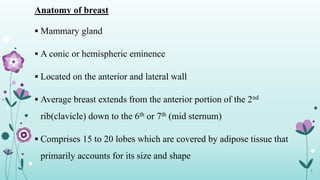
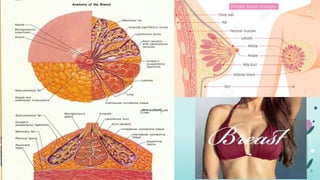
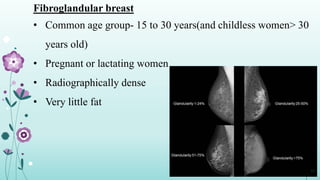
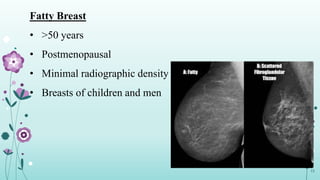
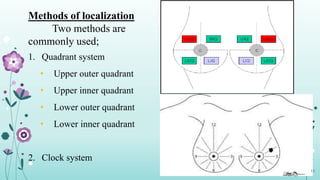
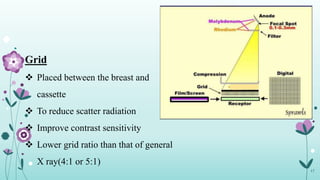
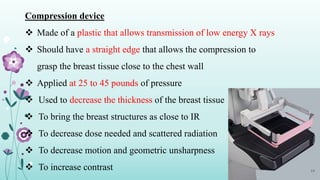
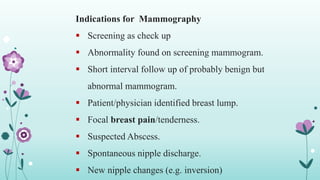
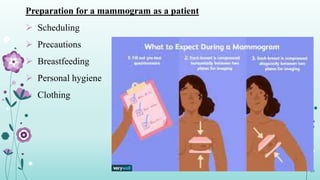
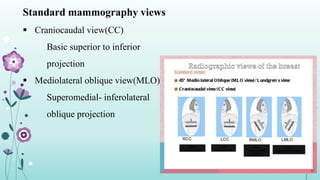
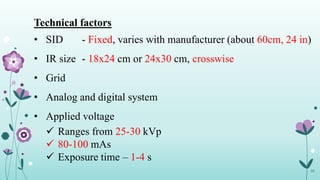
The document presents an overview of mammography, detailing its definition, history, equipment, and various types used for breast cancer detection. It emphasizes patient preparations, indications for mammography, and radiation safety, highlighting the benefits of early detection. Additionally, it discusses technical factors and specific views related to mammography imaging.