This document summarizes guidelines for radiotherapy planning for lung cancer. It discusses:
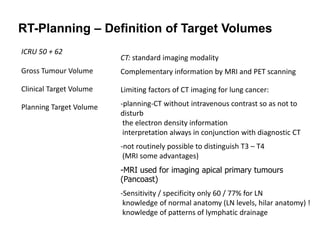
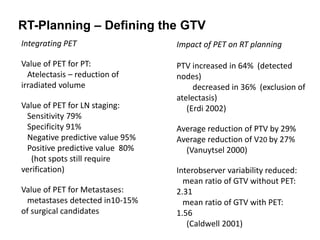
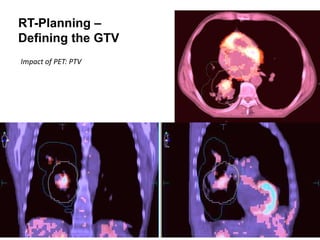
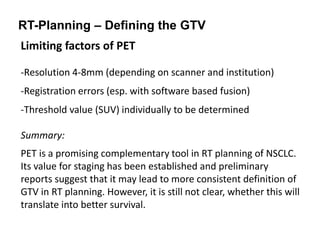
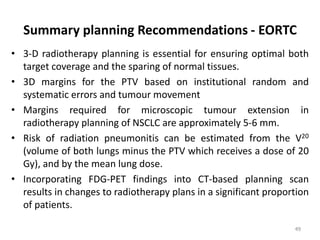
- Defining the gross tumor volume (GTV) based on imaging like PET which can help reduce margins.
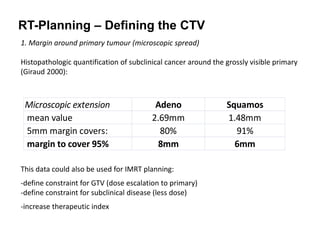
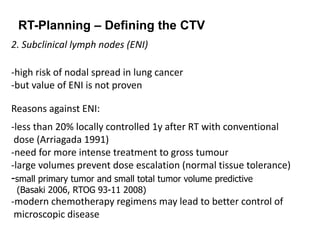
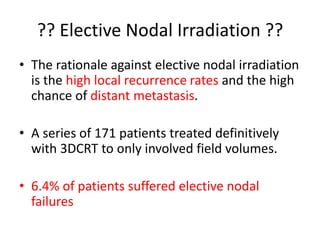
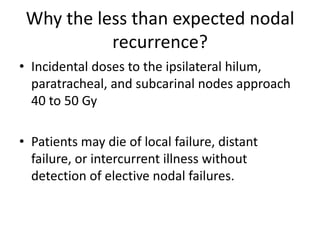
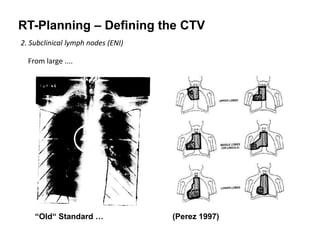
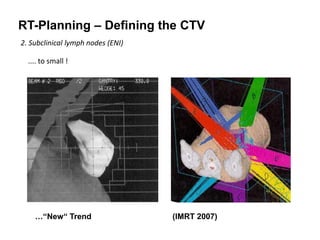
- Adding margins to the GTV to create the clinical target volume (CTV) accounting for microscopic spread. There is debate around elective nodal irradiation.
