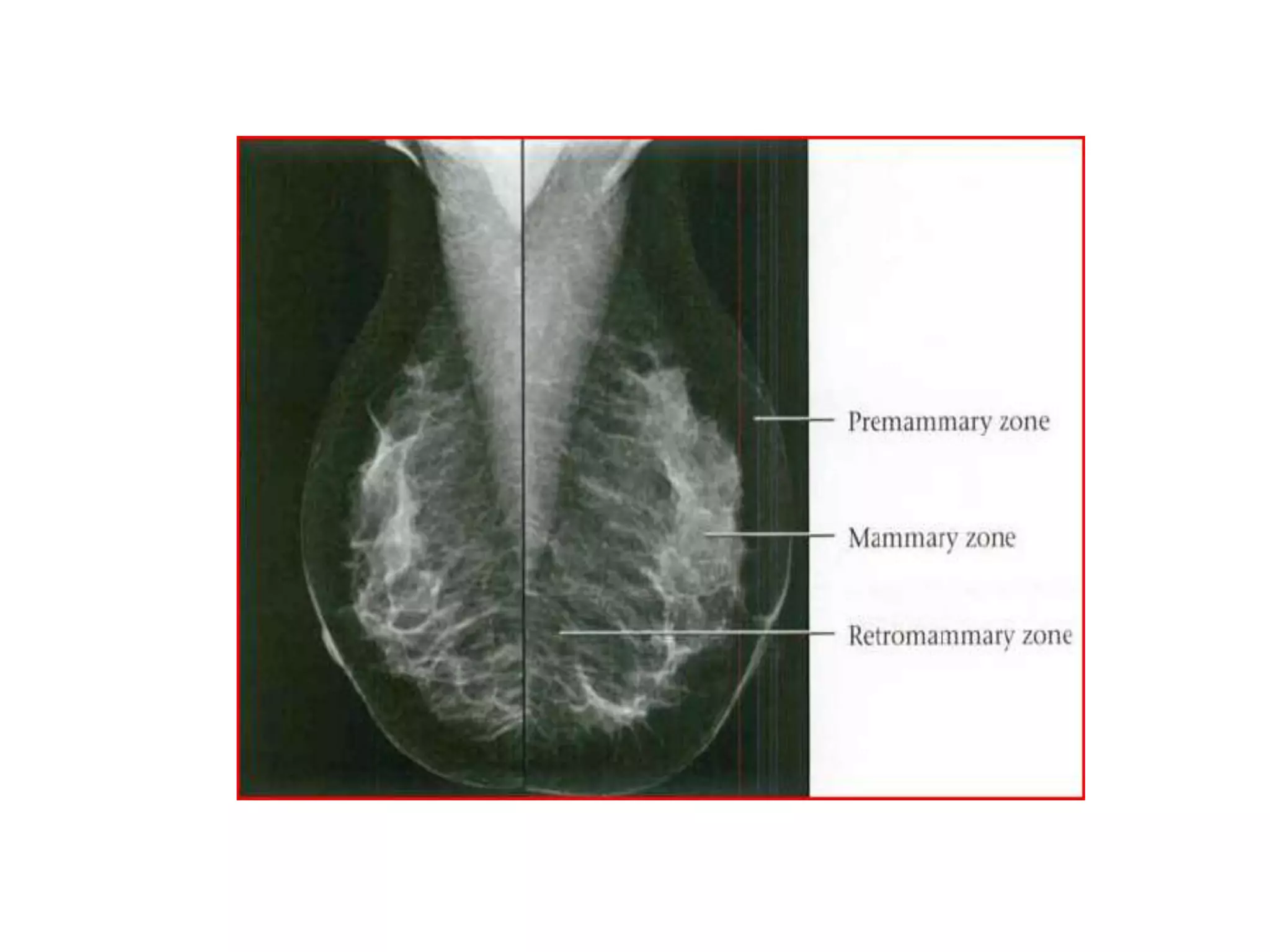
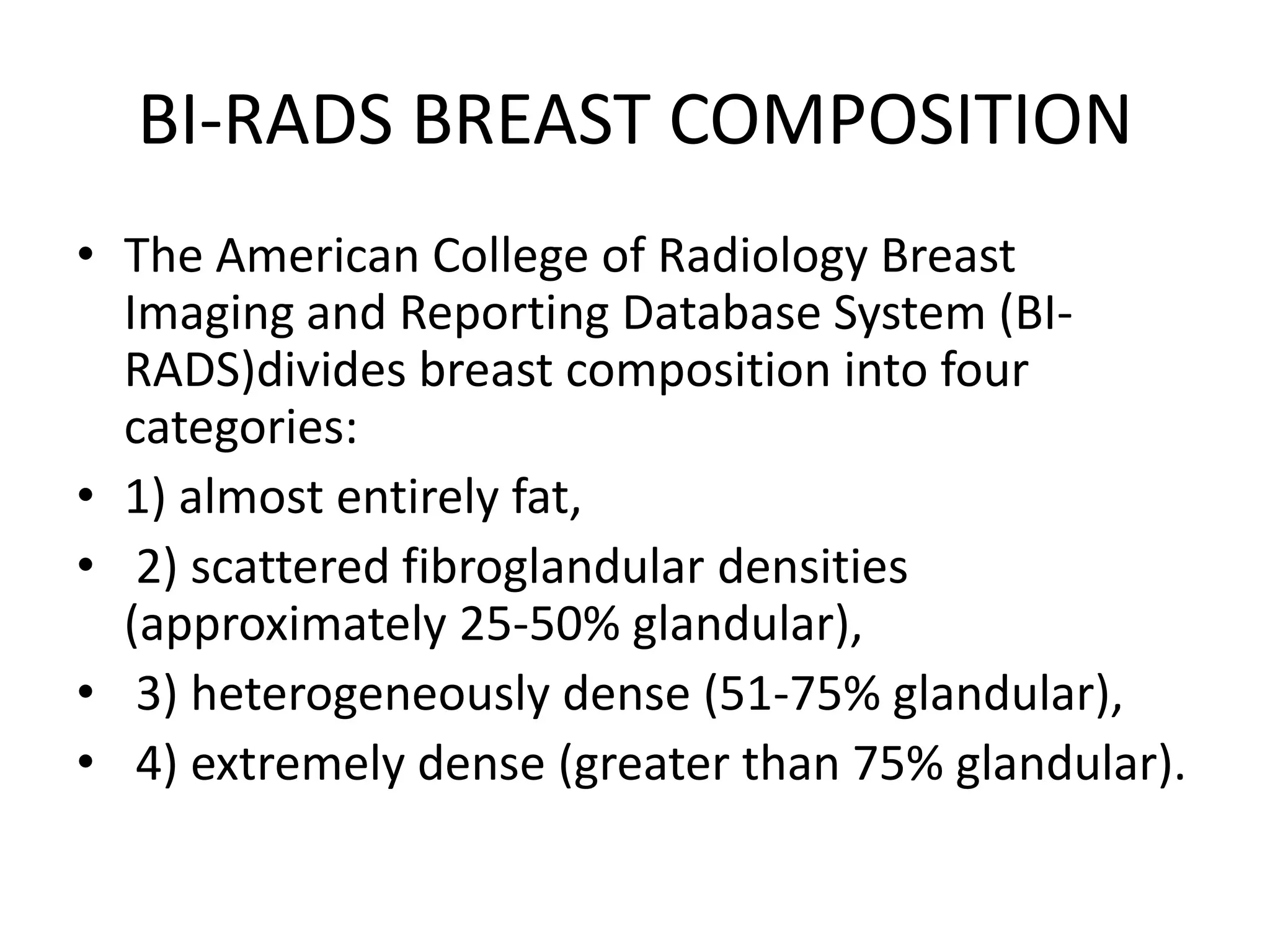
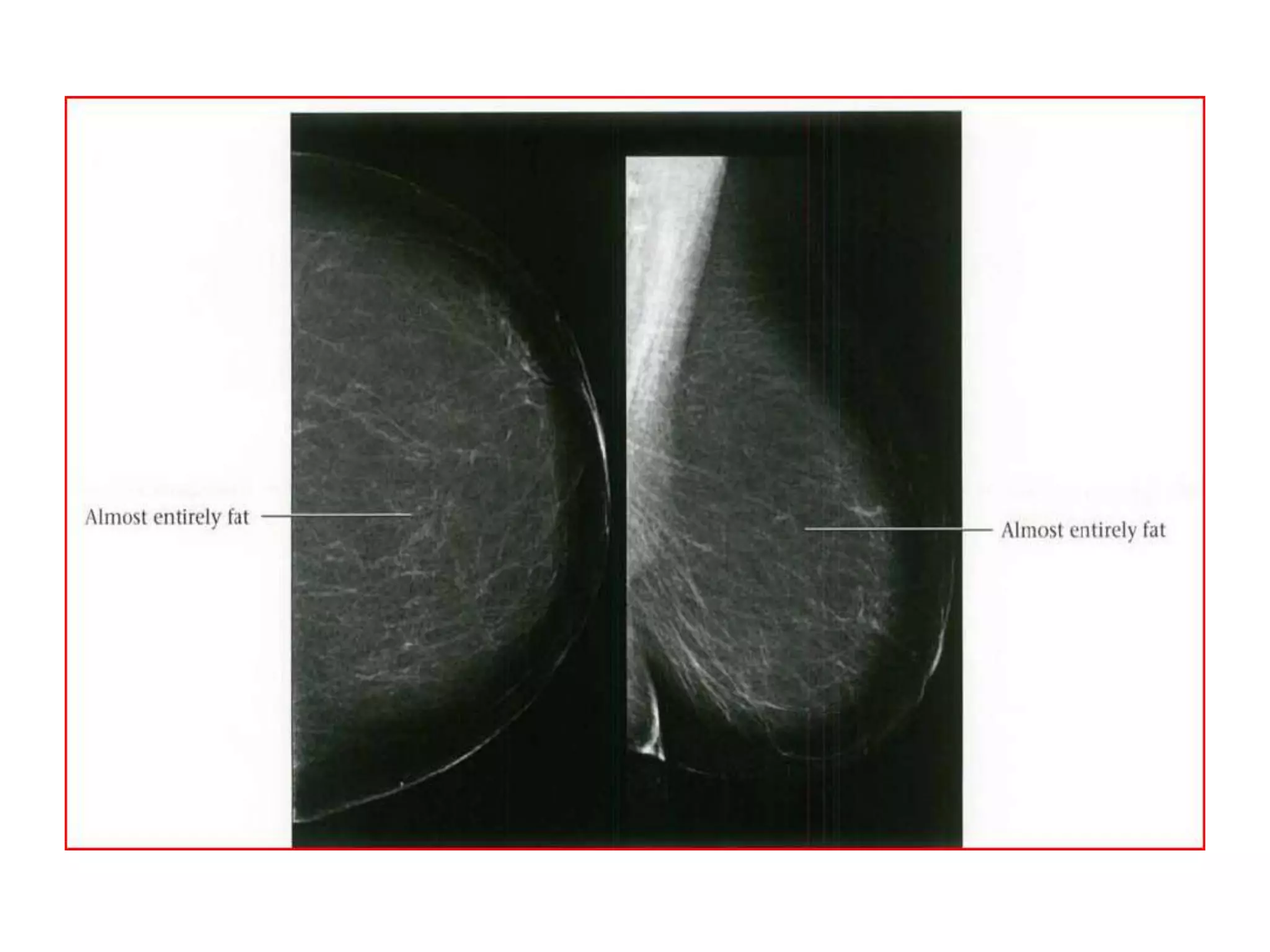
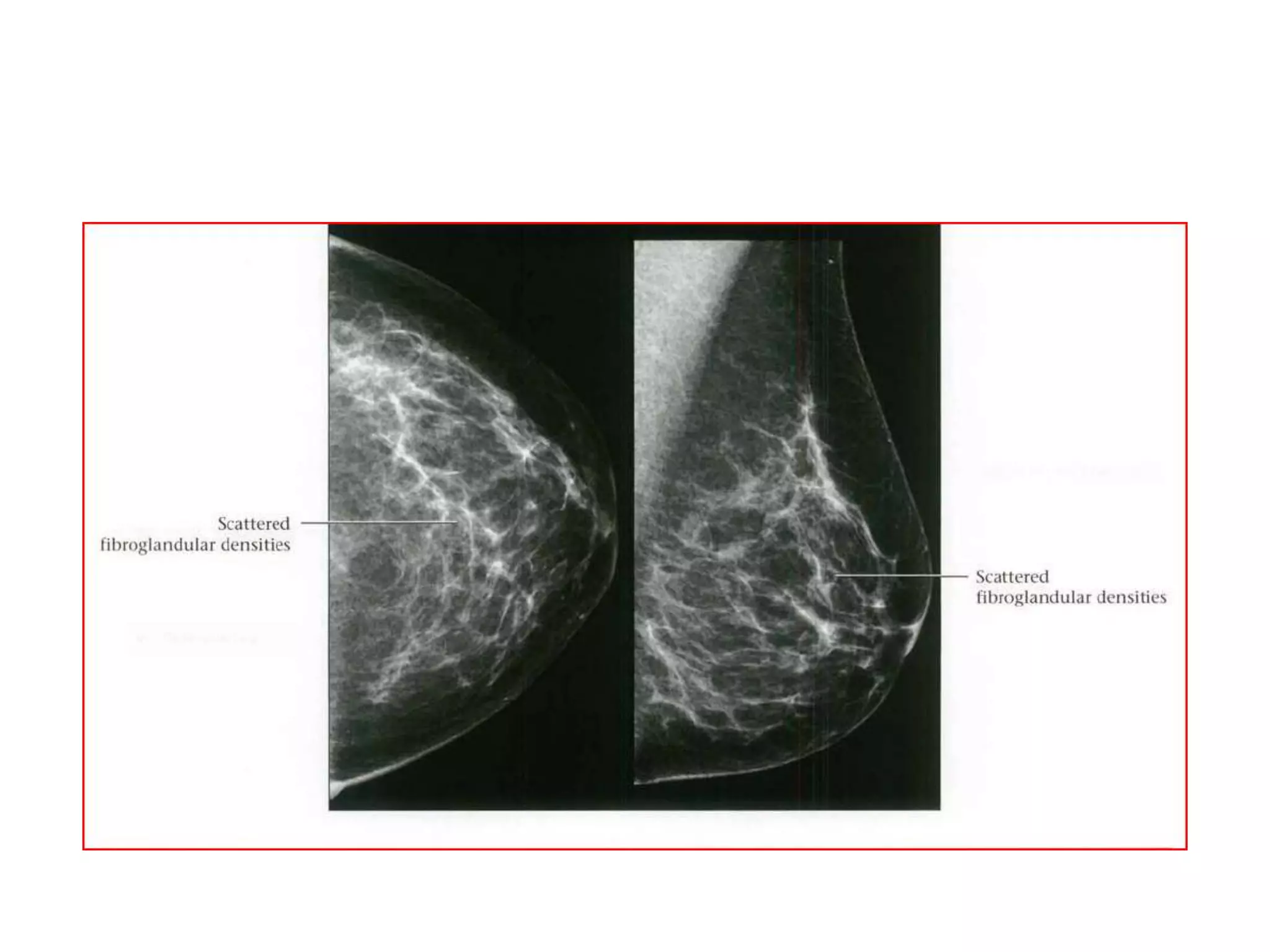
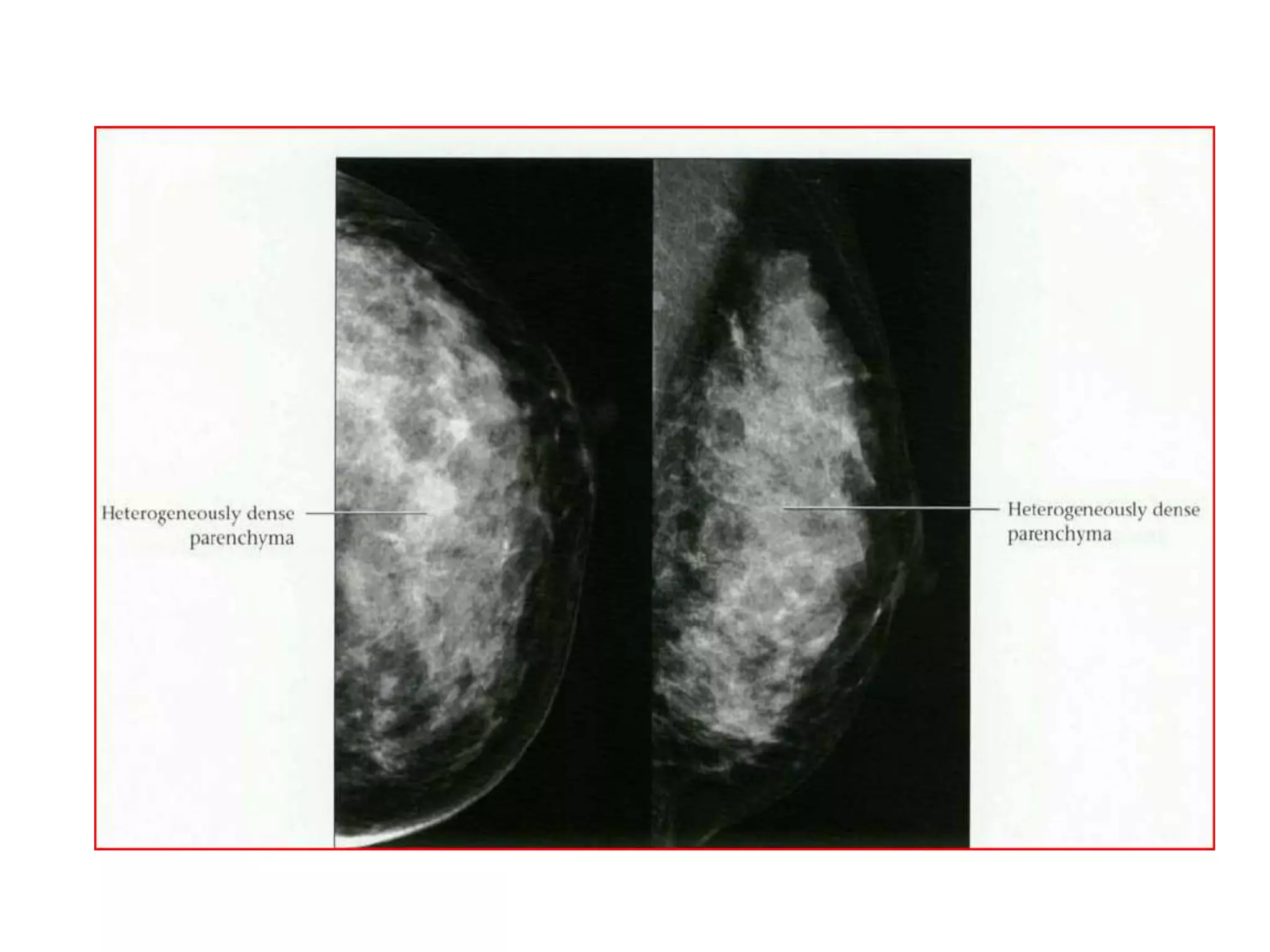
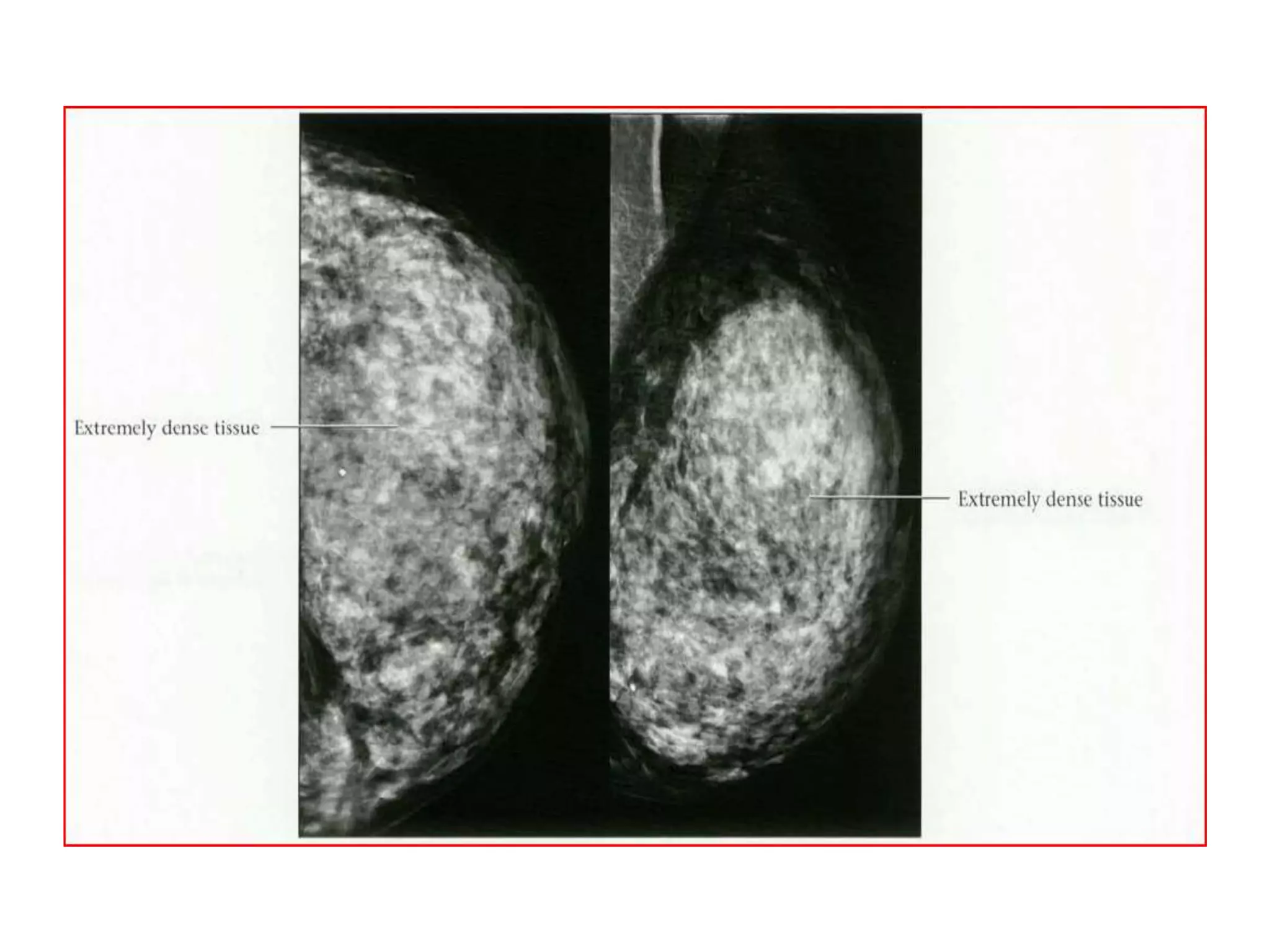
