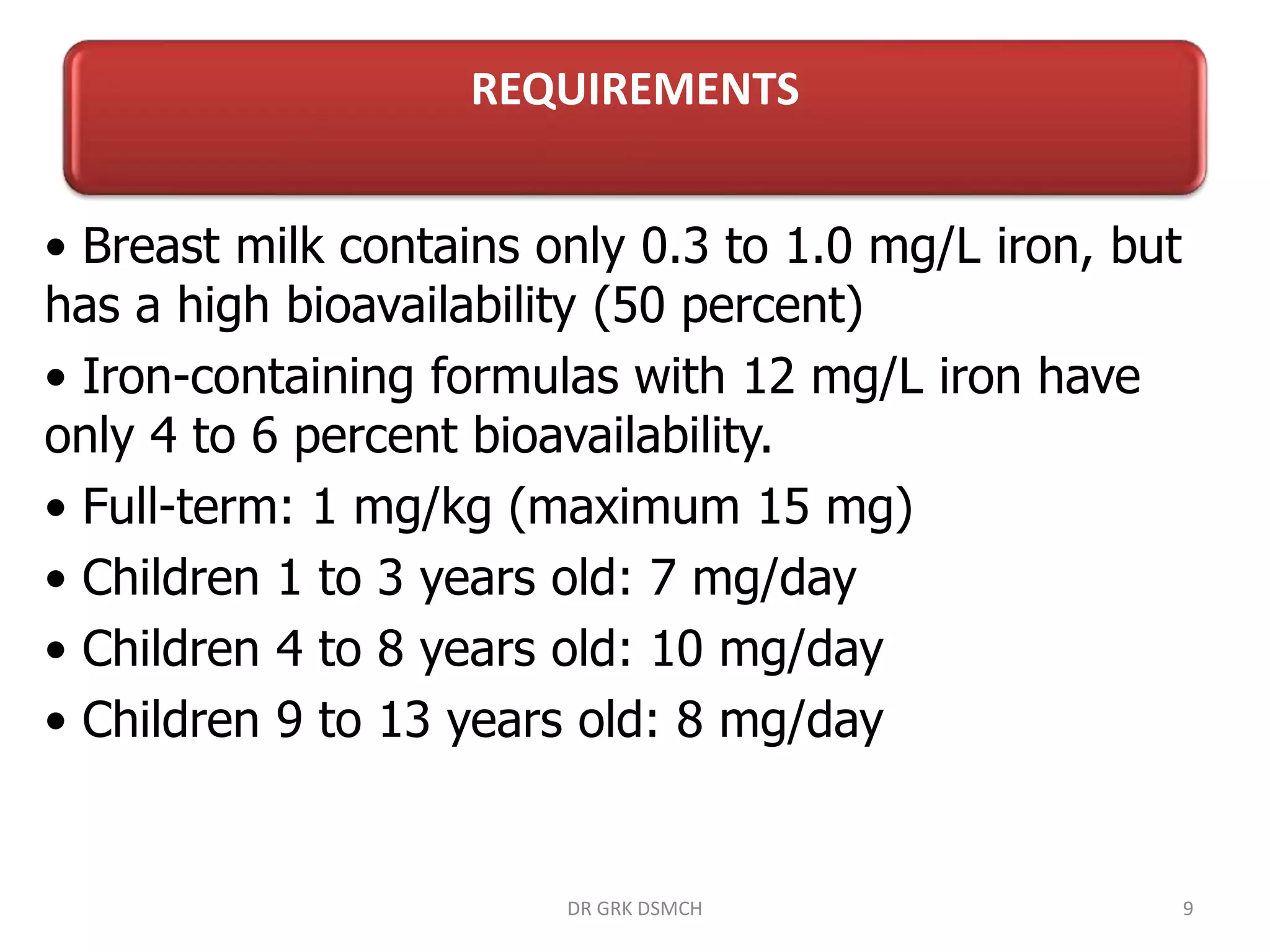
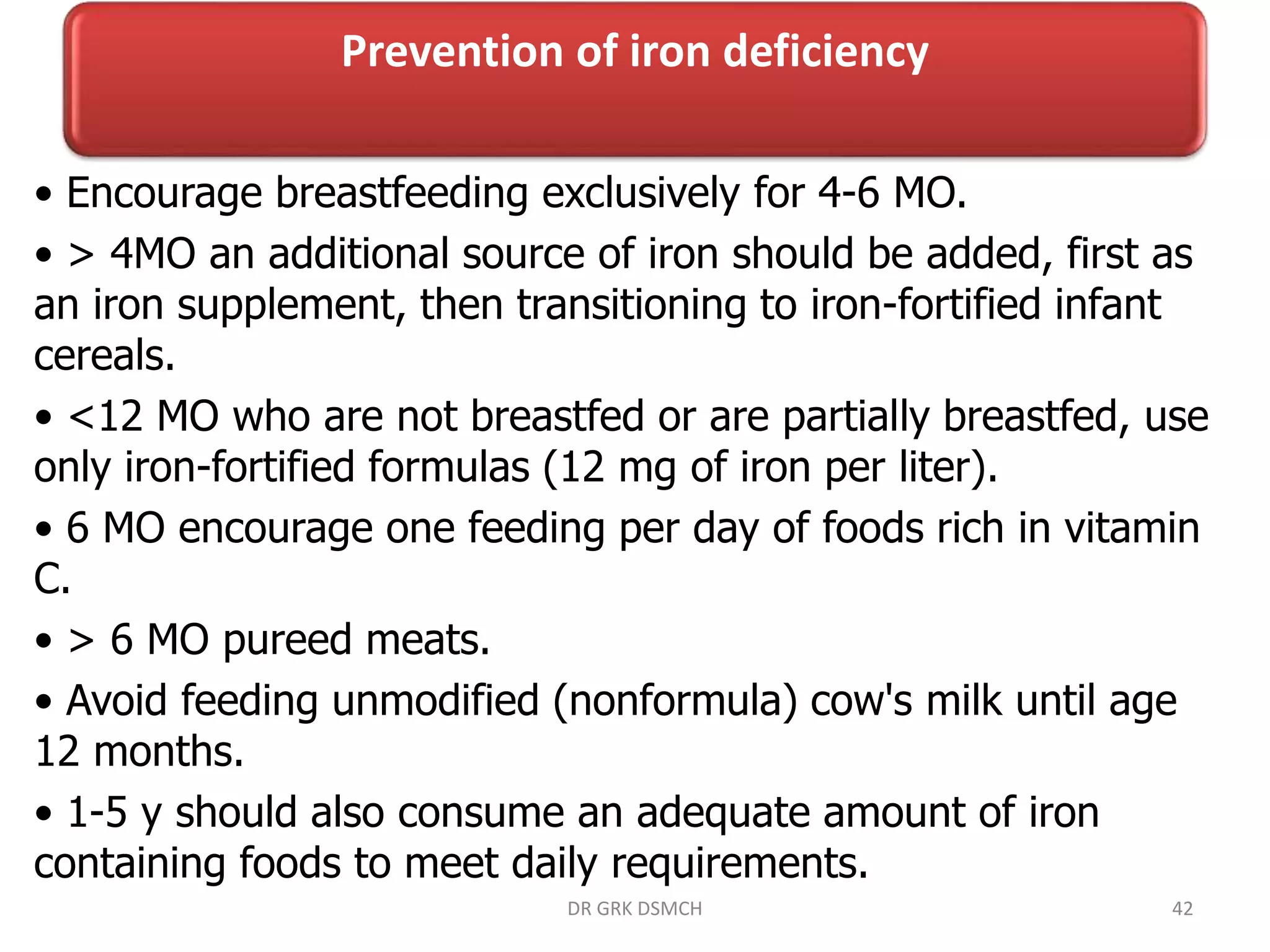
Dr. G.R. Rajkumar's document discusses iron deficiency and anemia in children. It begins with definitions, prevalence, functions of iron, and iron balance. It then discusses requirements, causes, clinical manifestations, diagnosis, treatment, and prevention of iron deficiency. The key points are:
- Iron deficiency is the most common nutritional deficiency in children.
- It can cause decreased attention, alertness, and learning abilities in children.
