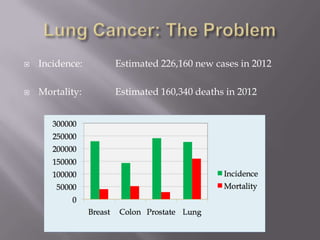
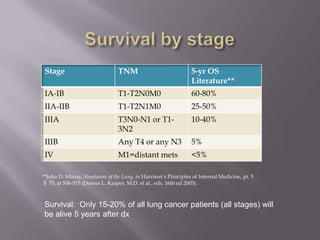
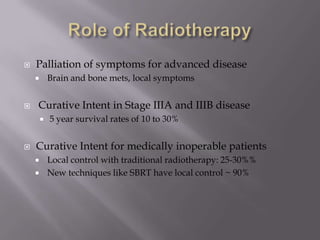
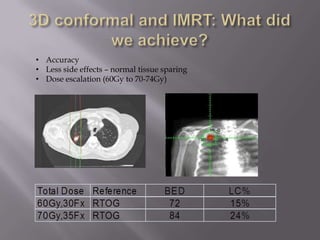
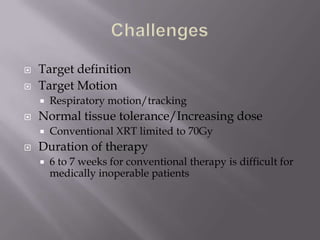
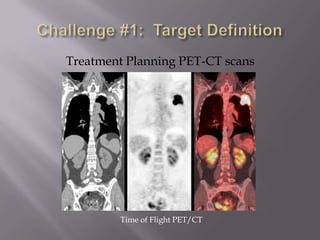
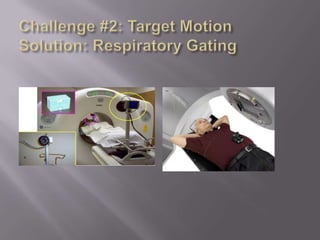
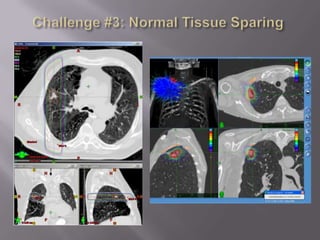
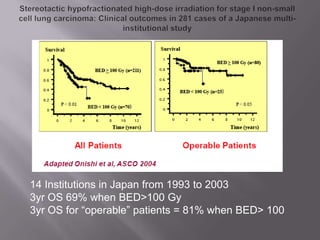
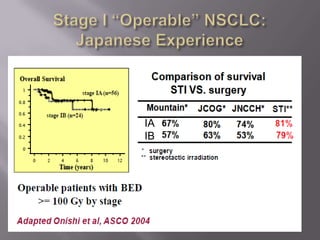
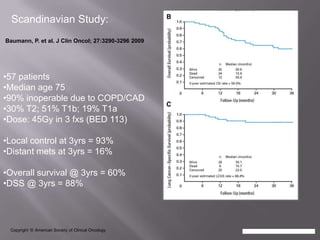
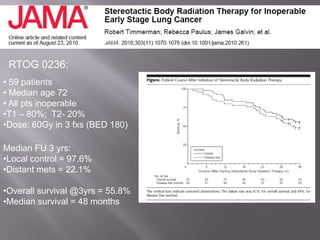
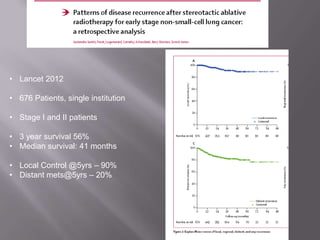
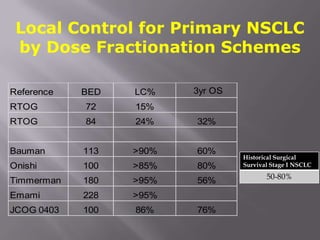
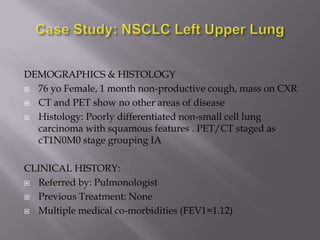
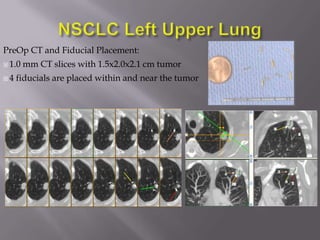
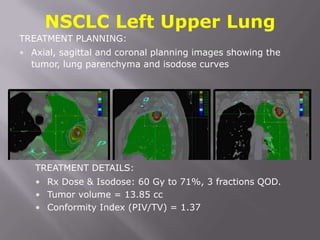
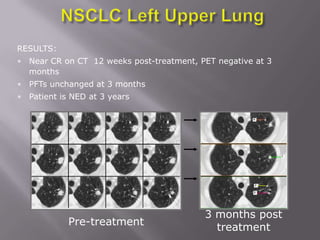
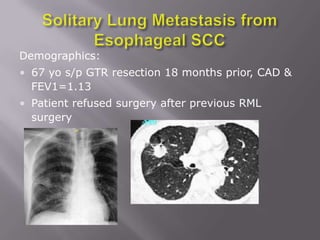
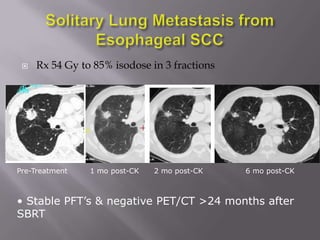
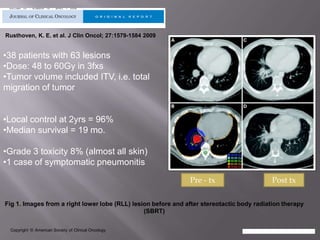
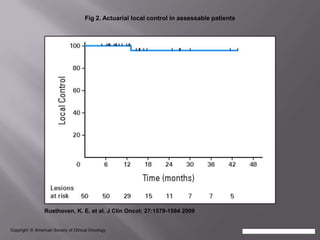
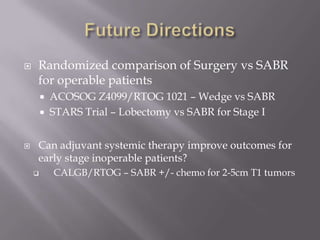
The document discusses the incidence, mortality, and survival rates of lung cancer, emphasizing the importance of advanced treatment modalities like stereotactic body radiation therapy (SBRT) for patients with early-stage non-small cell lung carcinoma (NSCLC). It highlights detailed findings from various studies on treatment effectiveness, local control rates, and patient demographics, suggesting SBRT as a minimally toxic yet potent therapy compared to traditional methods. The conclusion advocates for SBRT's emerging role in the standard care of medically inoperable patients and suggests future research directions comparing SBRT with surgery.