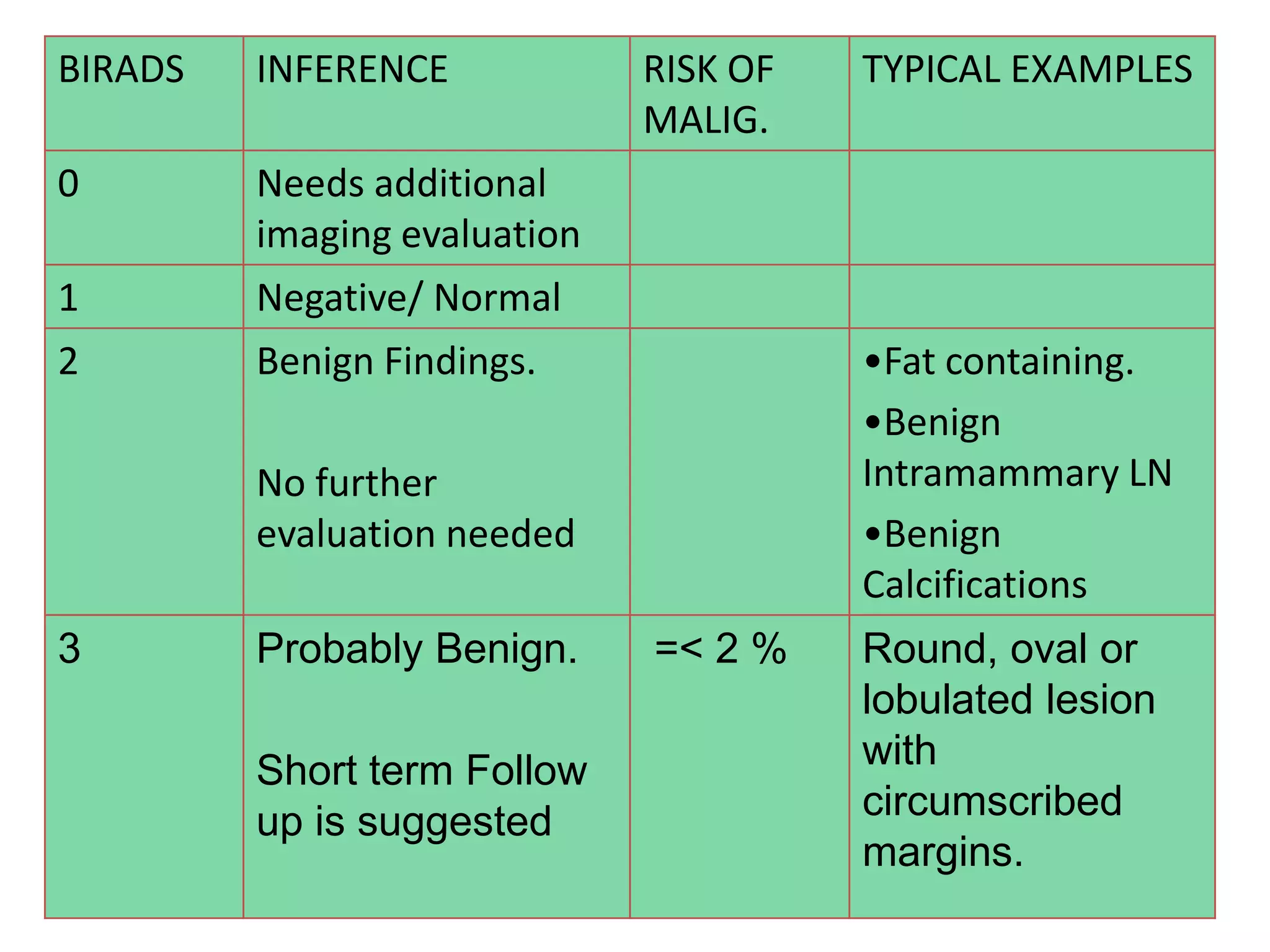
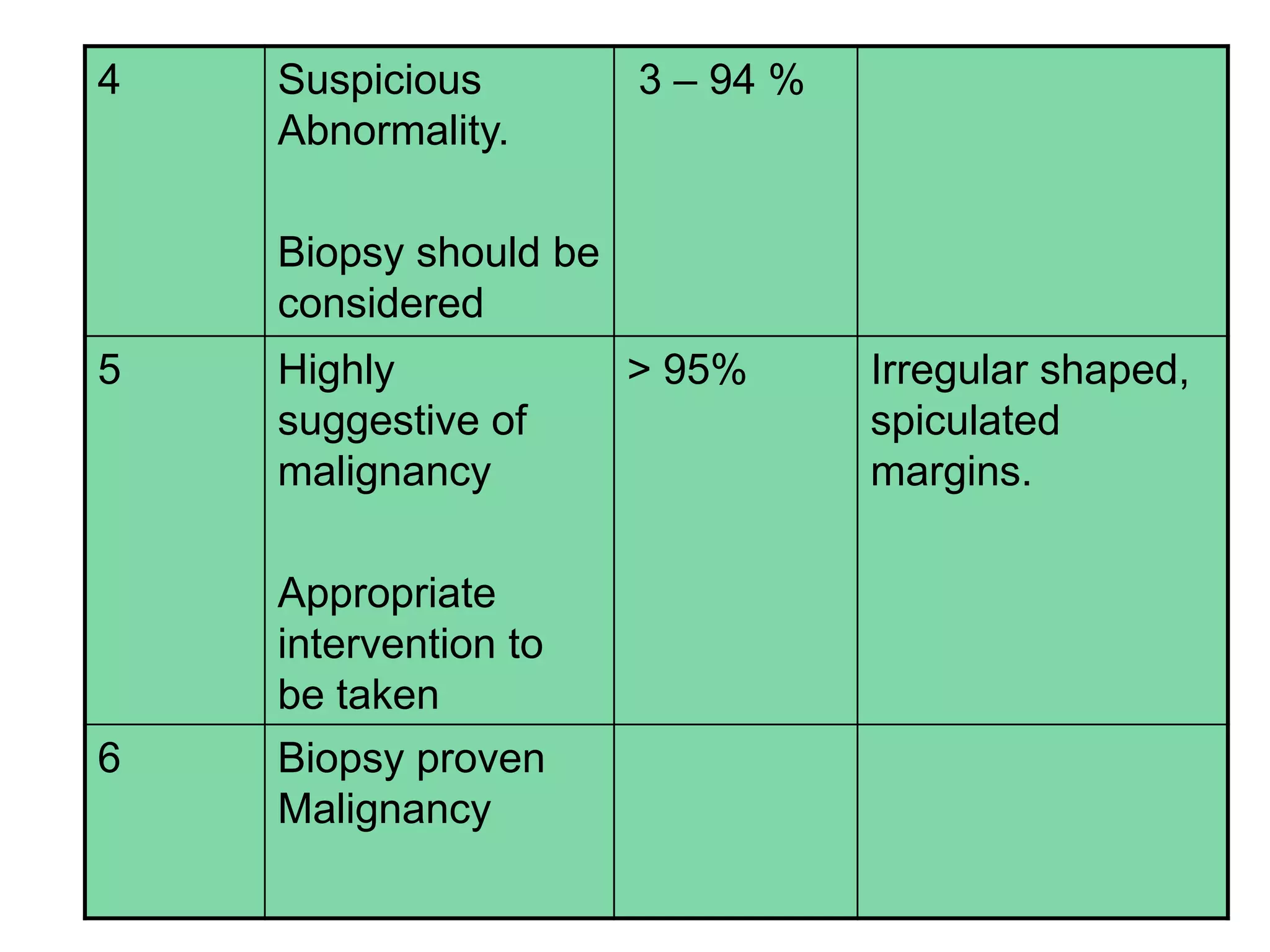
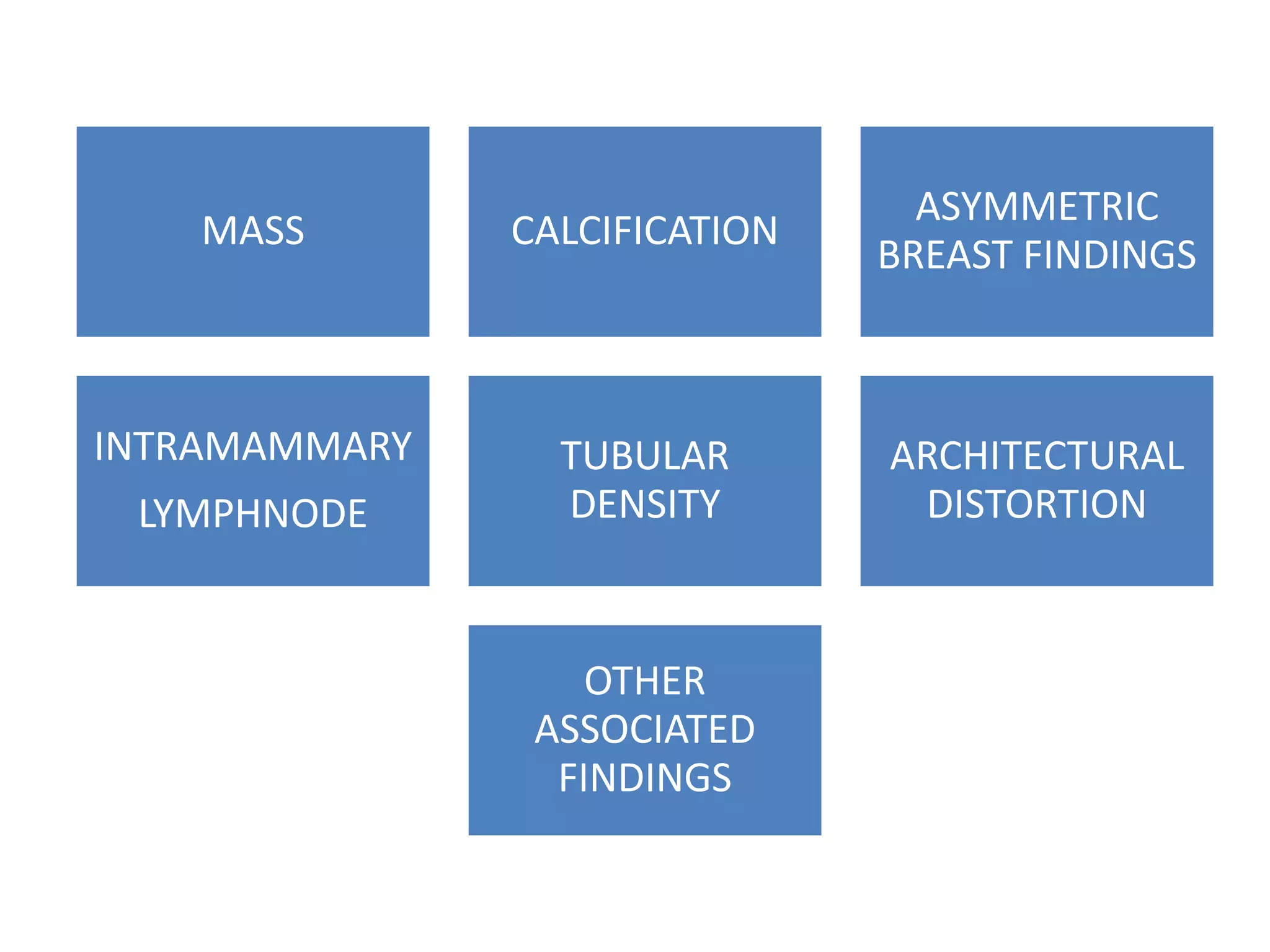
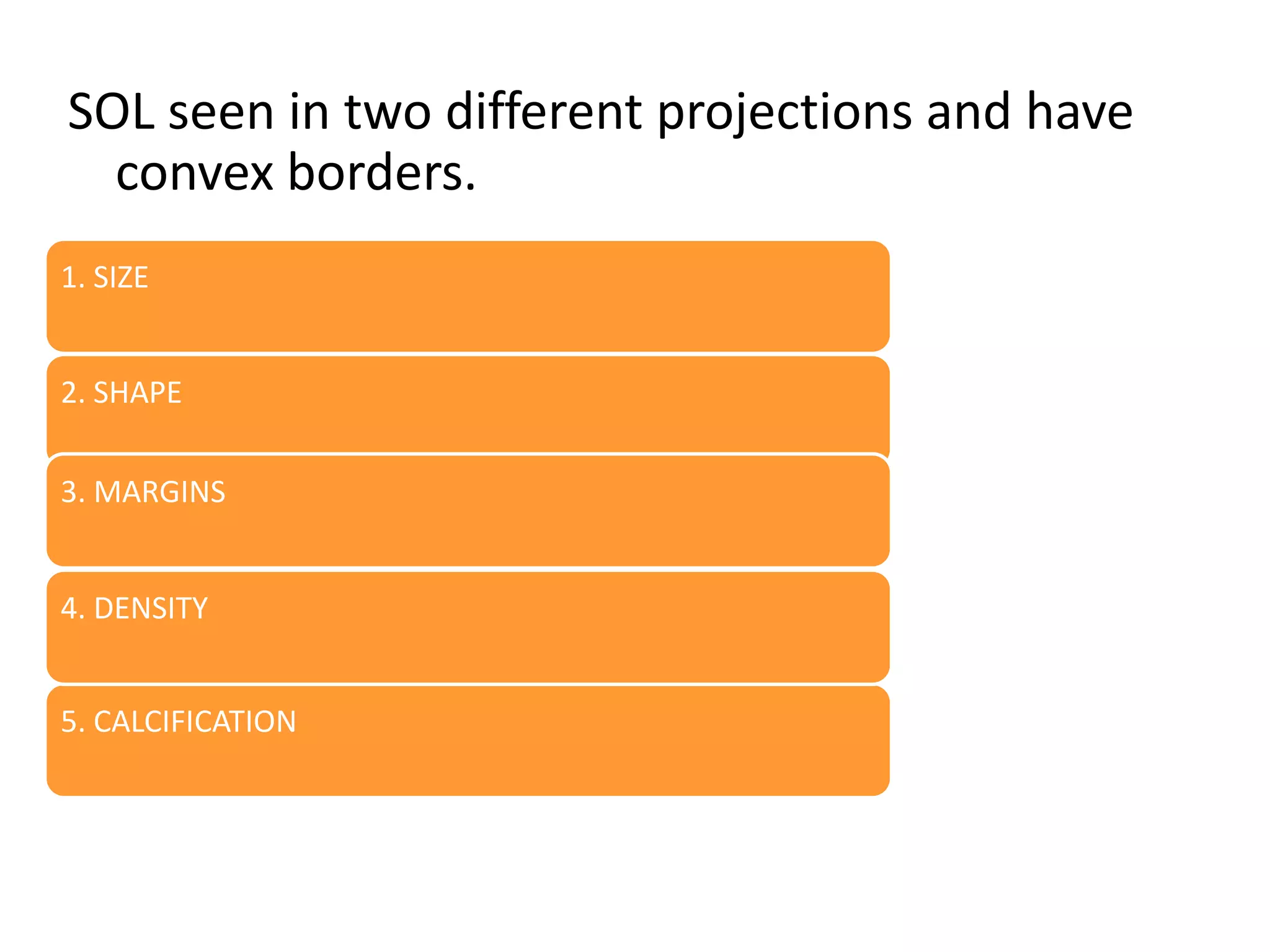
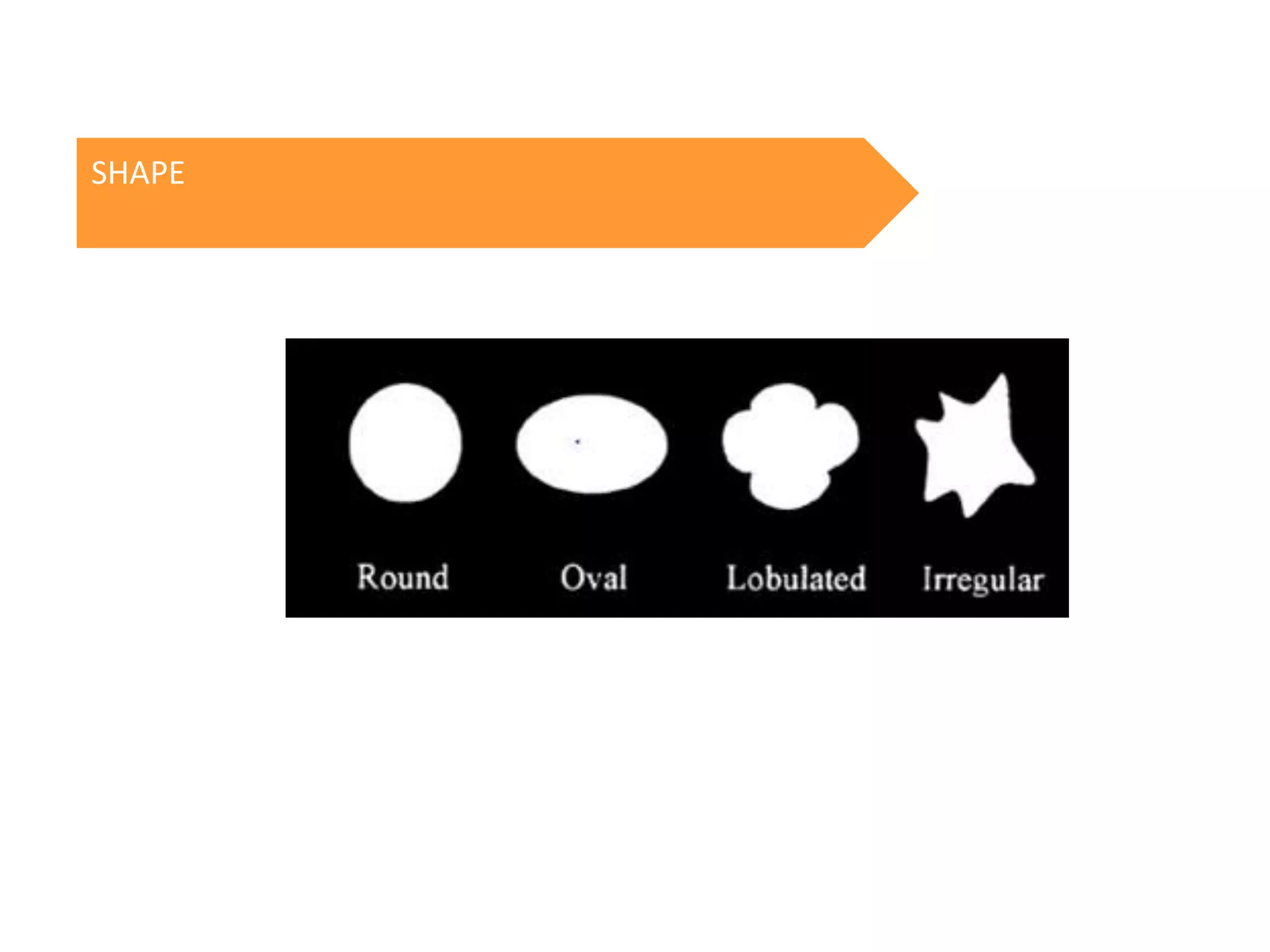
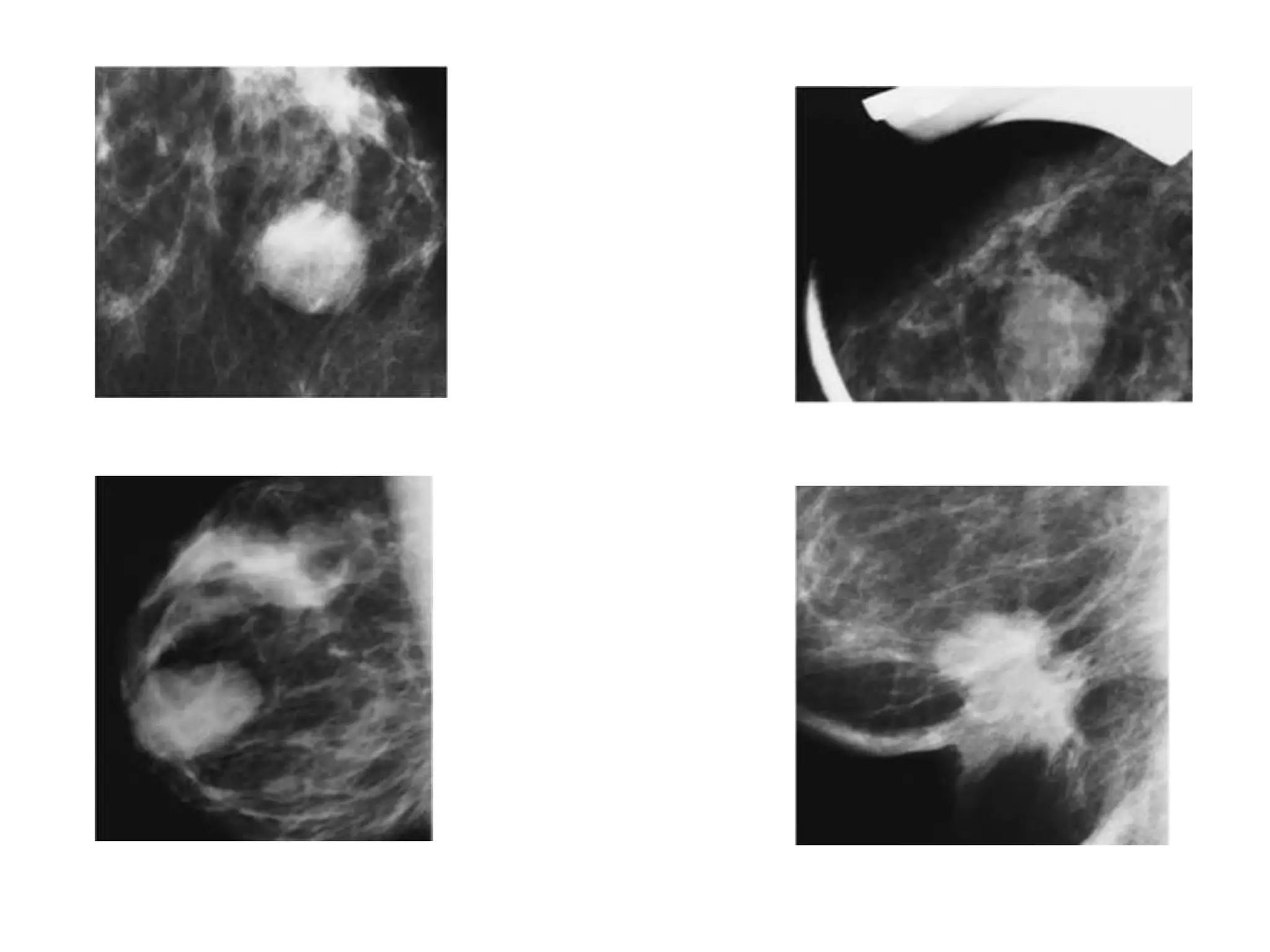
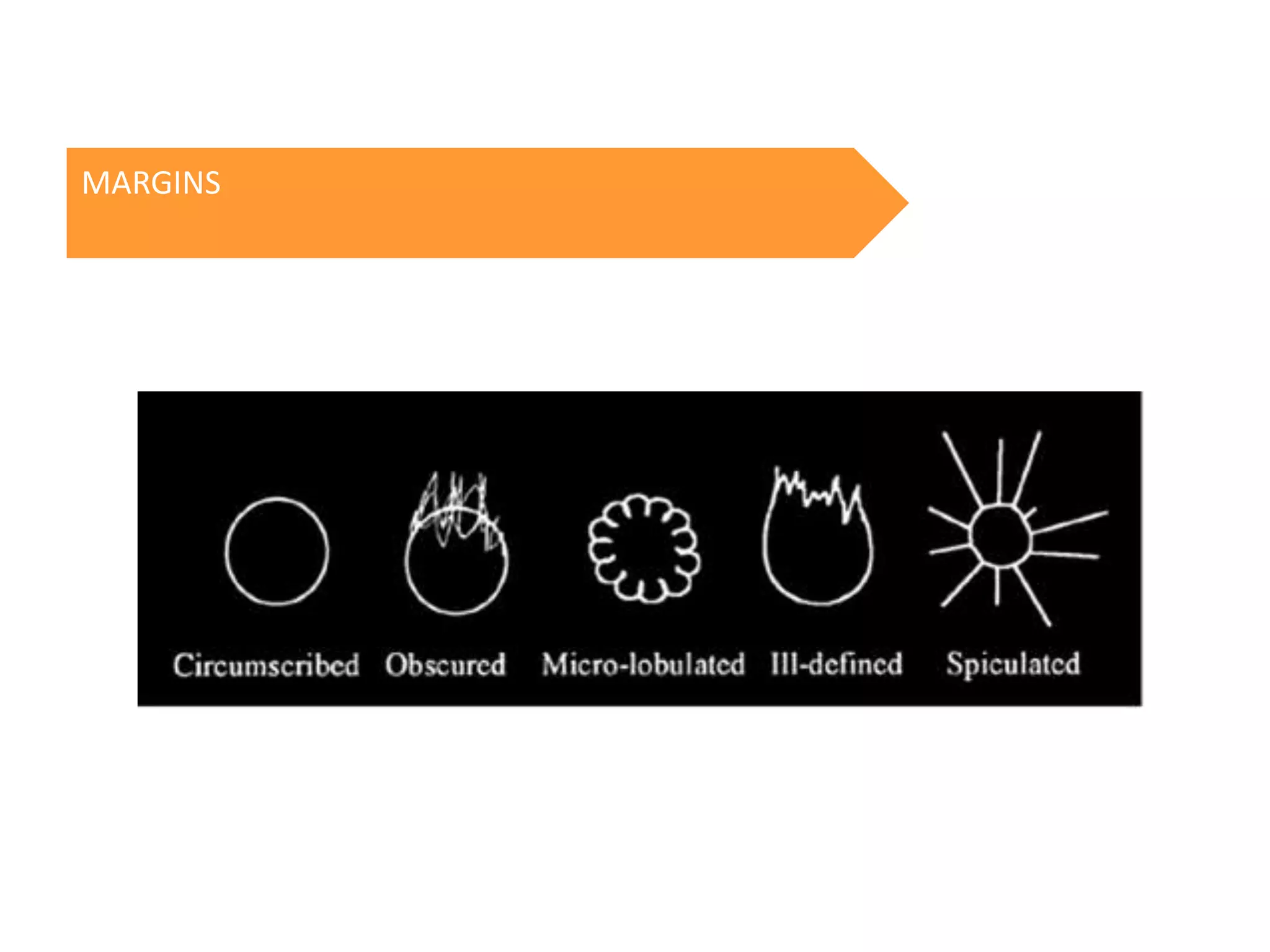