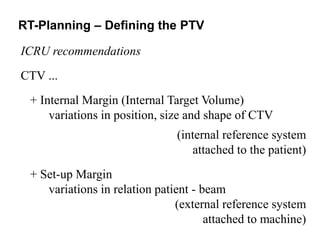
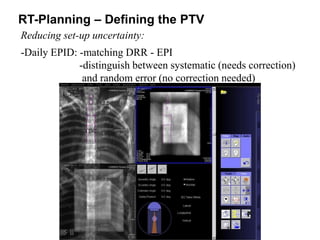
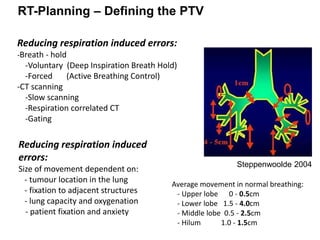
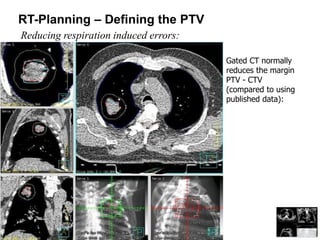
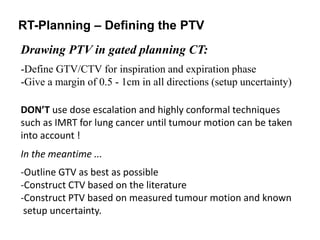
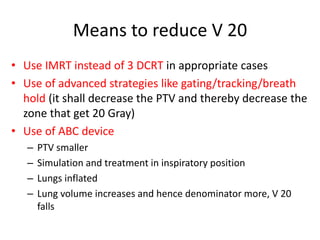
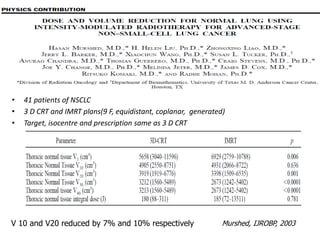
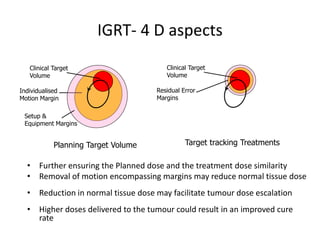
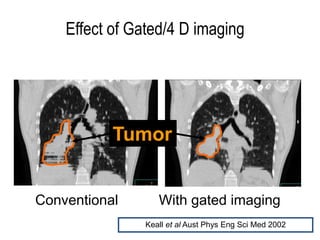
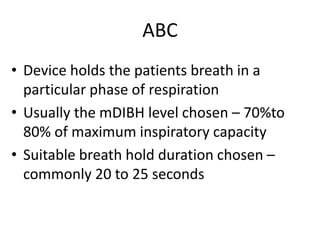
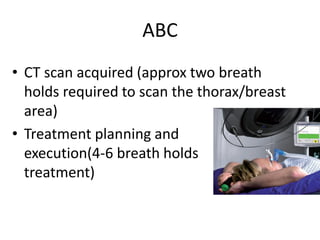
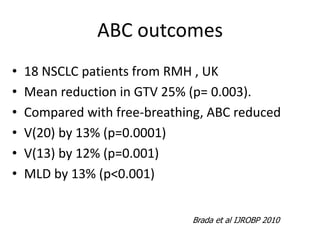
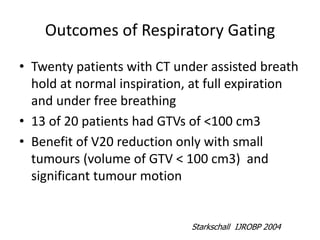
- Further expanding the CTV to create the planning target volume (PTV) accounting for set-up uncertainty and tumor motion. Techniques like gating can help reduce this.
