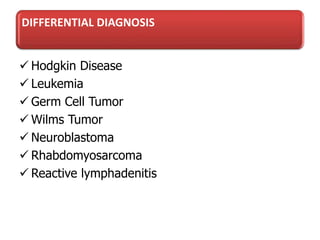
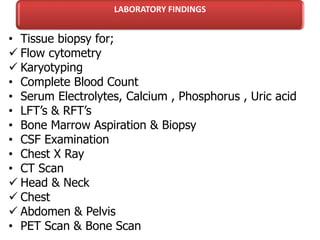
1. Lymphoma is the third most common childhood cancer and is broadly categorized into Hodgkin's disease and non-Hodgkin's lymphoma.
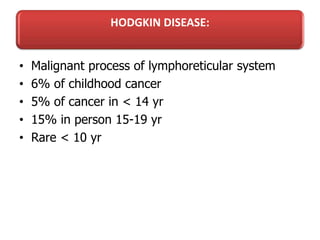
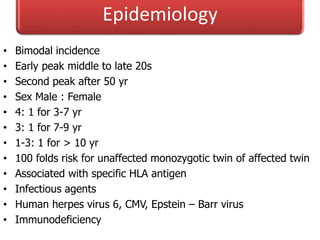
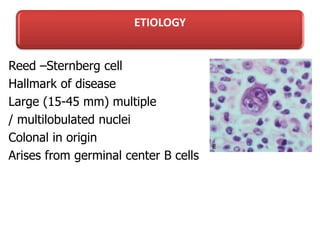
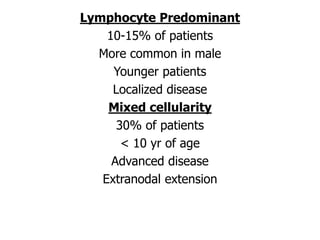
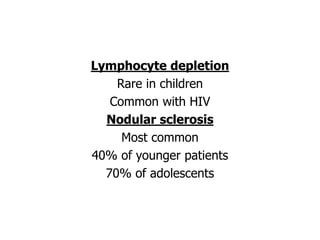
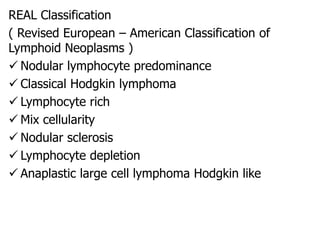
2. Hodgkin's disease is characterized by Reed-Sternberg cells and is further classified under Rye or REAL systems. Common subtypes include lymphocyte predominant, mixed cellularity, and nodular sclerosis.
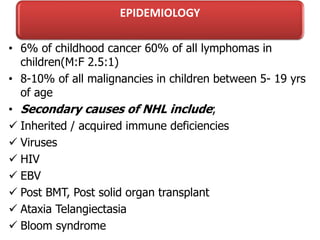
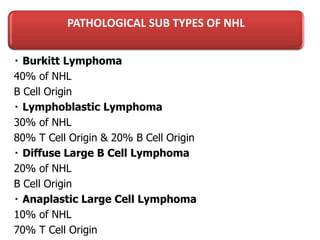
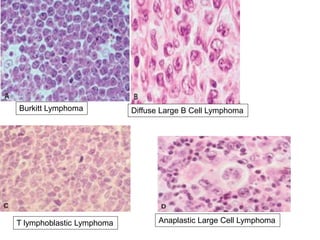
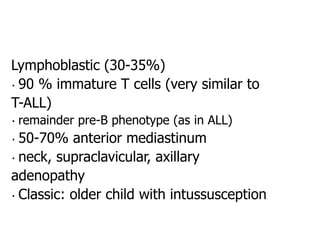
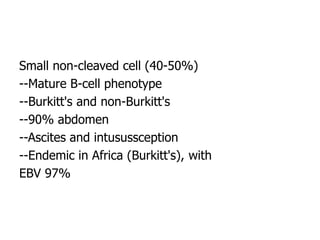
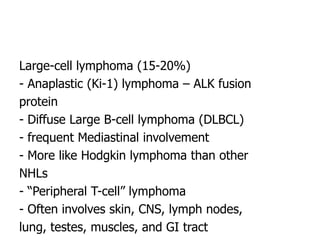
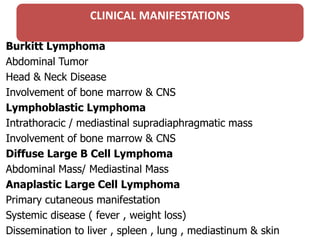
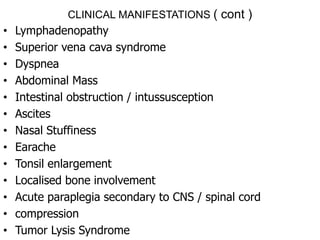
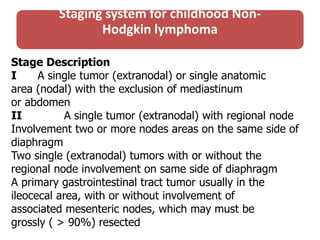
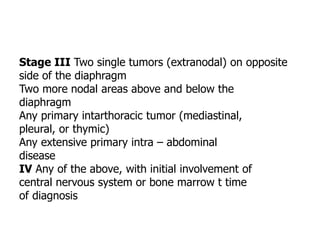
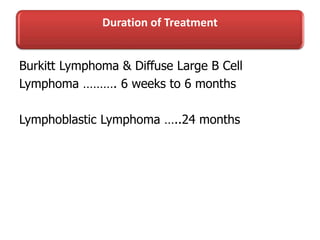
3. Non-Hodgkin's lymphoma in children includes subtypes like Burkitt's lymphoma, lymphoblastic lymphoma, diffuse large B-cell lymphoma, and anaplastic large cell lymphoma.