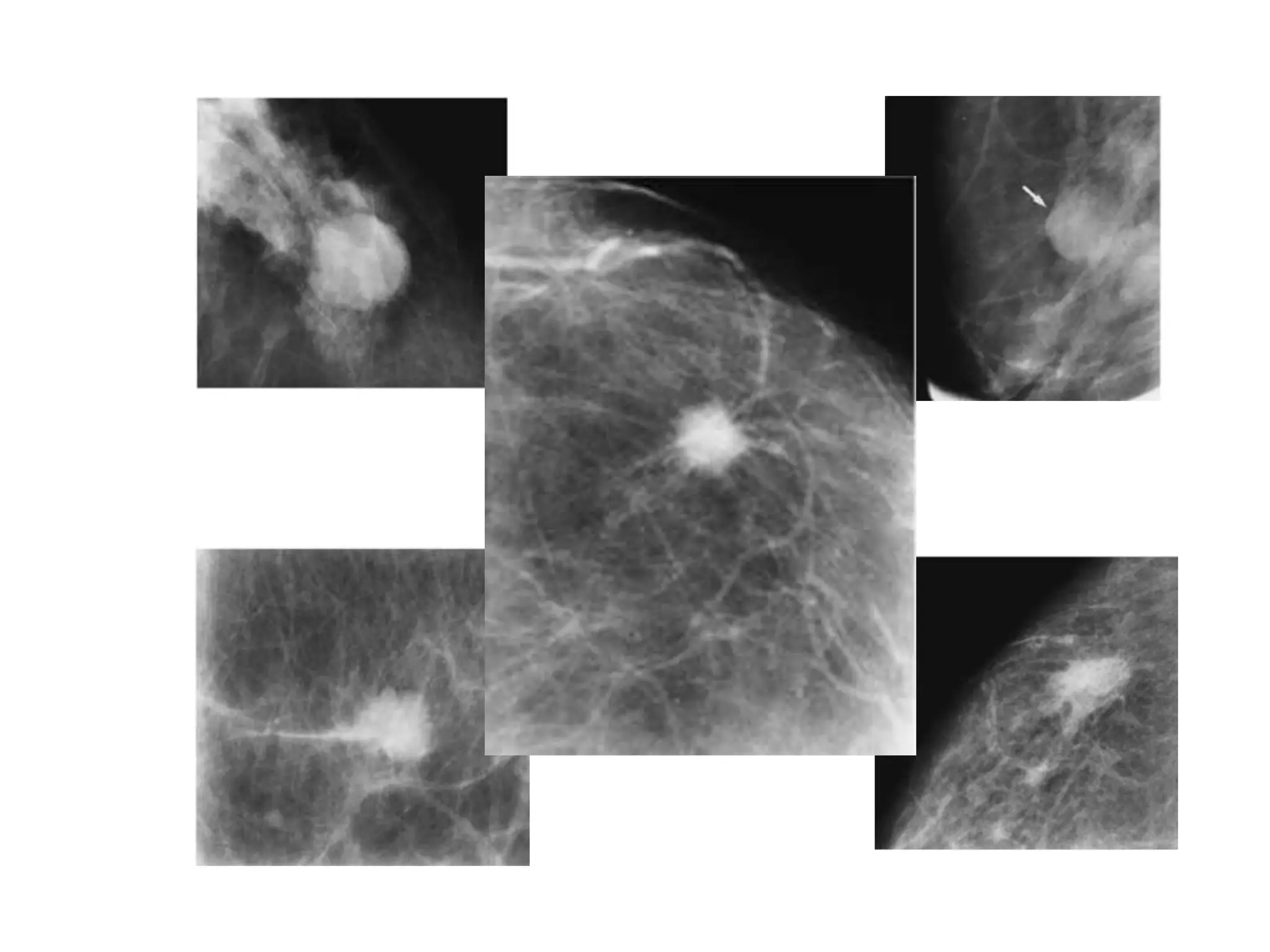
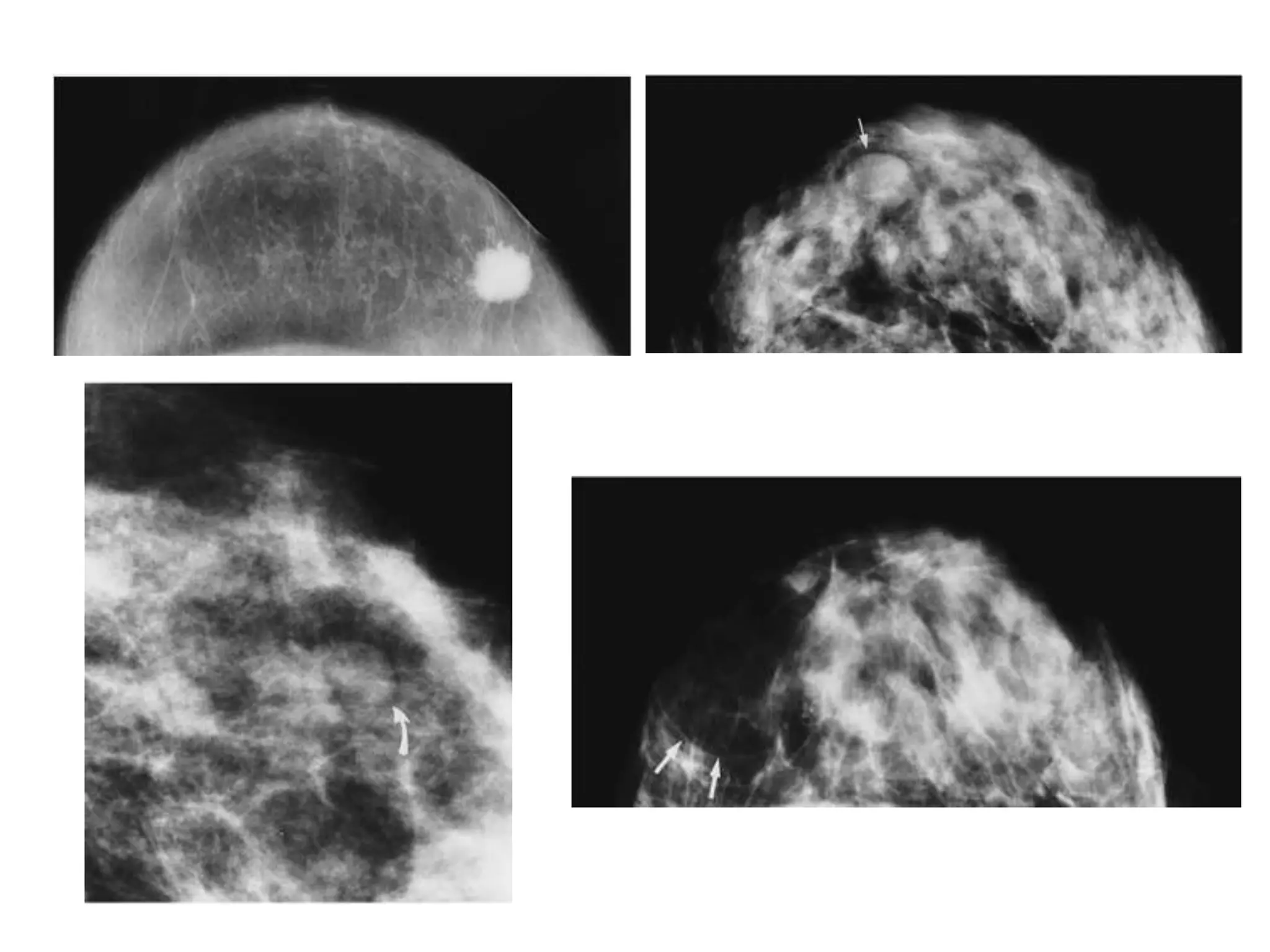
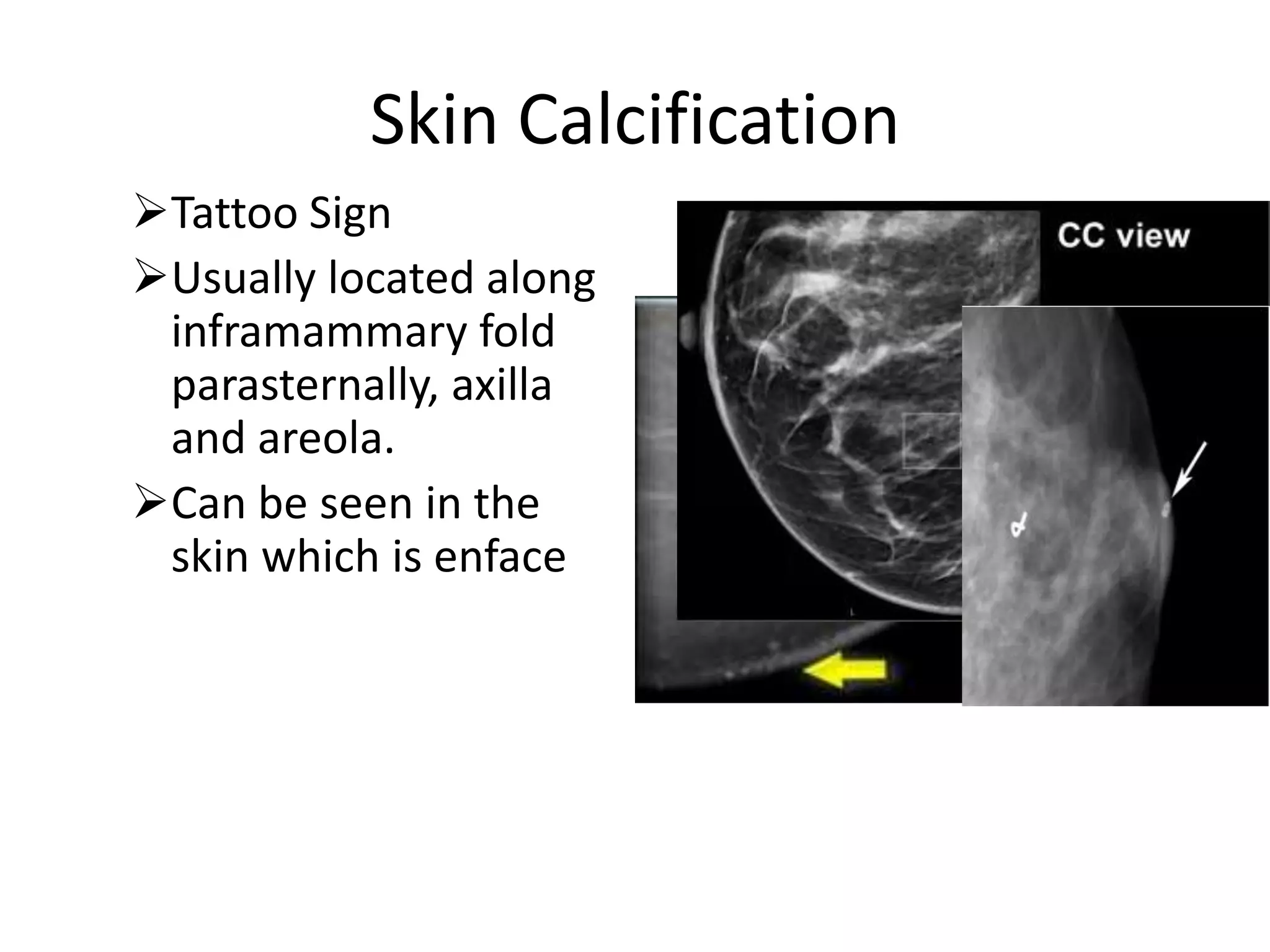
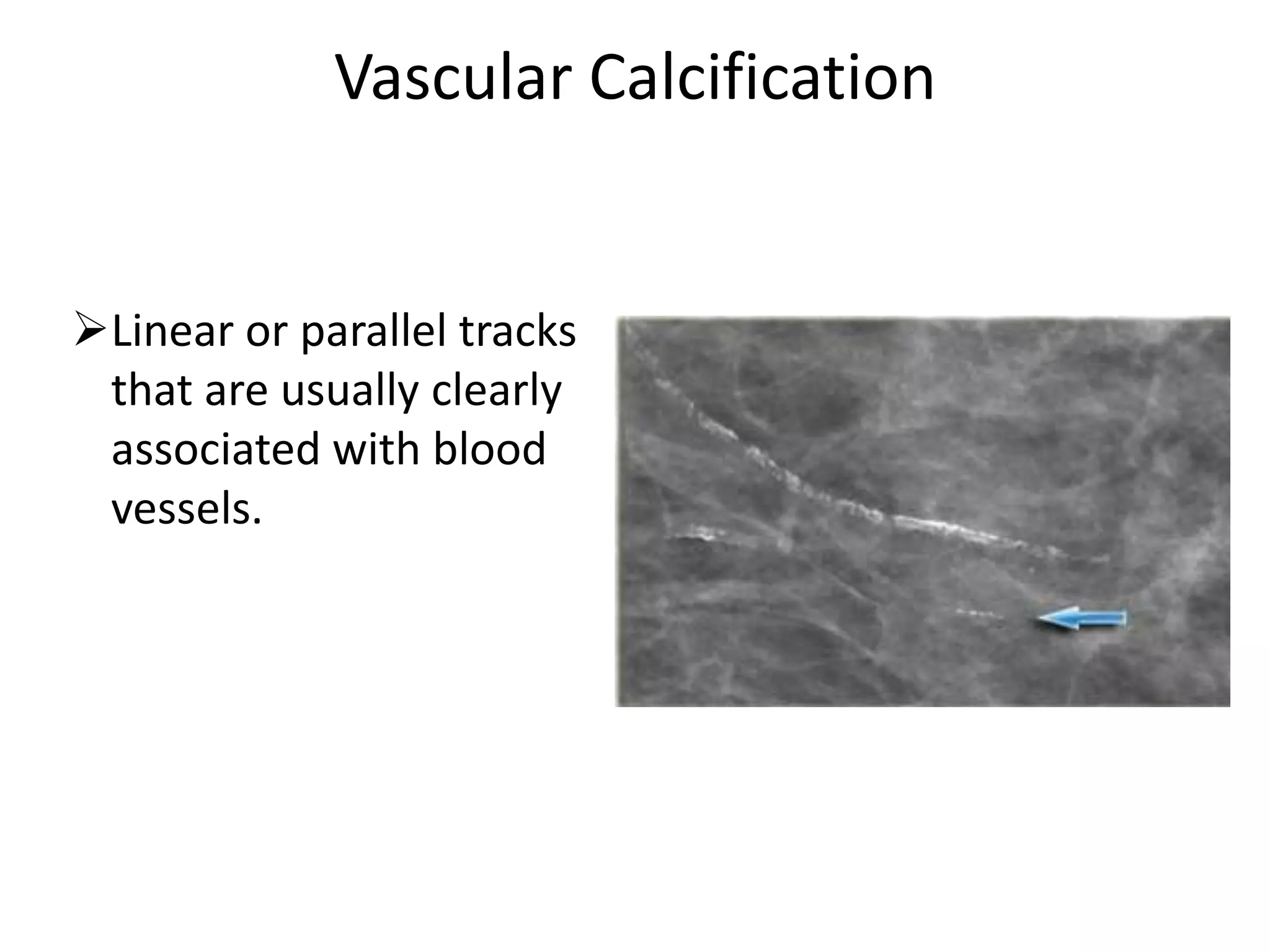
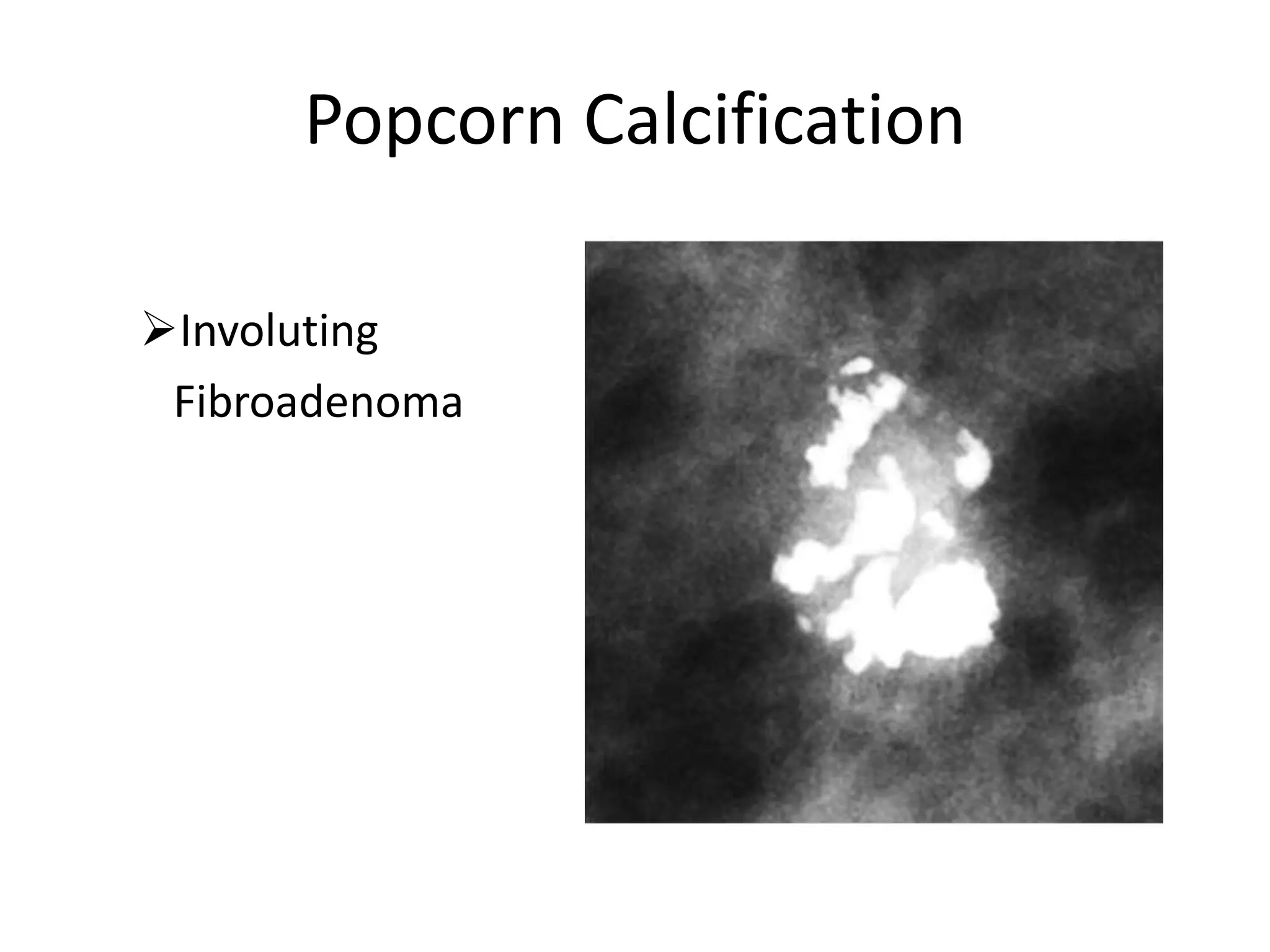
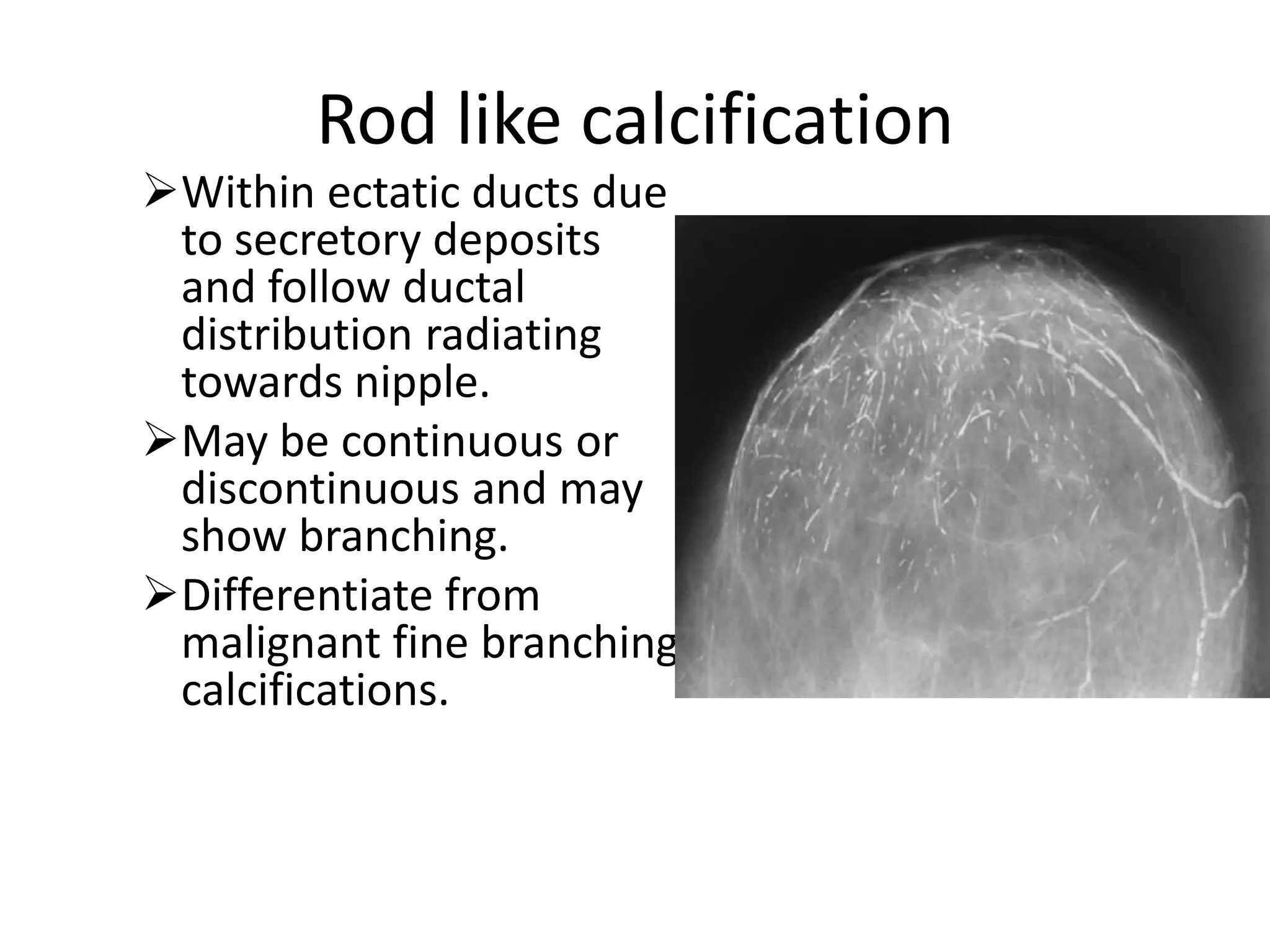
