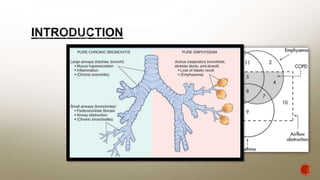
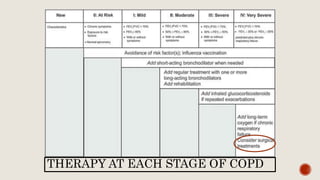
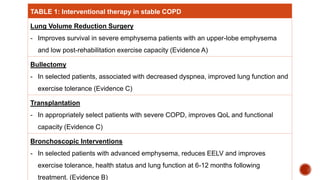
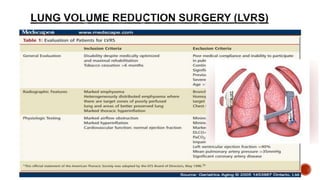
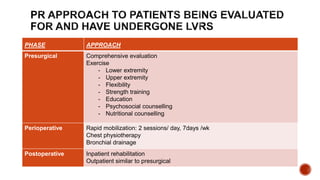
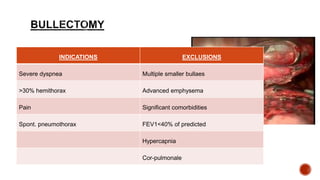
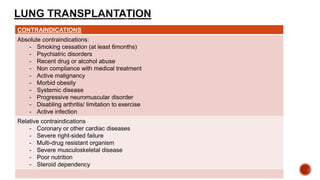
The document discusses various interventional therapies for managing chronic obstructive pulmonary disease (COPD), including lung volume reduction surgery and transplantation, emphasizing their benefits and criteria for selection based on patient's condition. It outlines preoperative and postoperative rehabilitation strategies, highlighting the importance of comprehensive evaluations and various contraindications for surgical options. Additionally, it addresses potential complications associated with lung transplantation and the necessity for immunosuppression post-surgery.