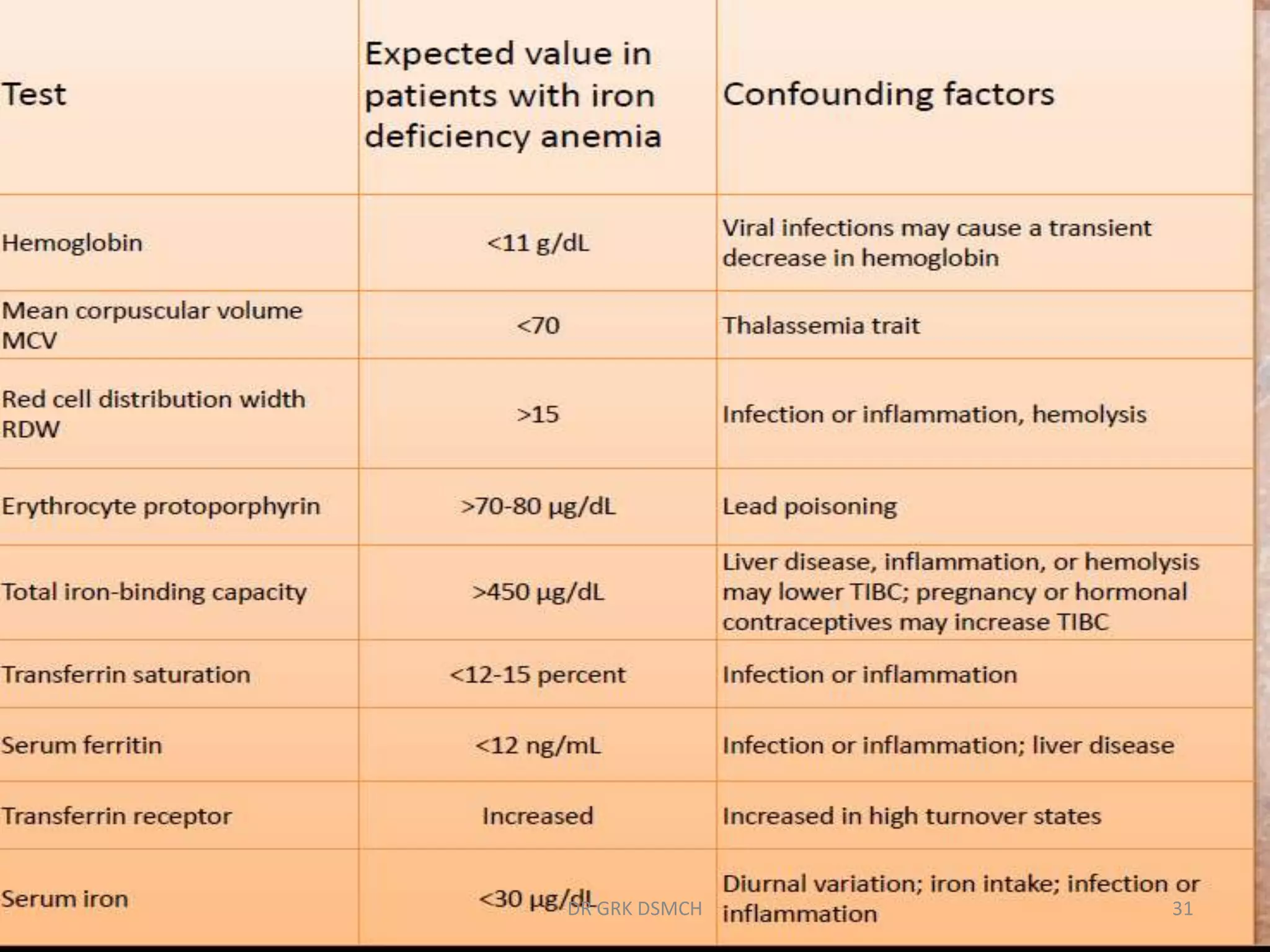
- Diagnosis involves laboratory tests like serum ferritin, transferrin saturation, and free erythrocyte protoporphyrin levels.
- Treatment is oral iron supplementation for 4-6 months to replenish iron stores after correcting anemia