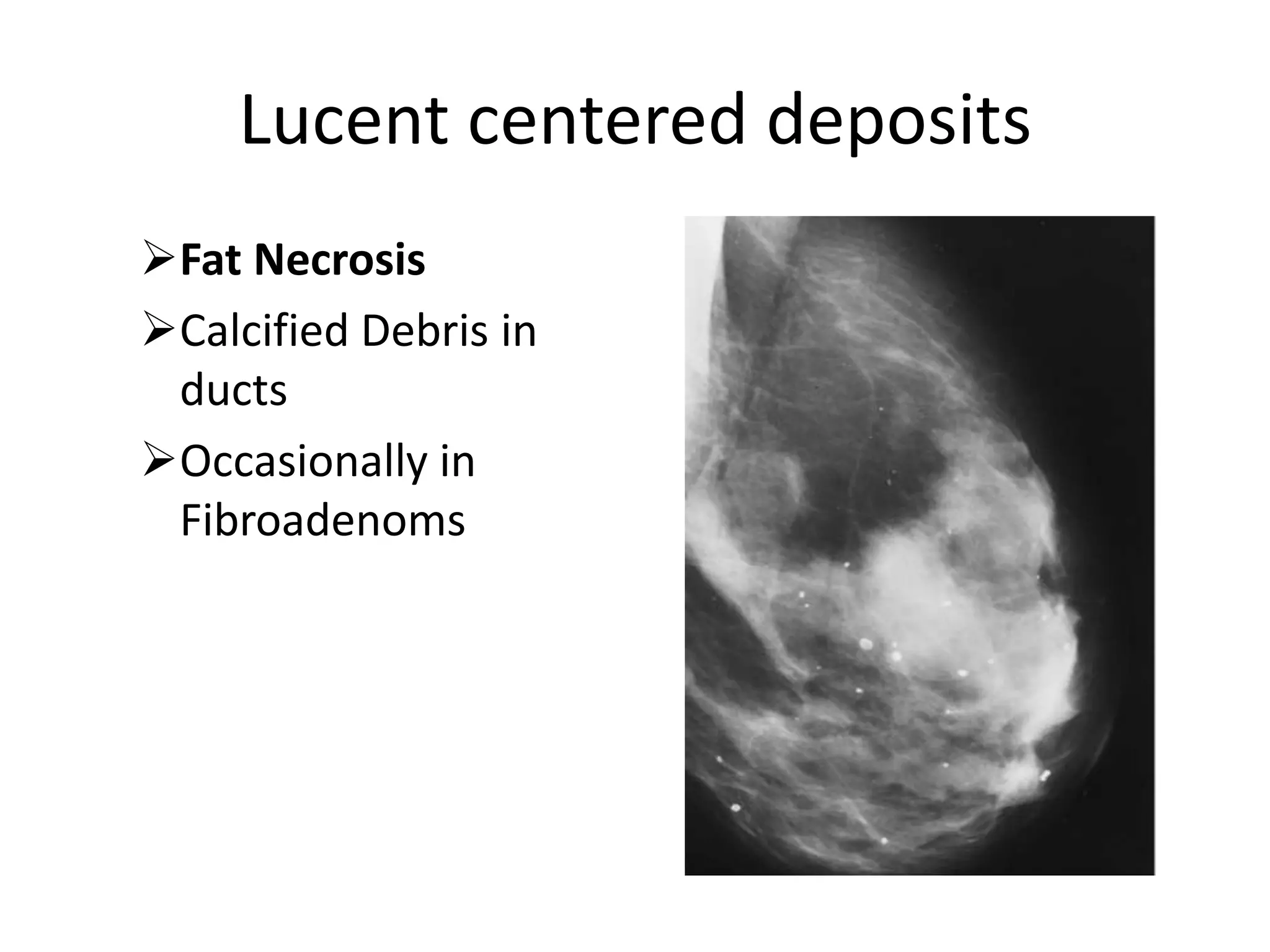
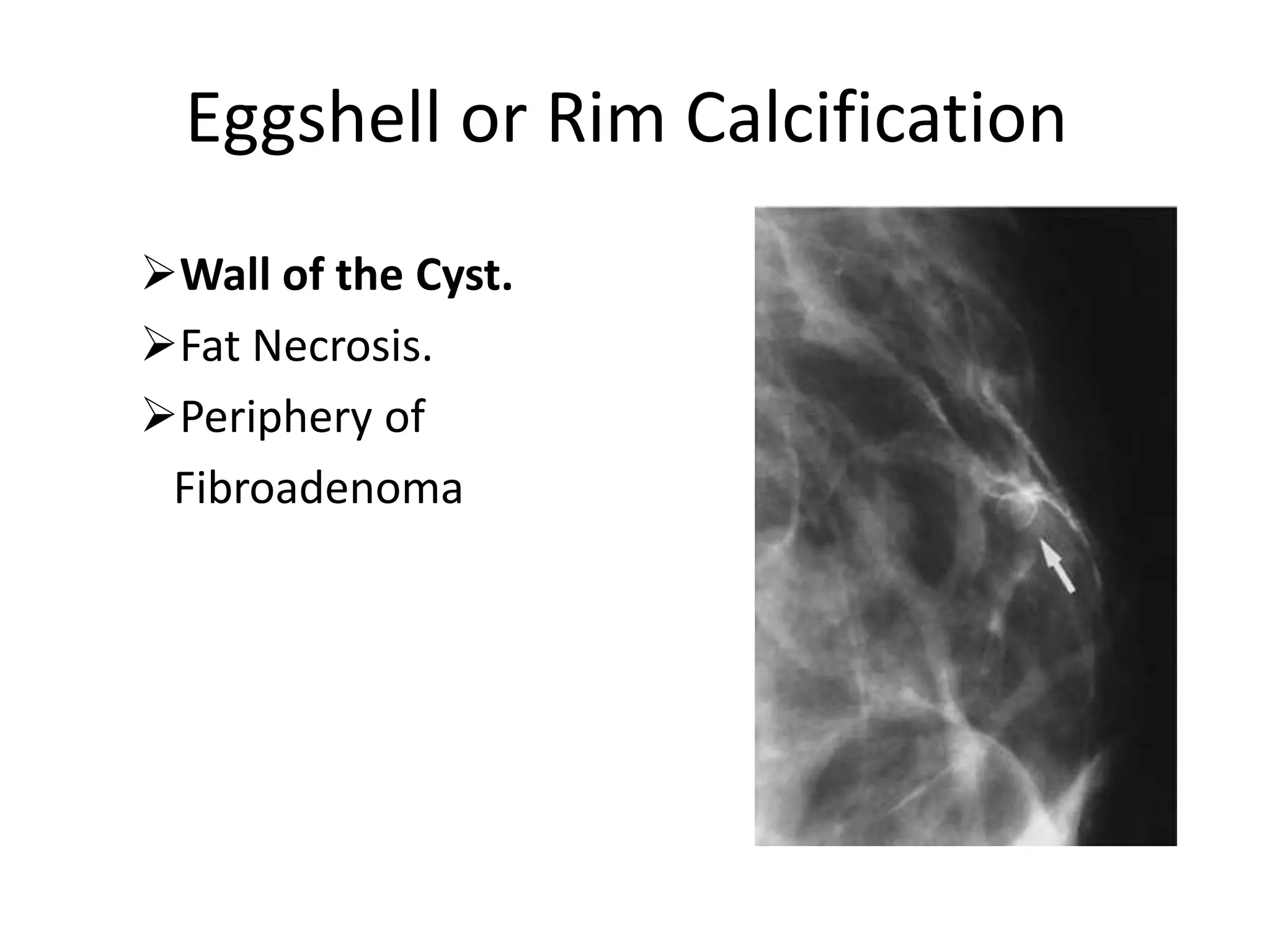
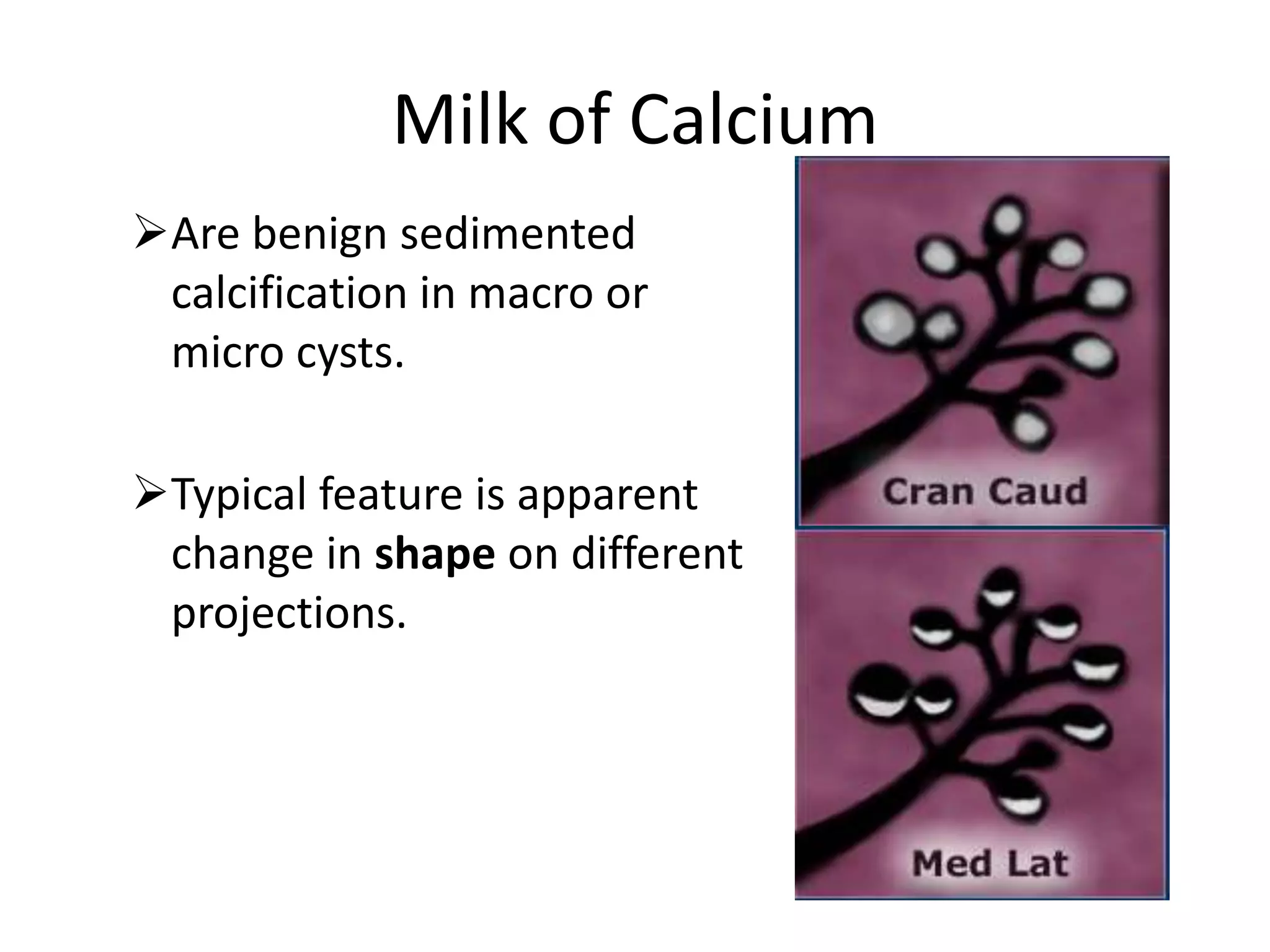
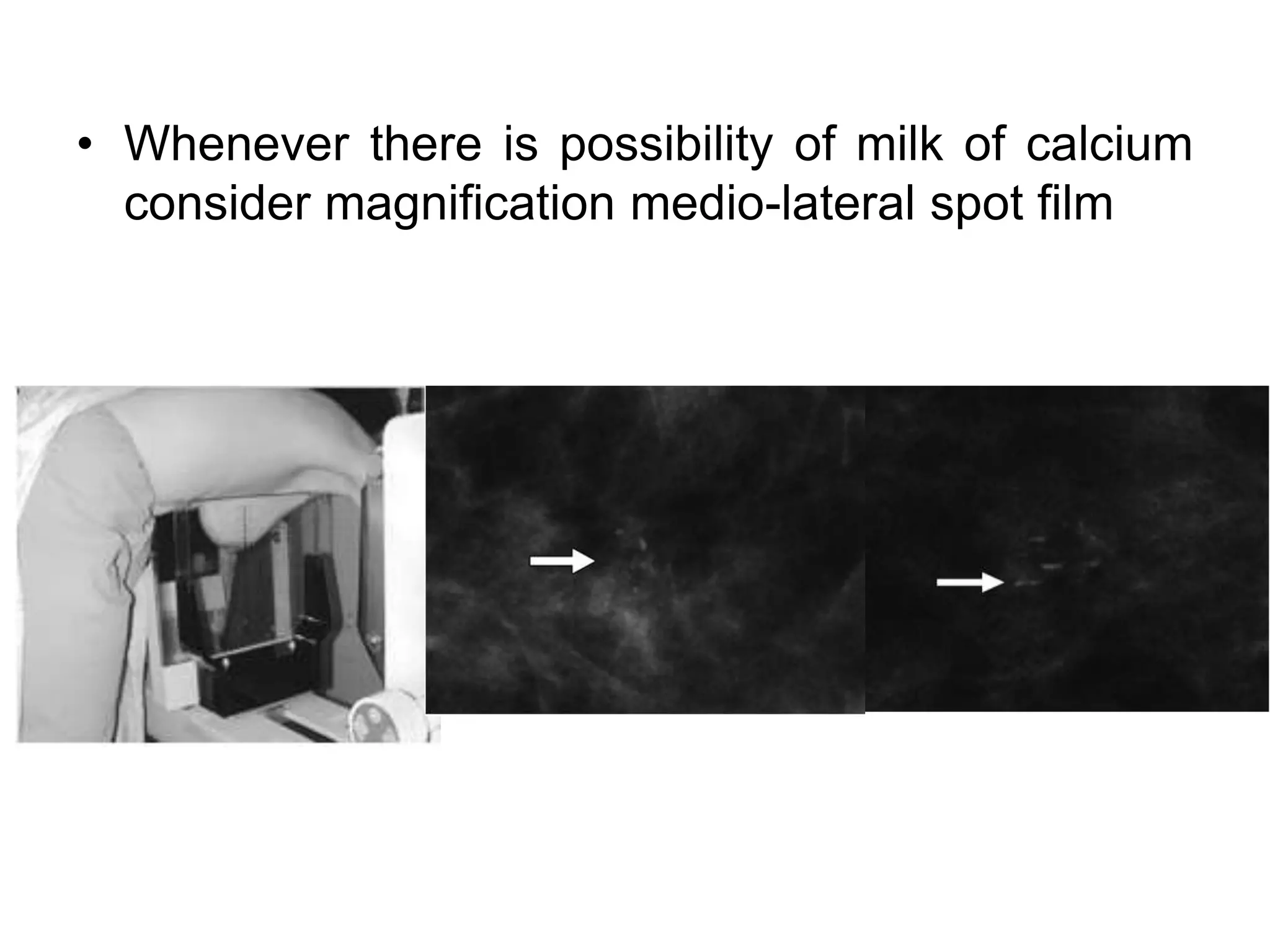
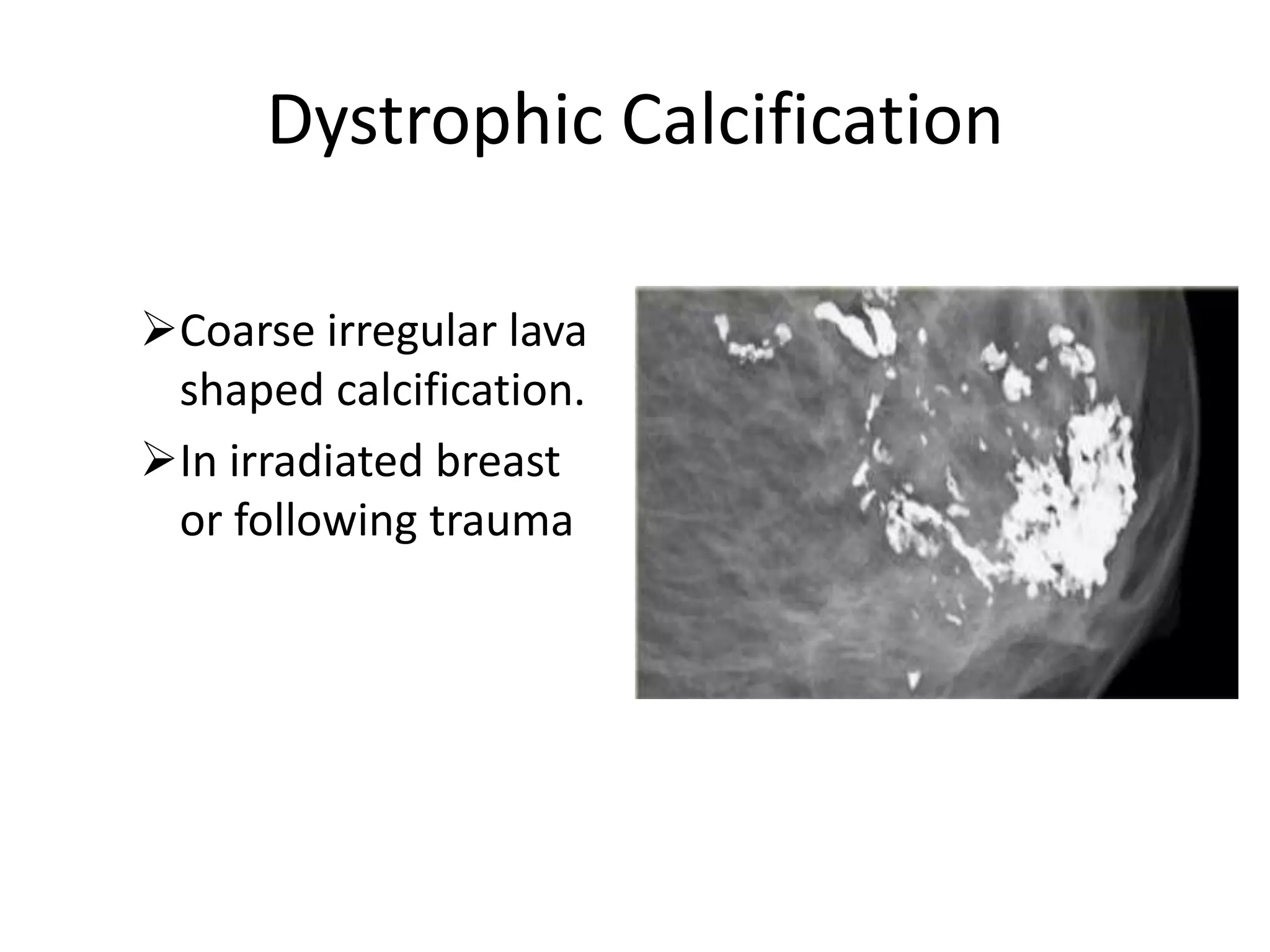
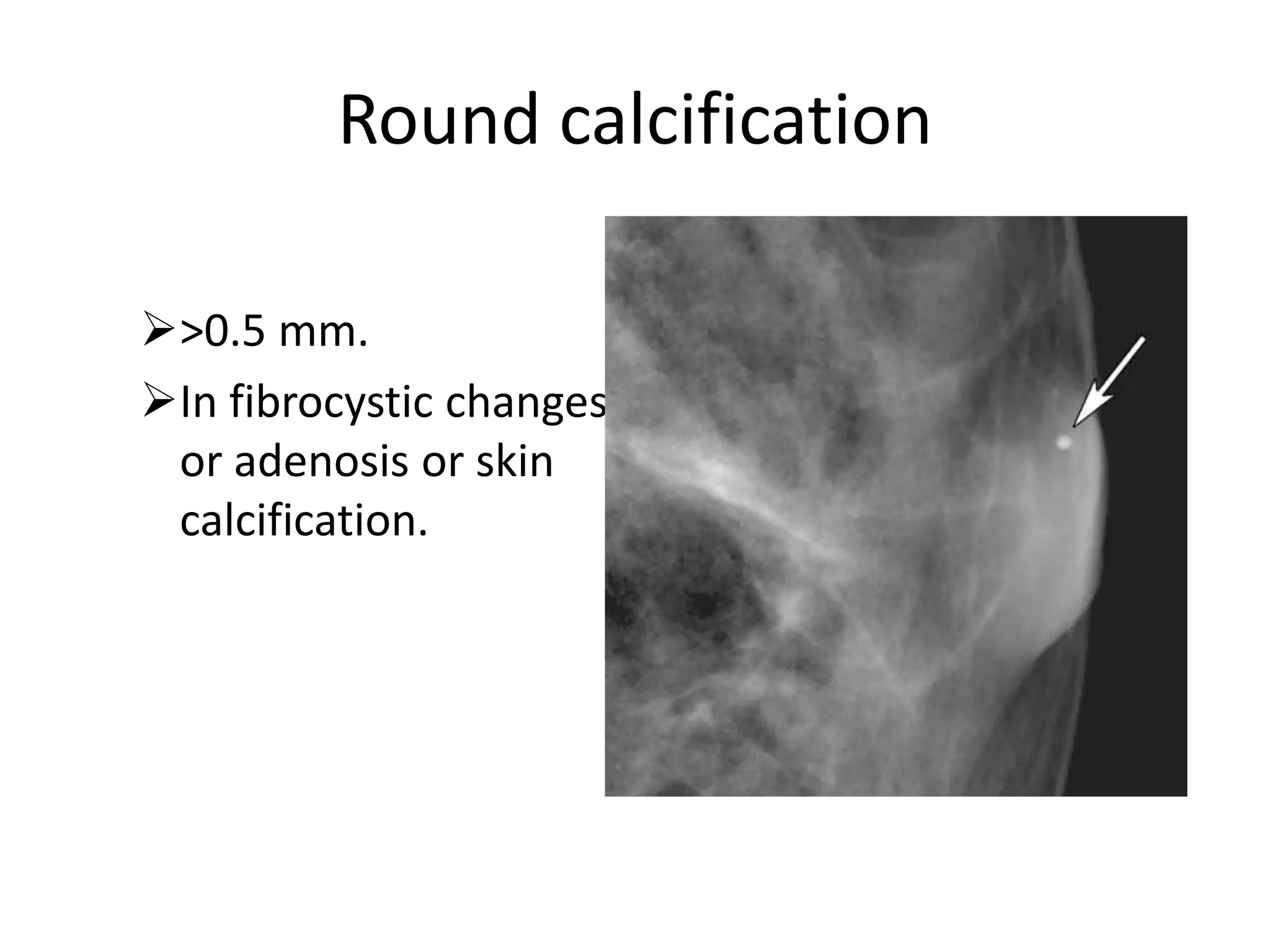
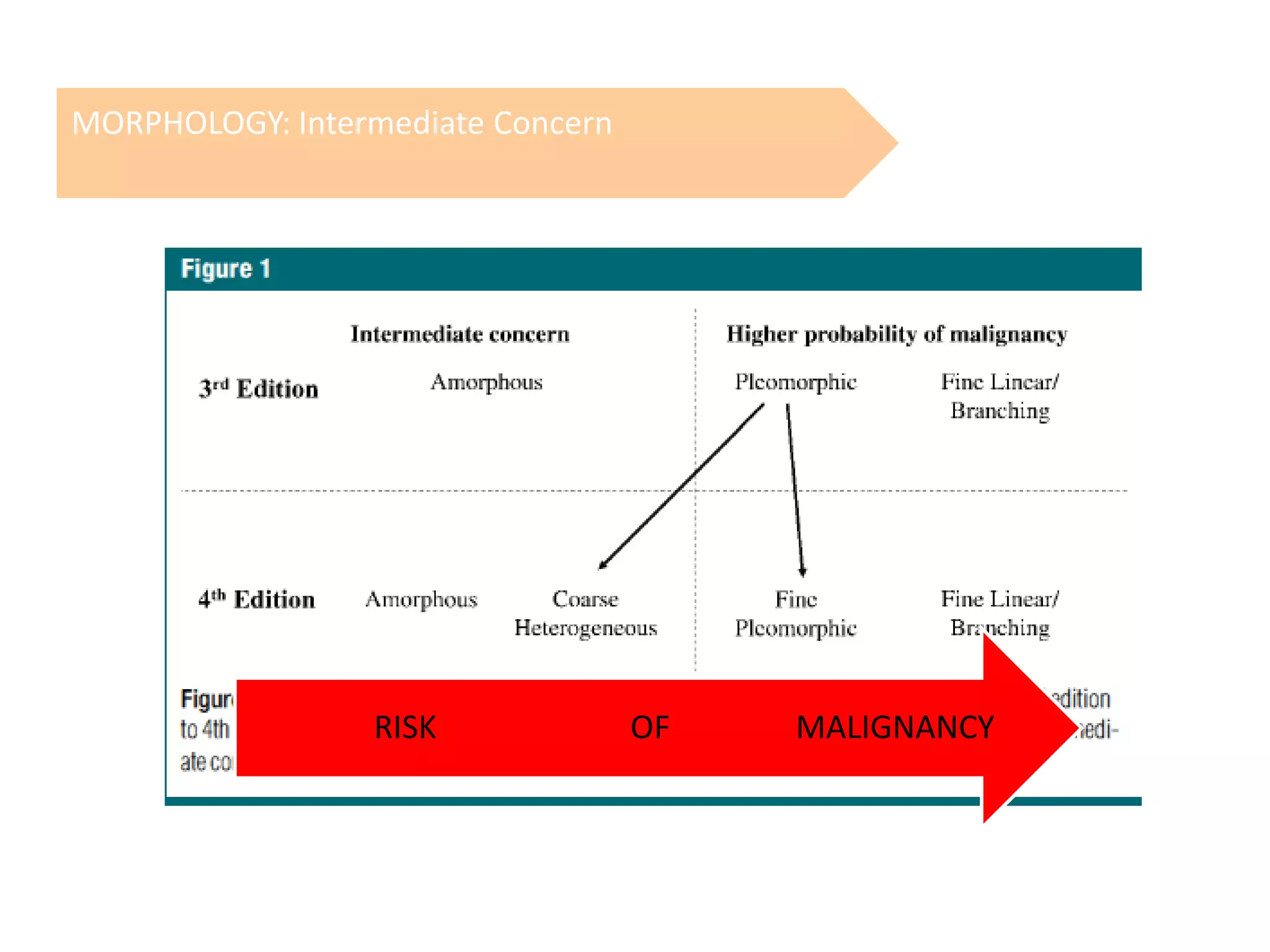