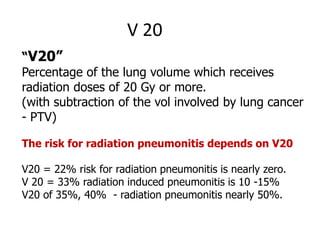
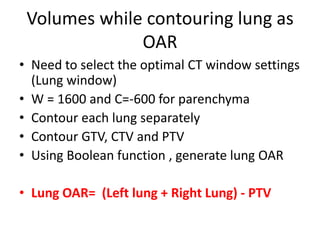
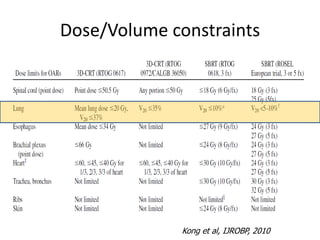
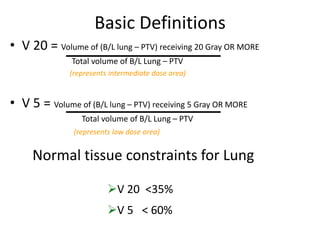
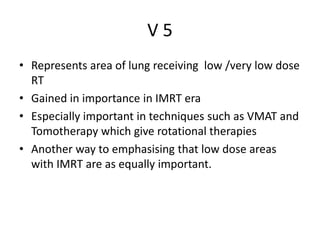
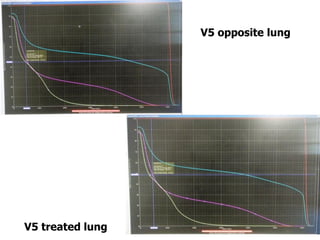
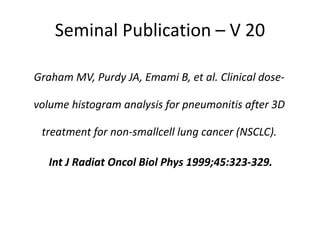
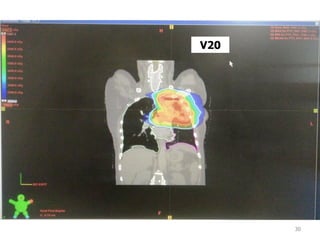
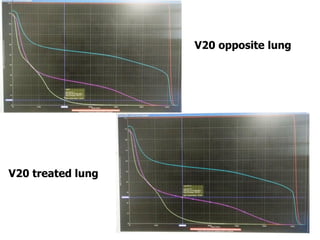
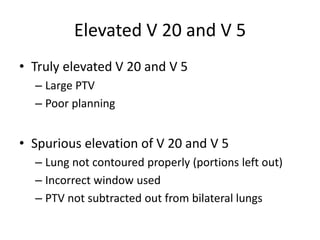
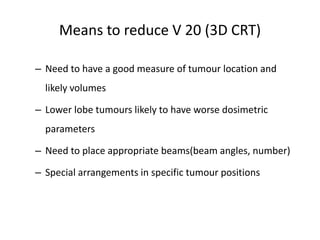
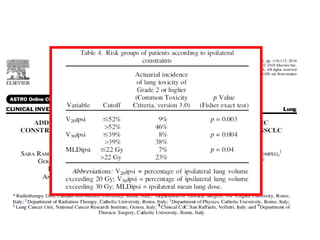
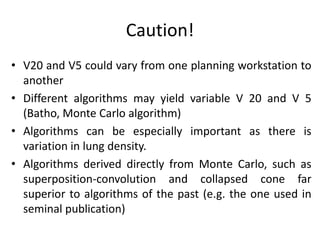
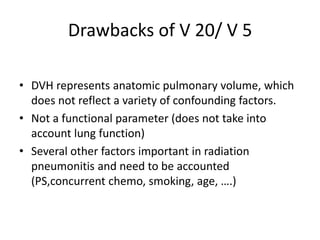
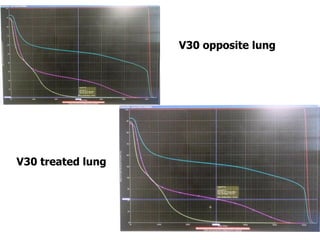
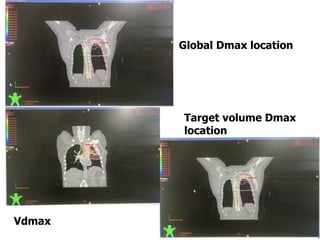
- Contouring the lungs as organs at risk and calculating dosimetric parameters like V20 and V5 to quantify lung dose and risk of toxicity. Dose needs to