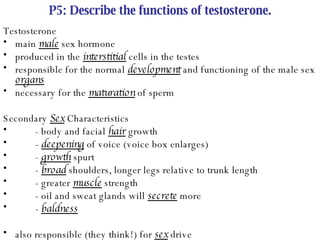
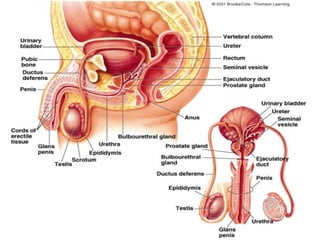
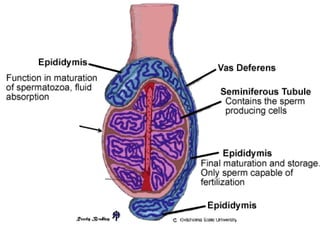
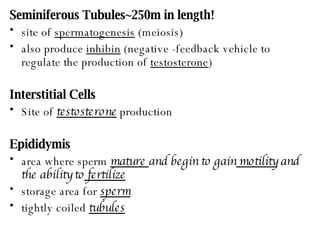
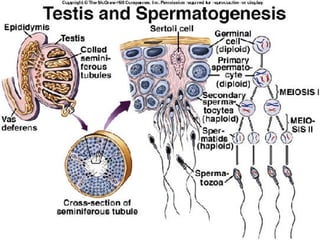
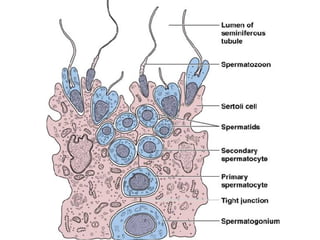
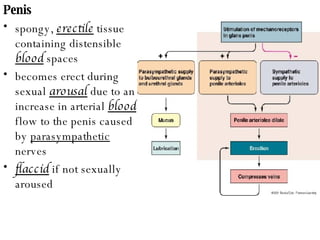
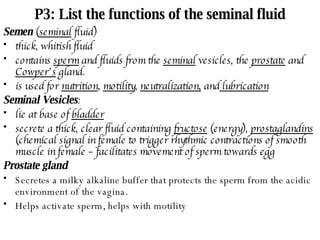
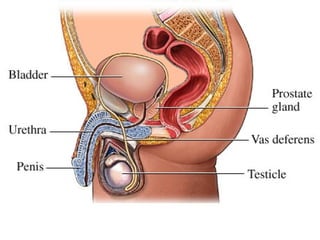
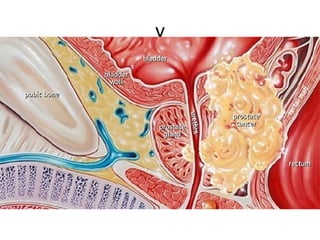
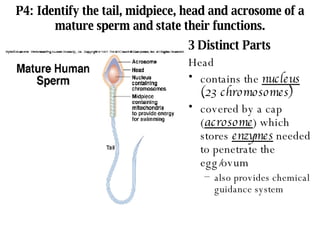
The male reproductive system produces sperm and testosterone. The testes produce sperm in the seminiferous tubules and testosterone with the interstitial cells. Sperm mature in the epididymis and are stored in the vas deferens. During ejaculation, sperm are mixed with fluids from the seminal vesicles, prostate, and Cowper's glands and travel through the urethra. Testosterone controls male secondary sex characteristics and supports sperm production.
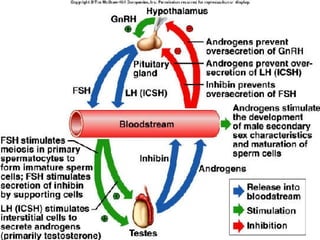
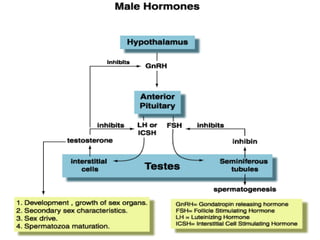
![P6: Demonstrate a knowledge of the control of testosterone levels by the endocrine system . Hormonal Regulation in Males hypothalamus secretes gonadotropic releasing hormone (GnRH) GnRH stimulates the anterior pituitary to secrete the gonadotropic hormones: Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) [this is true of both males and females]](https://image.slidesharecdn.com/male-reproductive-system-11040/85/Male-Reproductive-system-19-320.jpg)