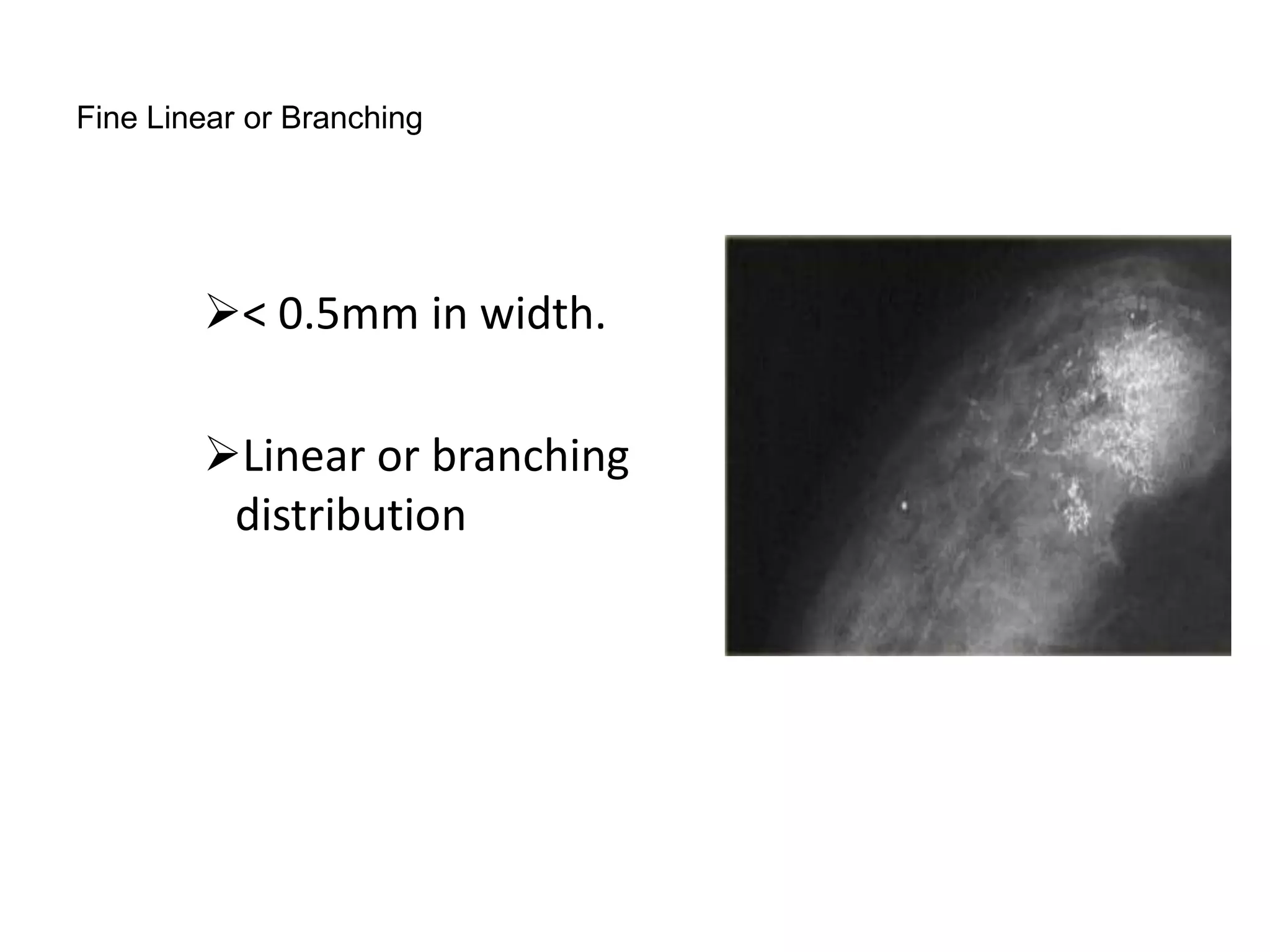
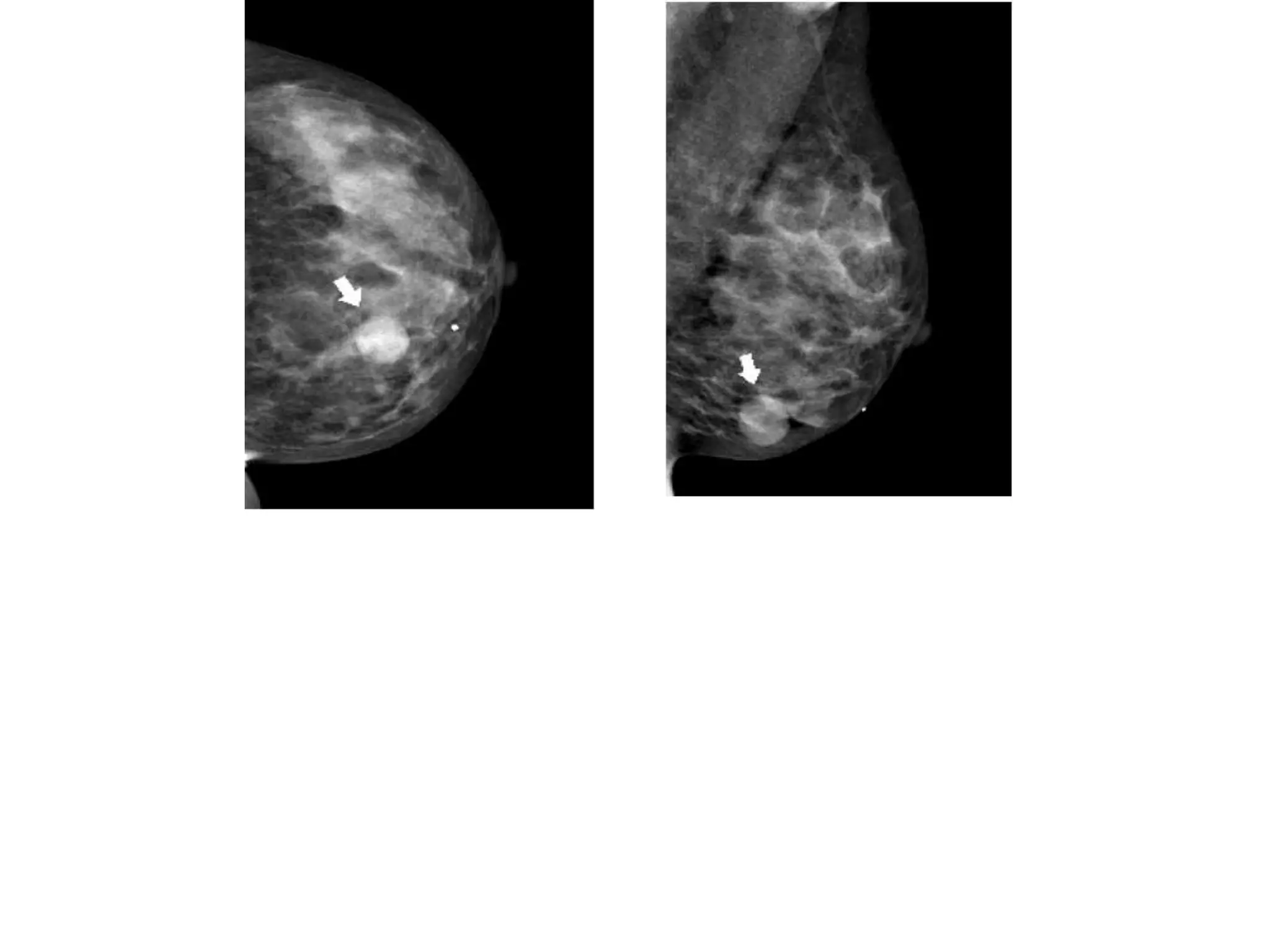
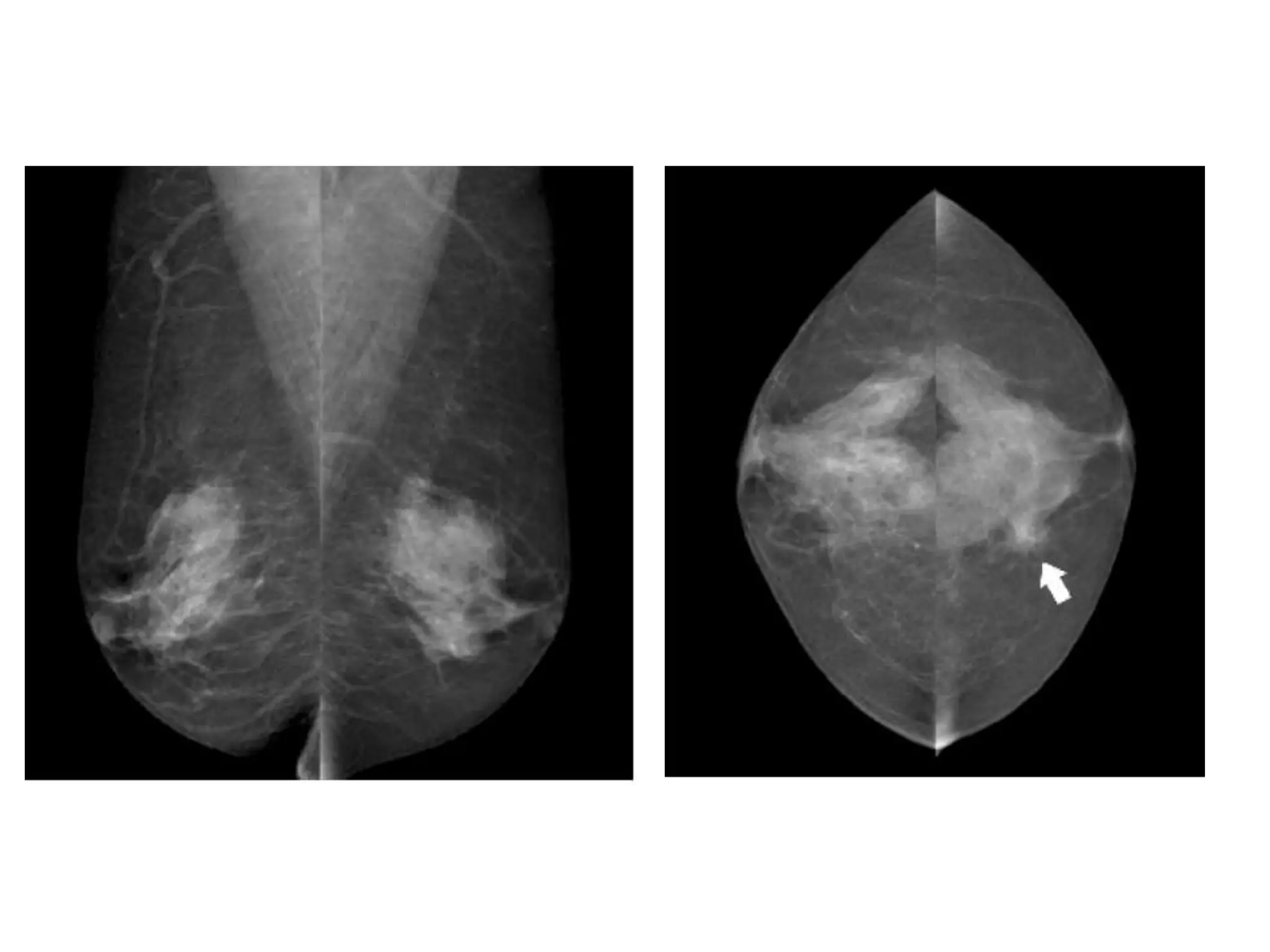
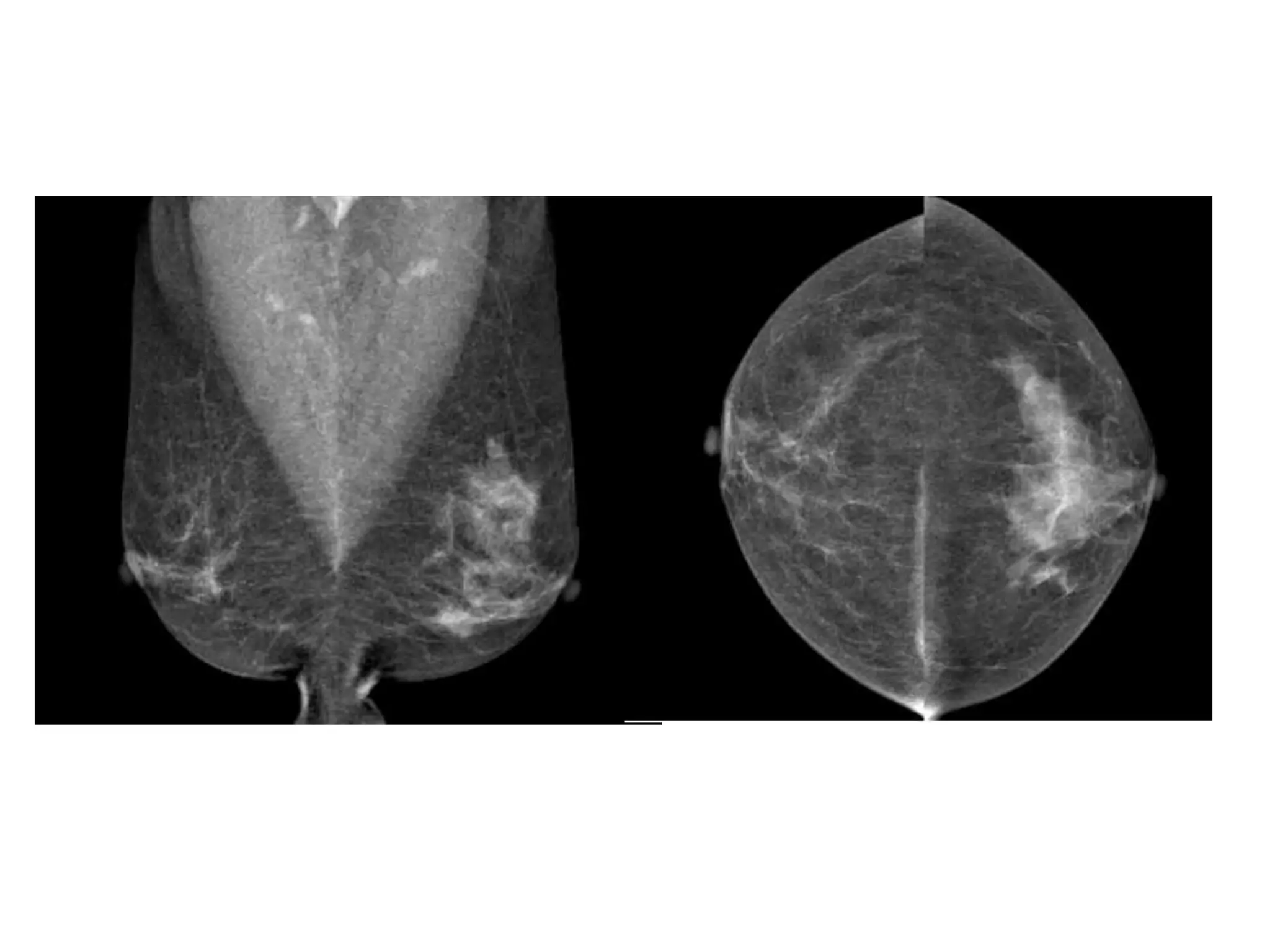
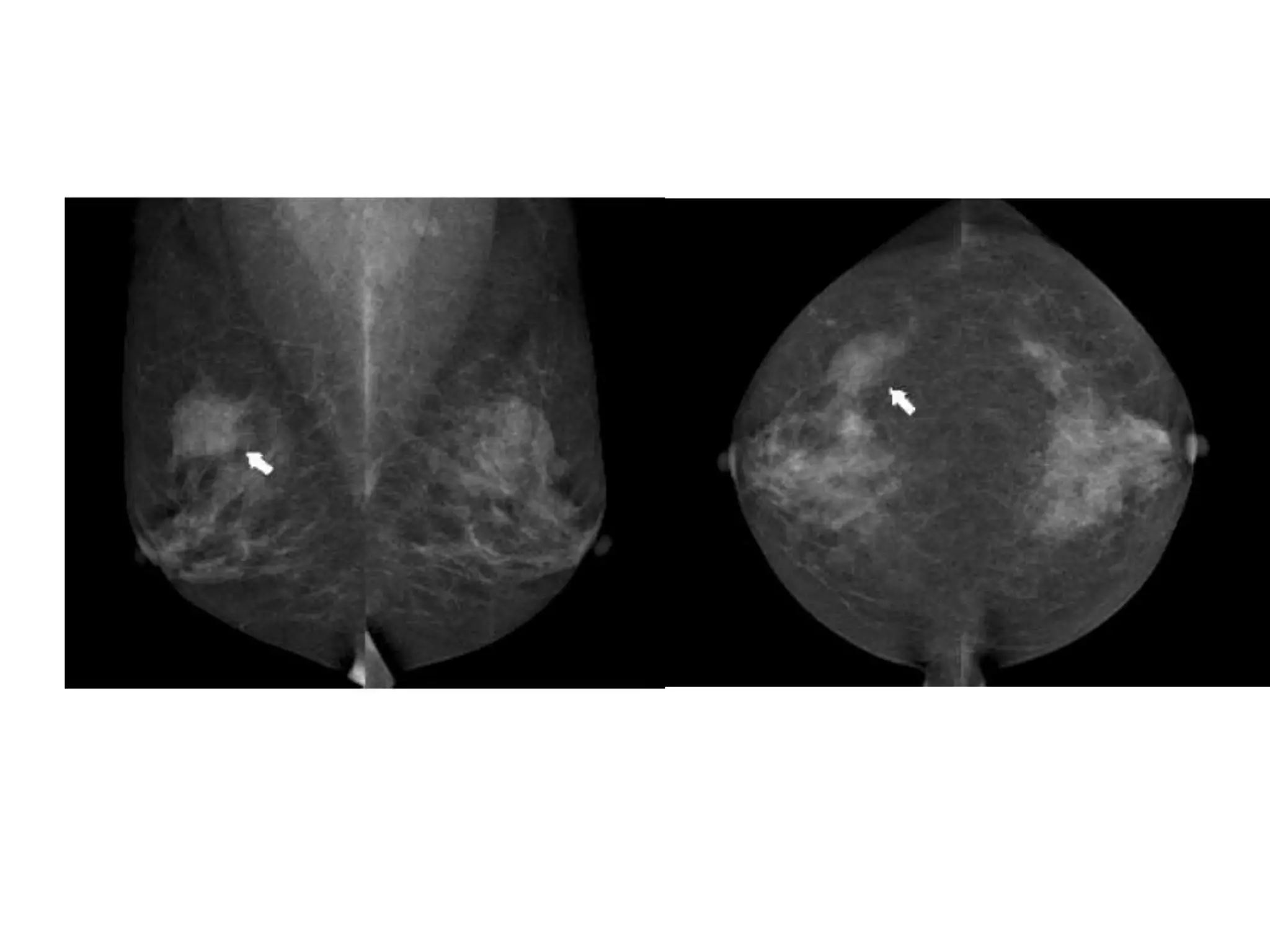
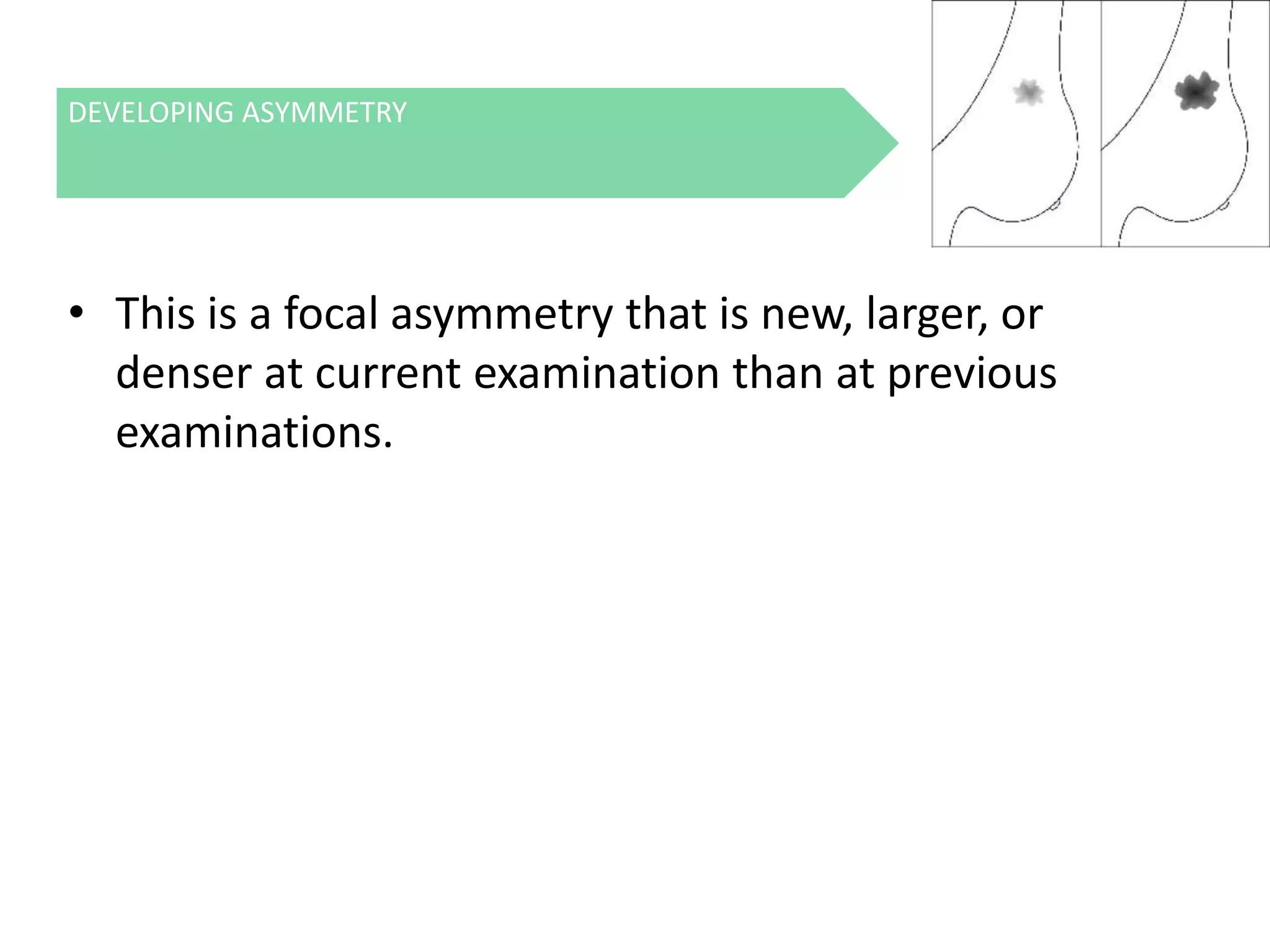
