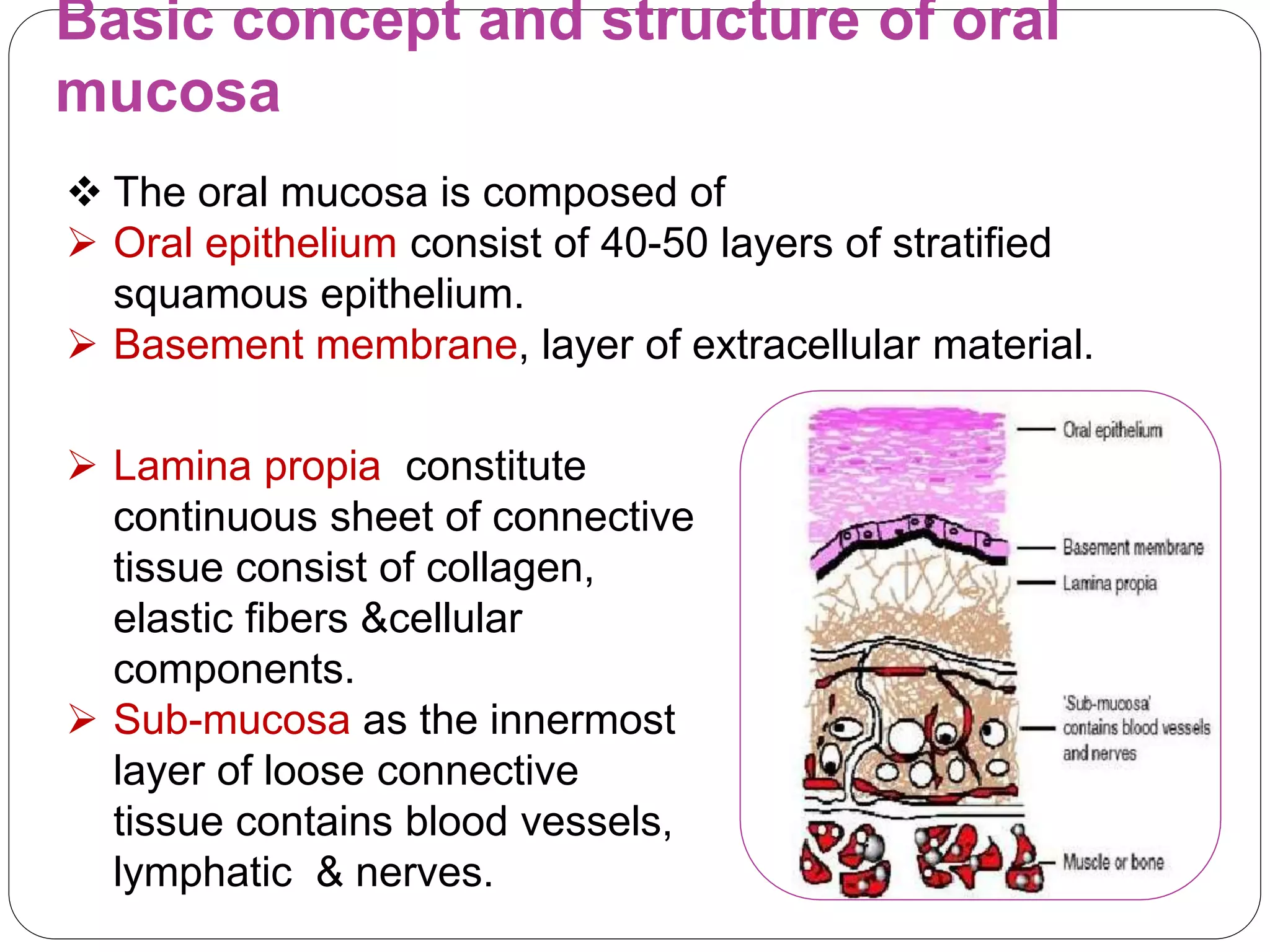
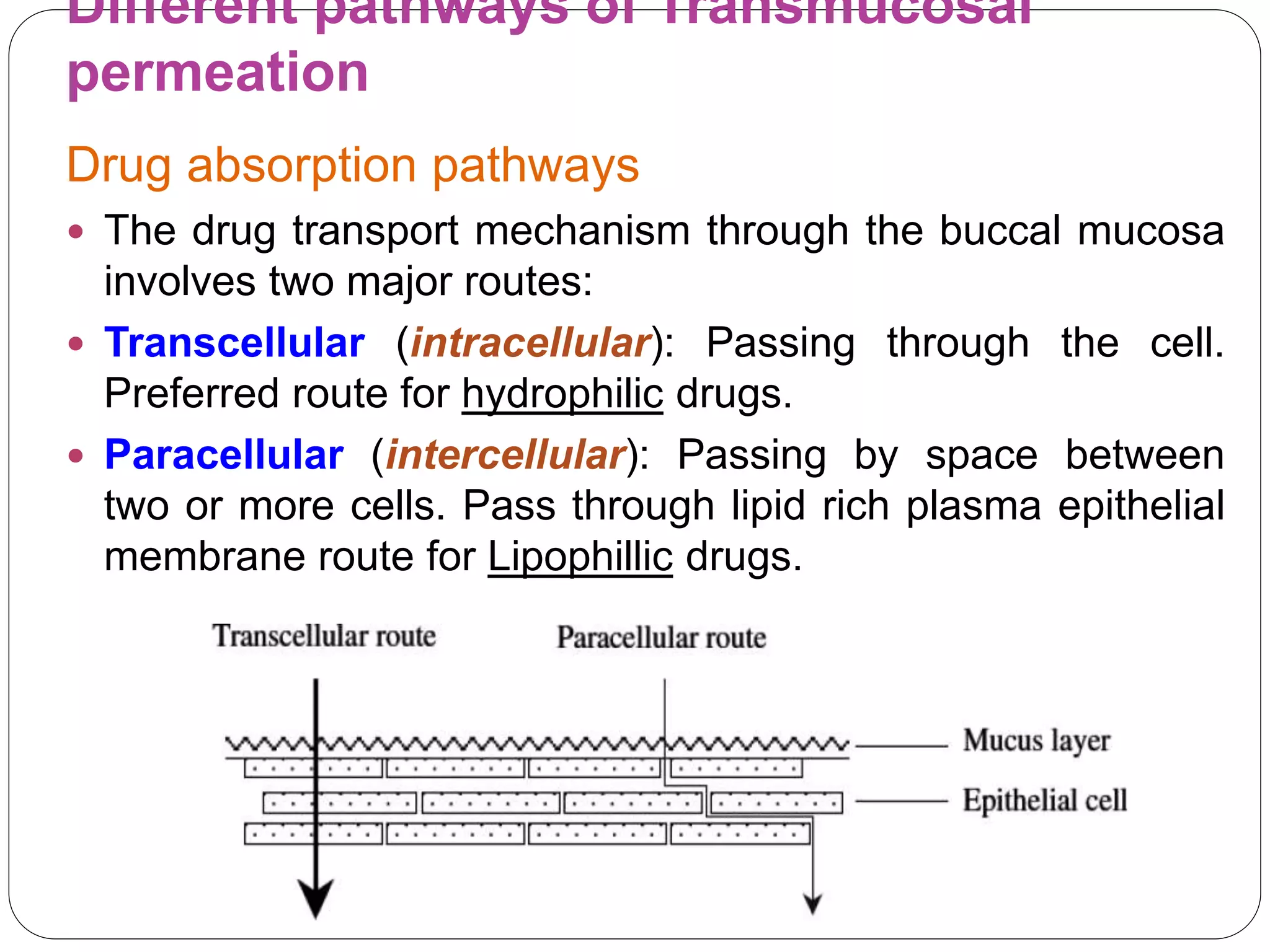
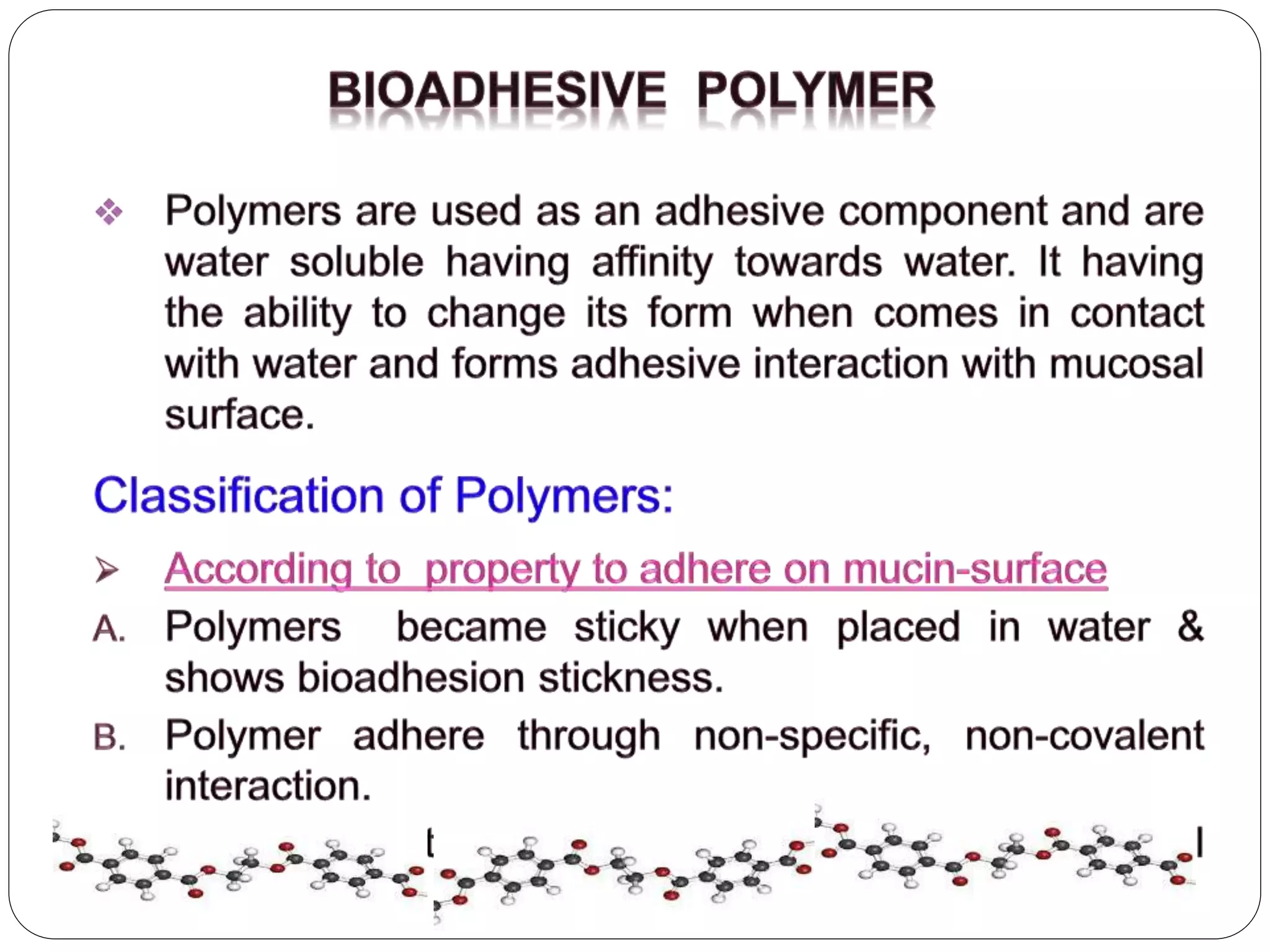
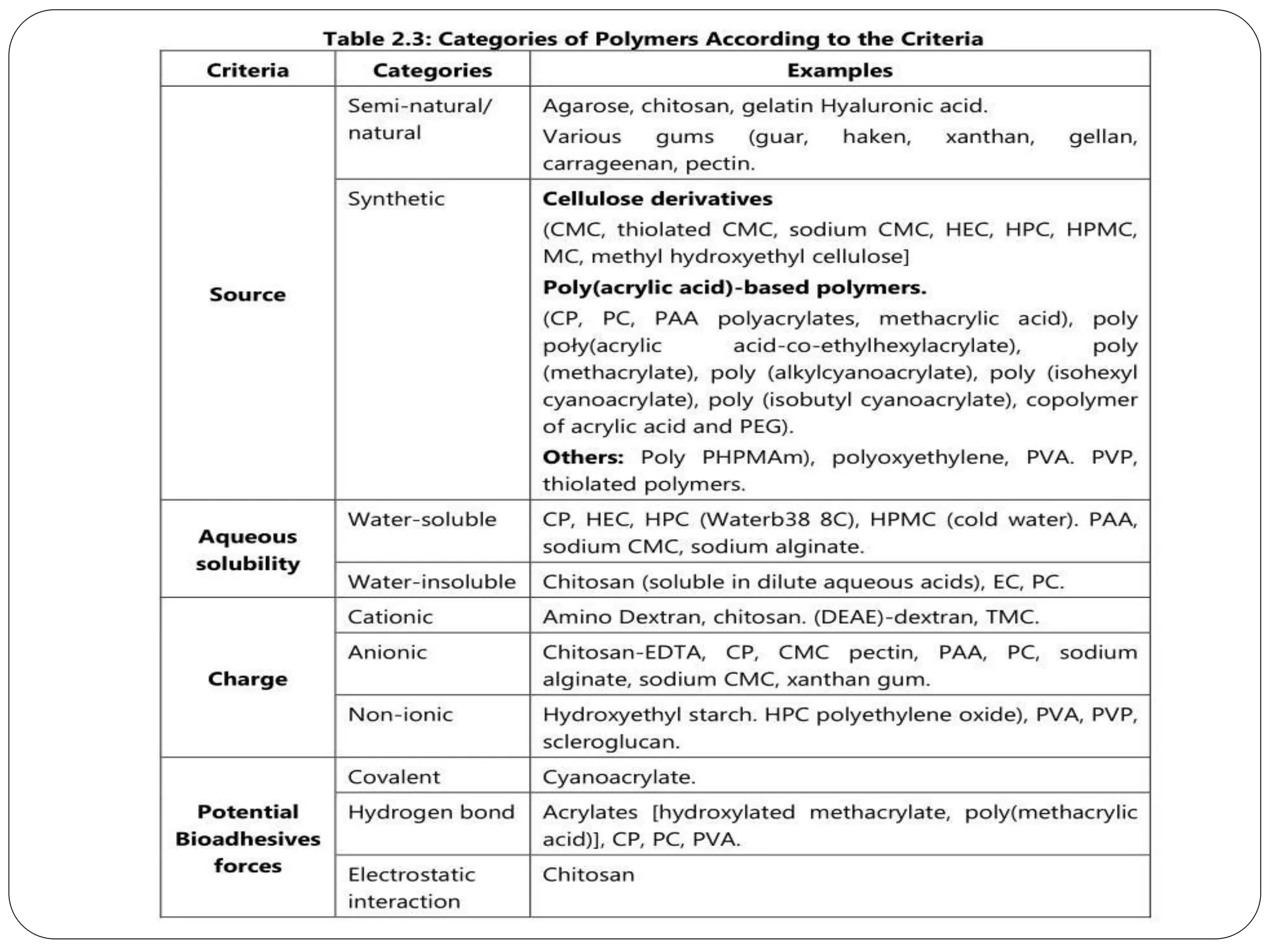
