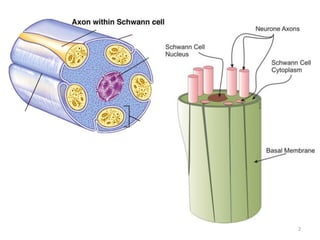
Malignant peripheral nerve sheath tumours (MPNST) are aggressive malignancies arising from peripheral nerves, characterized by a high rate of local recurrence and poor prognosis, especially in patients with neurofibromatosis type 1 (NF1). Diagnosis involves imaging techniques and histopathological analysis, with treatment primarily consisting of complete surgical excision, often combined with adjuvant radiation and chemotherapy. MPNST typically presents with neurological symptoms and may metastasize to distant organs, necessitating careful management to preserve nerve function and improve outcomes.