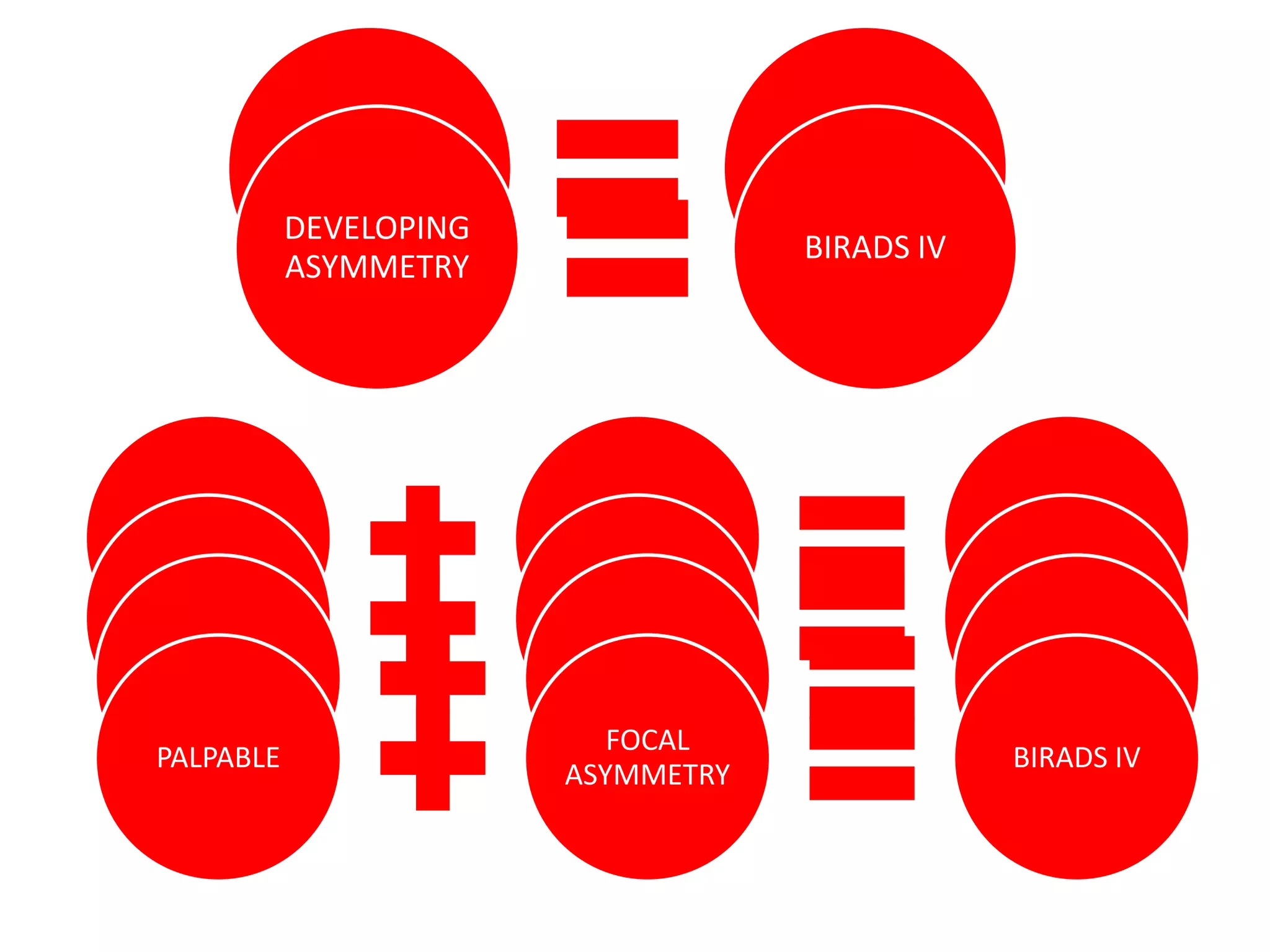
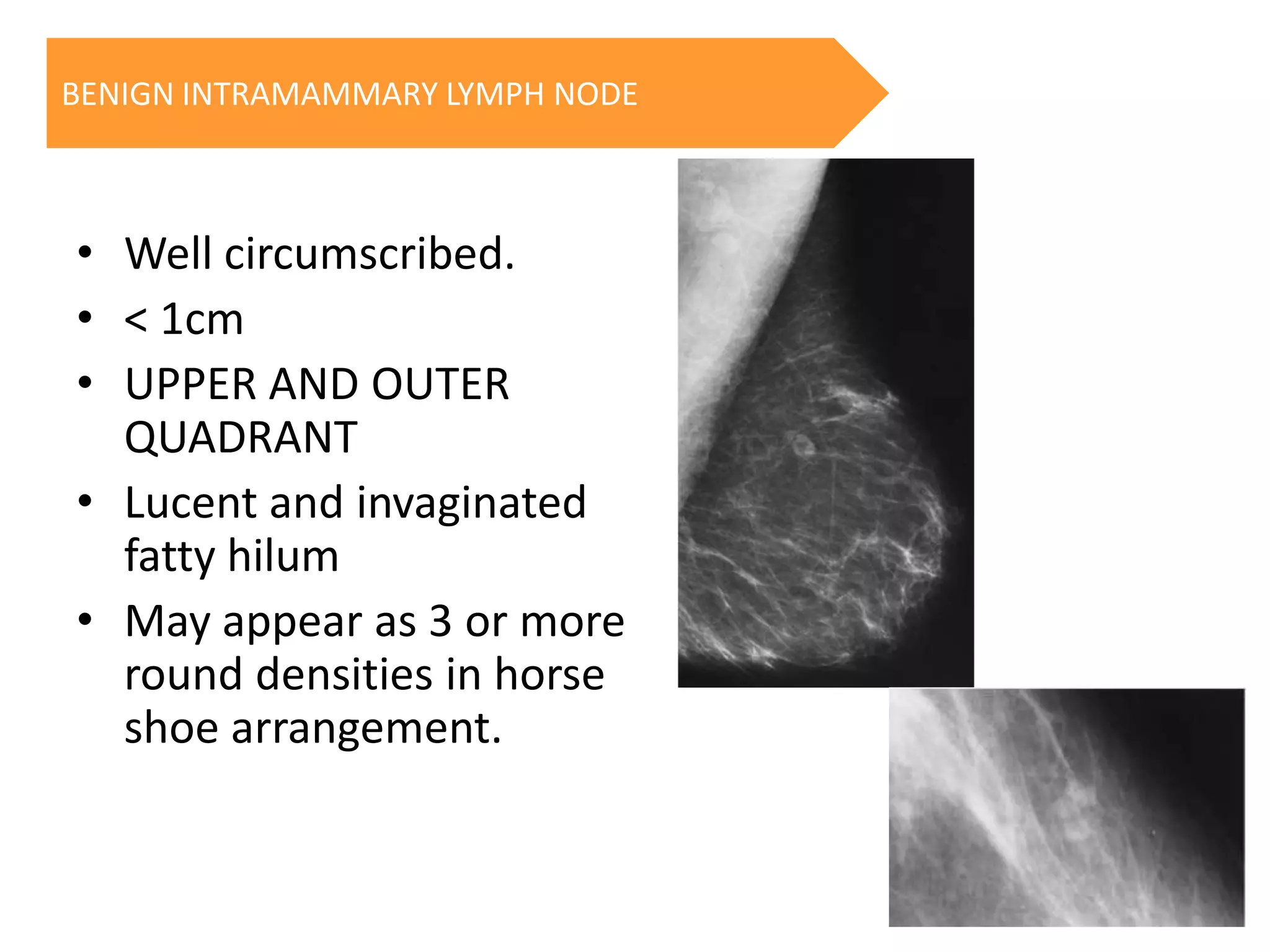
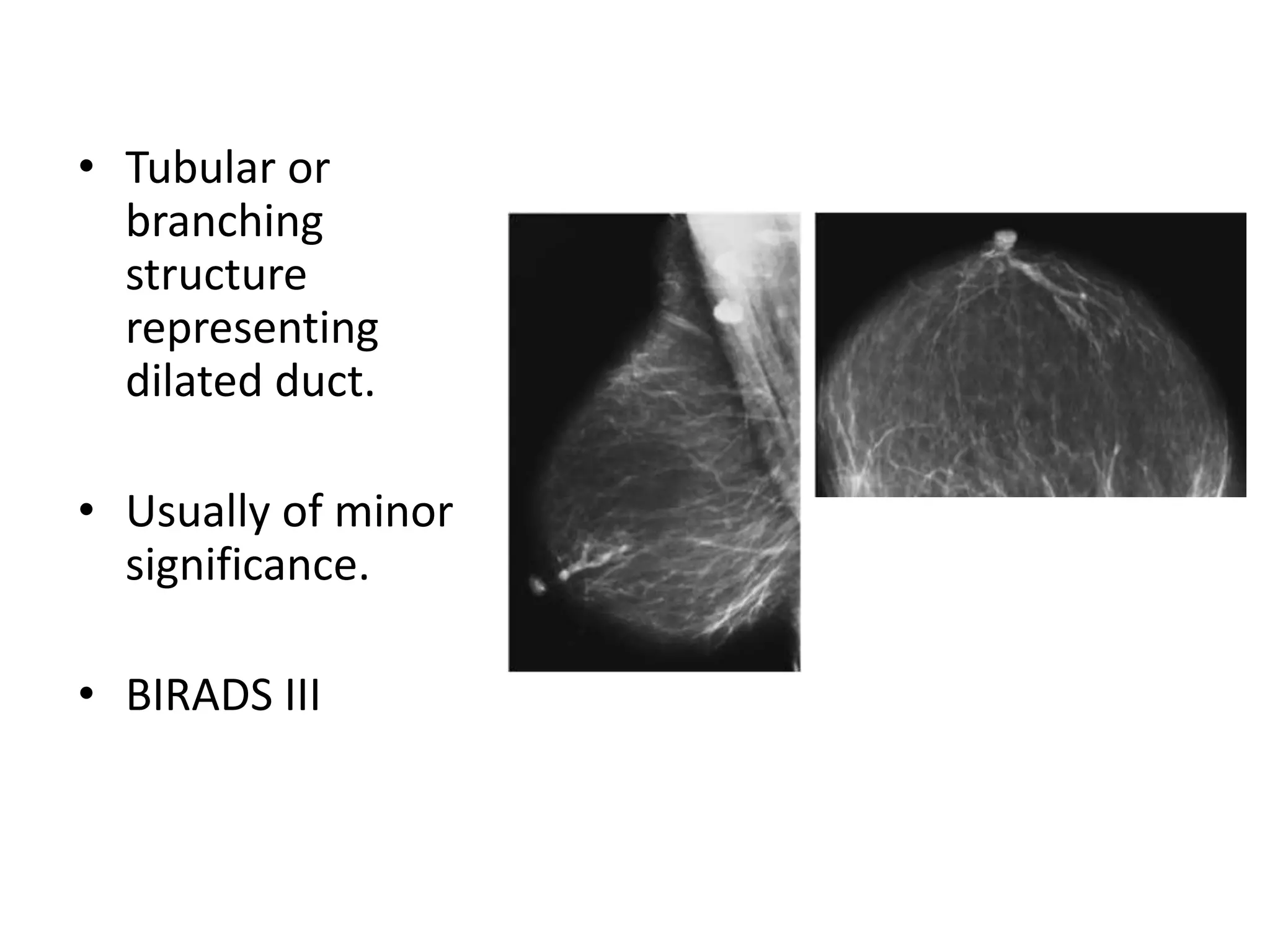
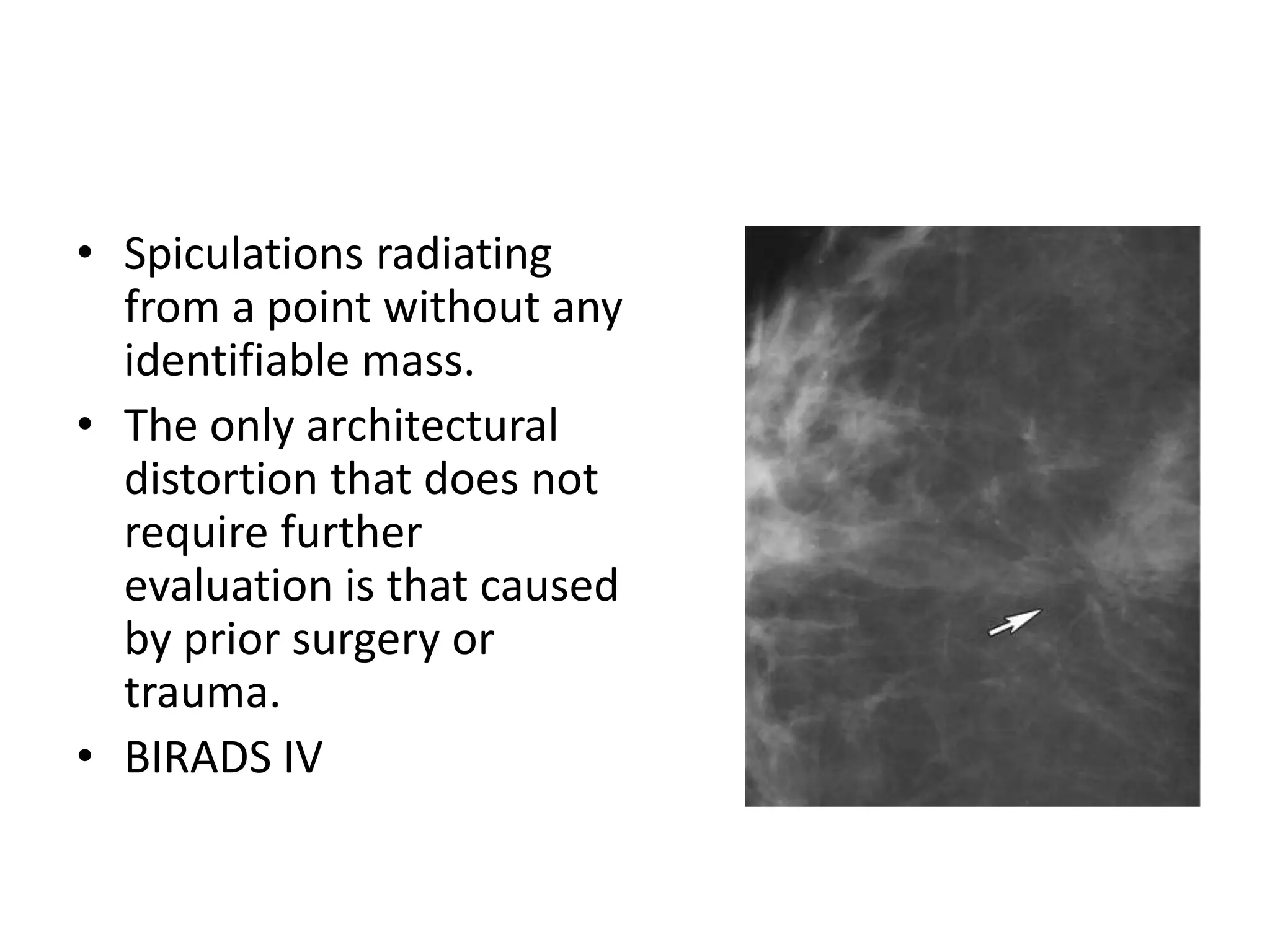
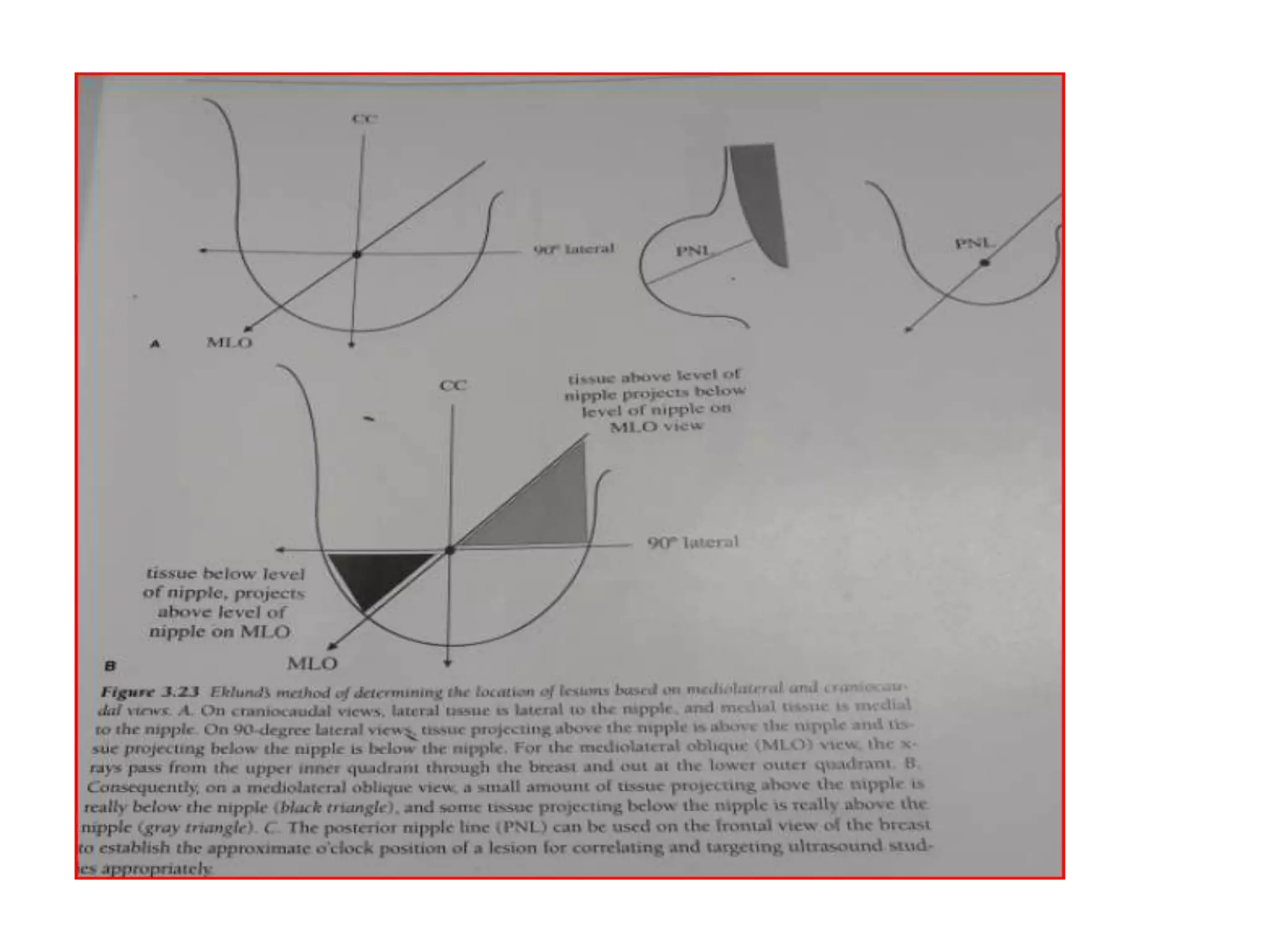
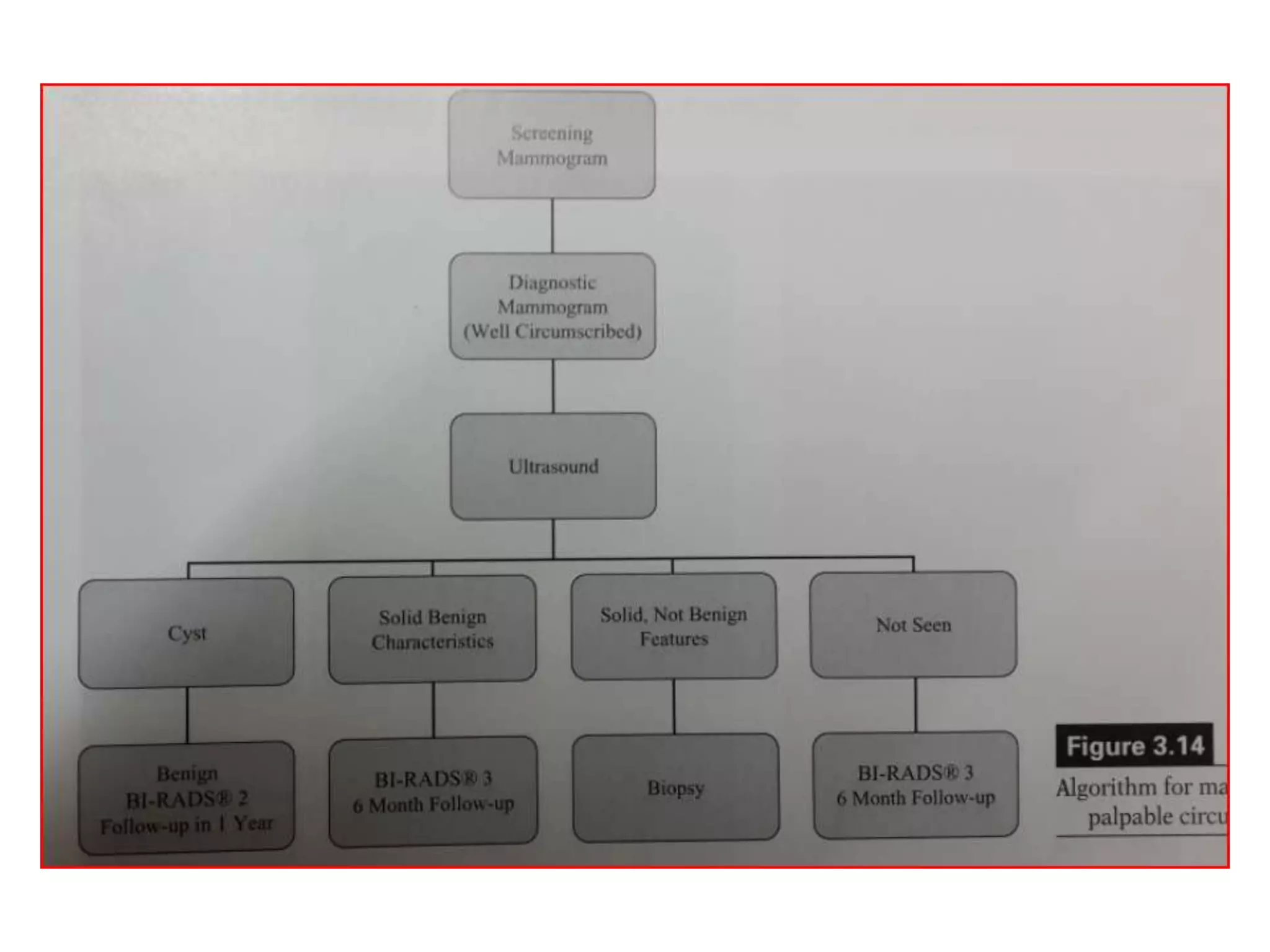
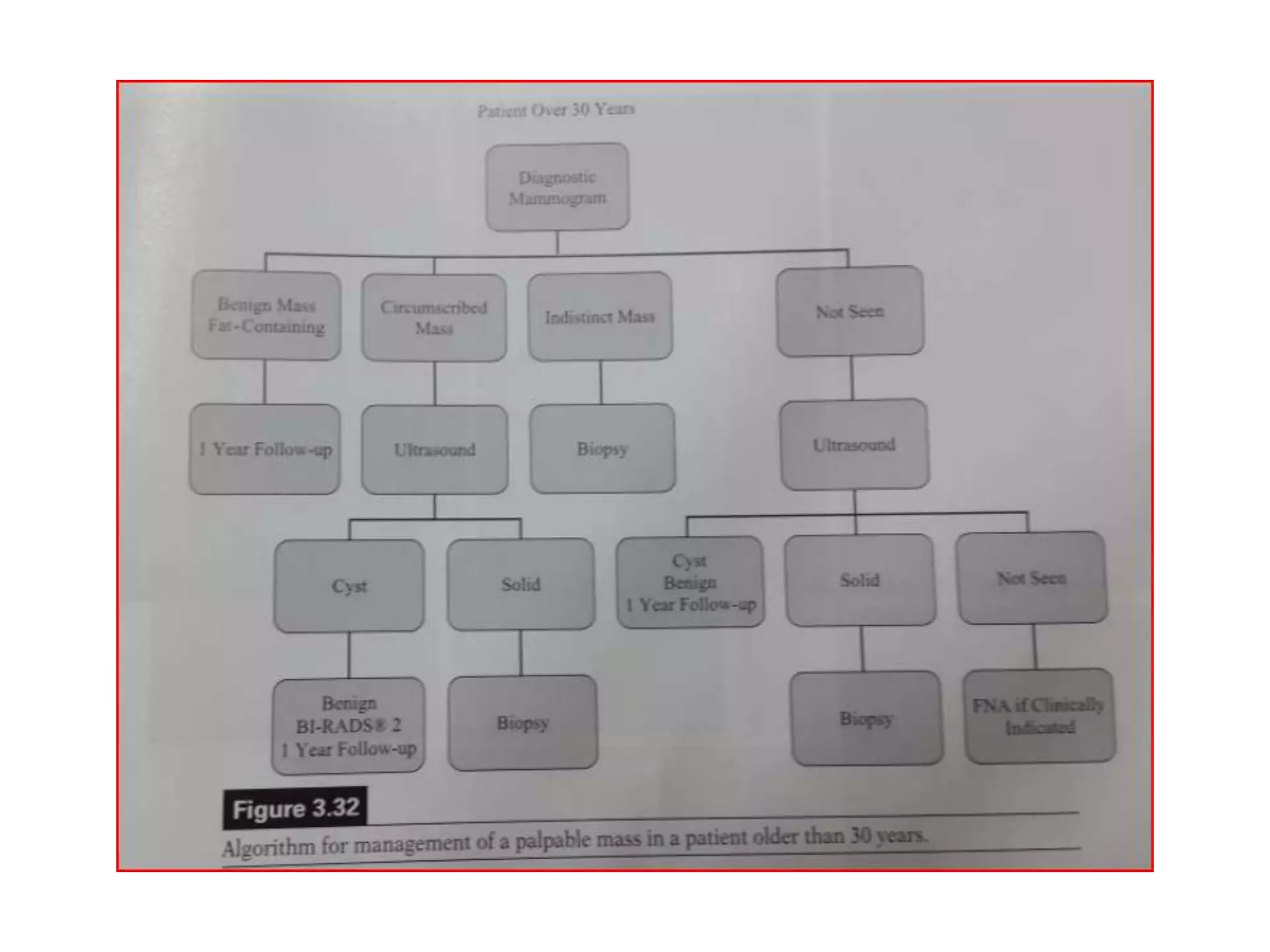
