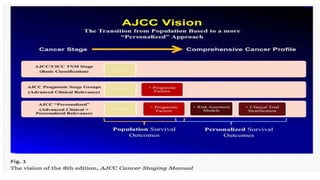
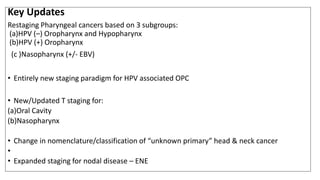
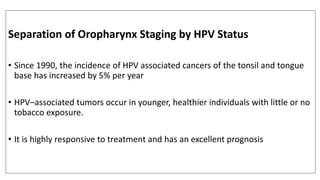
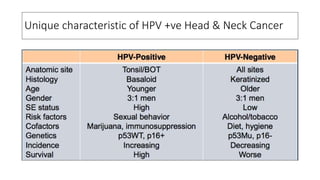
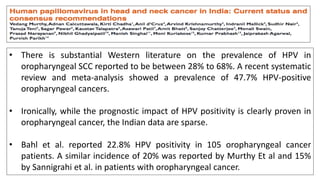
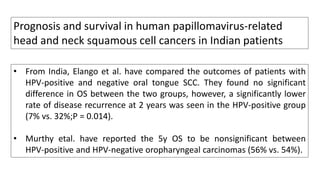
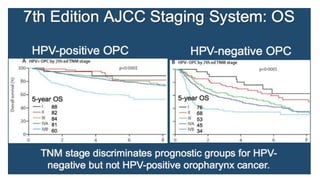
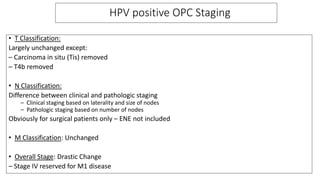
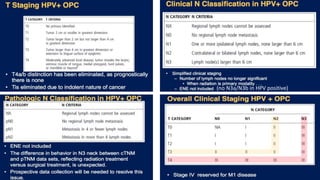
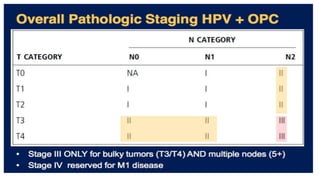
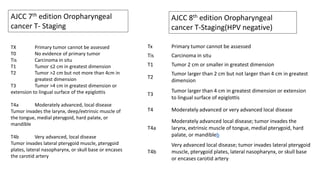
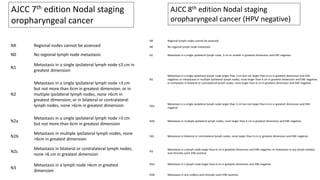
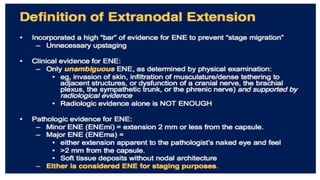
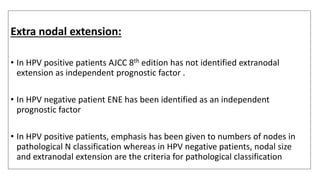
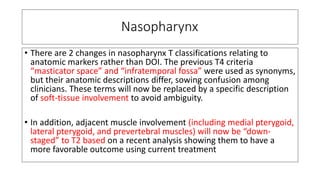
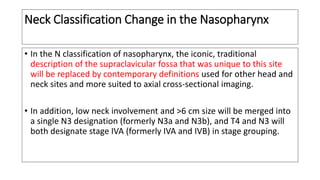
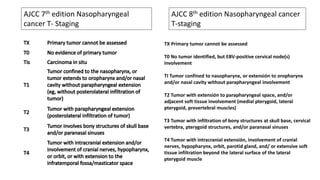
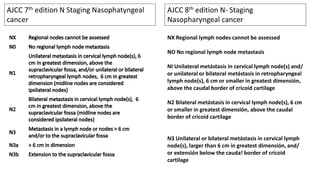
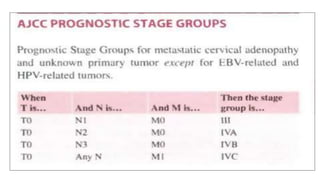
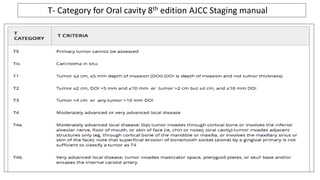
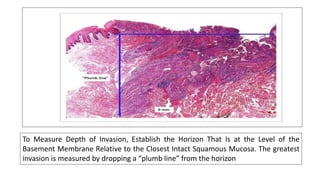
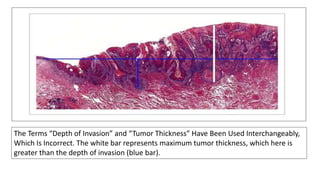
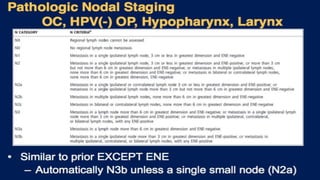
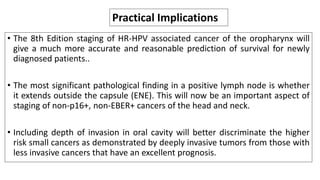
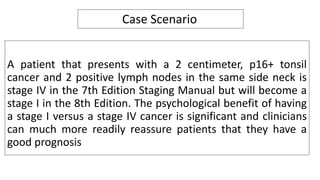
The 8th edition of the AJCC cancer staging manual introduces several changes to the staging of head and neck cancers. Key changes include separating the staging of oropharyngeal cancer based on HPV status, with HPV-positive cancers now staged differently and having a better prognosis. The TNM classification for nasopharyngeal cancer and nodal classifications for various head and neck cancers were also updated. These changes aim to provide oncologists with a more accurate prediction of patient outcomes and guide treatment planning.