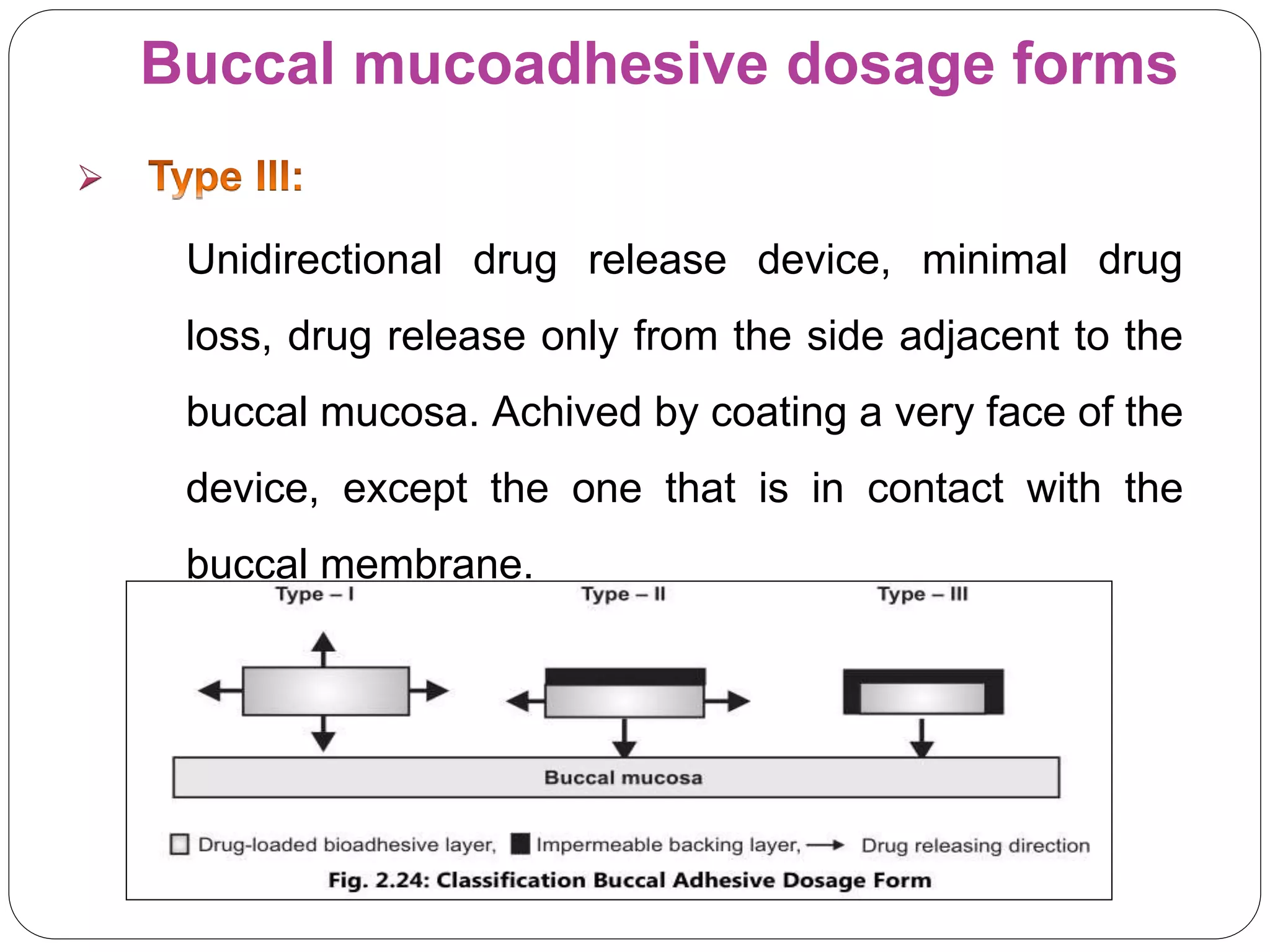
BDDS refers to drug delivery systems that administer drugs through the buccal mucosa in the oral cavity. The buccal mucosa has a rich blood supply and provides a non-invasive route for systemic drug delivery with advantages like rapid absorption and avoidance of first-pass metabolism. Formulations can be designed as solids, semisolids, or liquids depending on the drug properties and desired release characteristics. The drug permeates through the buccal mucosa via transcellular or paracellular routes to enter systemic circulation. Buccal delivery offers an alternative to oral and parenteral routes for certain drugs.