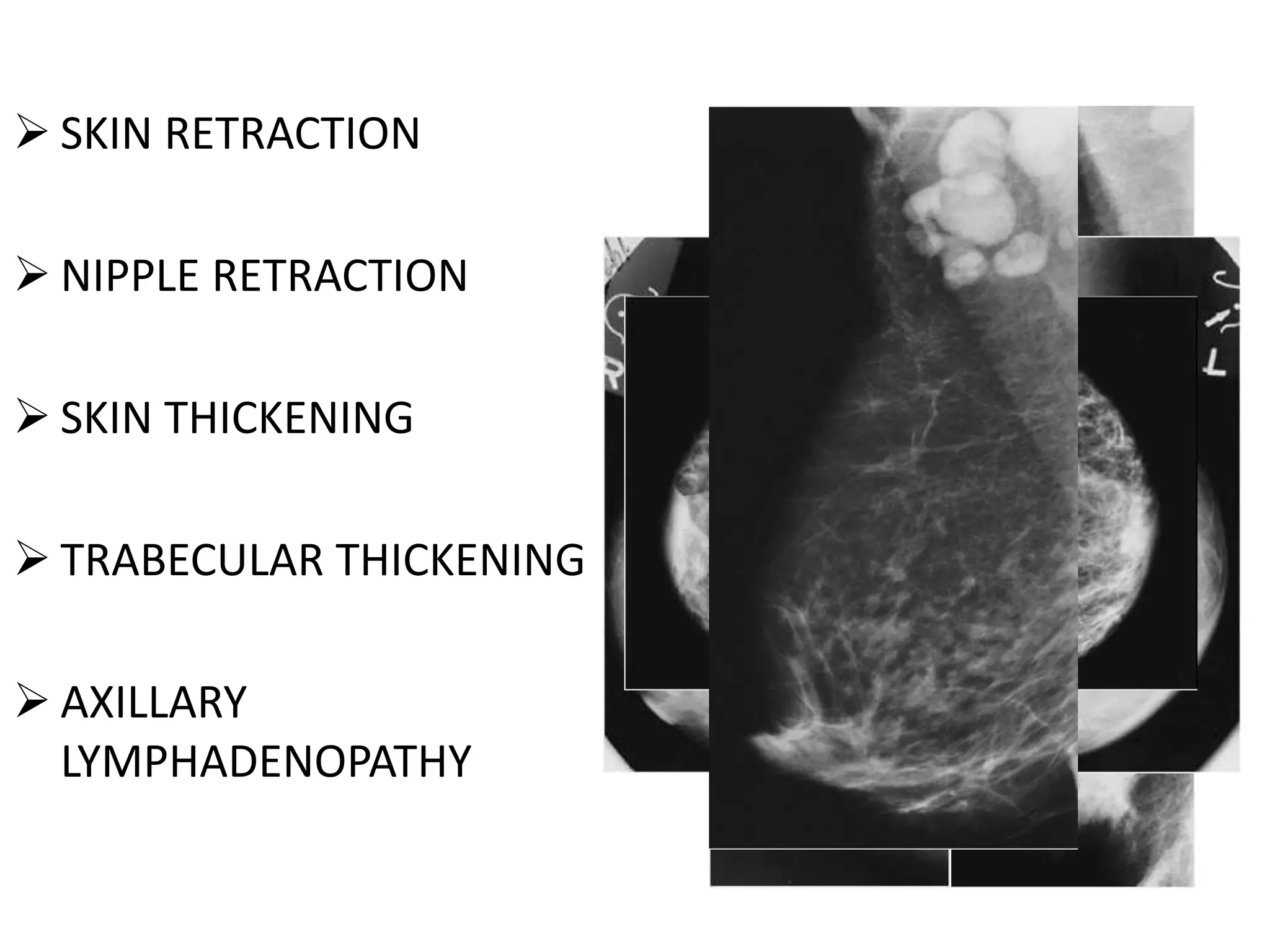
The document provides a detailed overview of breast anatomy and its imaging characteristics as seen in mammograms, categorized by the BI-RADS system. It describes the zonal anatomy of the breast, types of breast composition, and interpretations of mammographic findings, including benign and suspicious characteristics. The importance of assessing various factors such as mass shape, margins, and calcification types to evaluate anomalies and potential malignancy risk is emphasized.