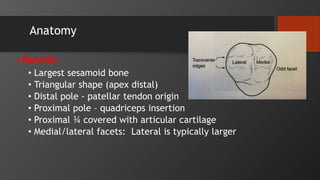
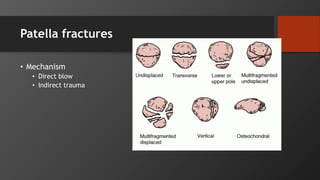
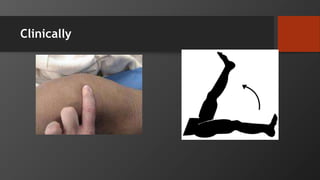
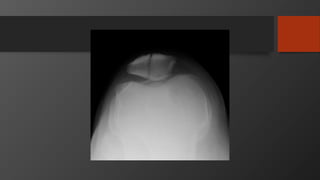
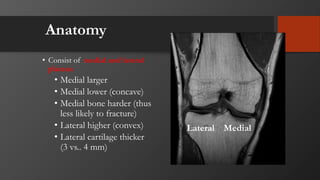
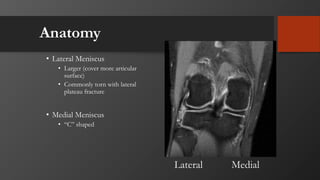
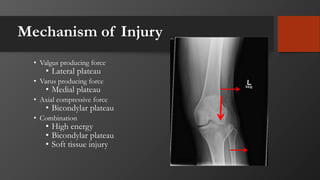
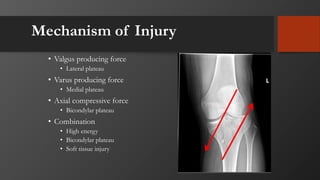
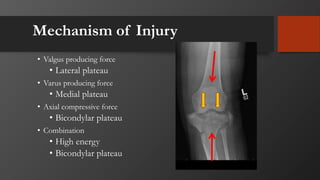
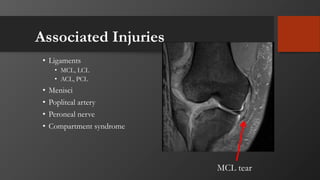
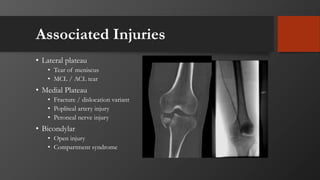
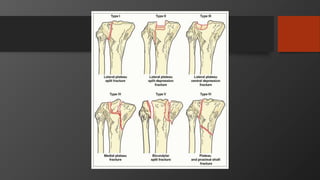
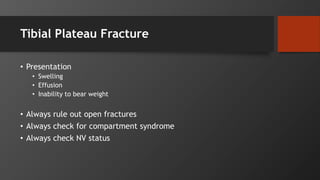
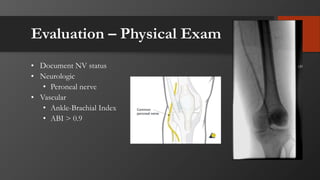
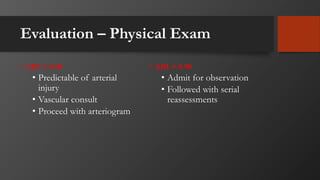
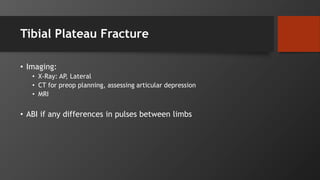
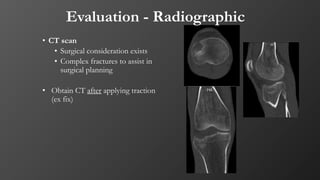
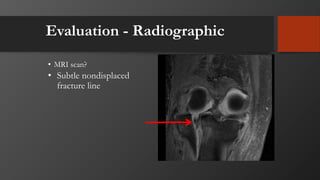
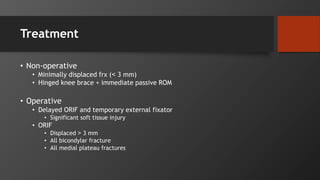
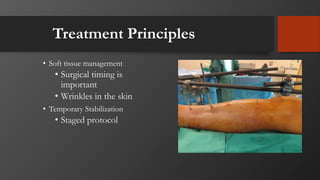
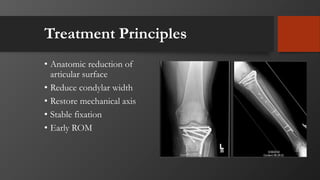
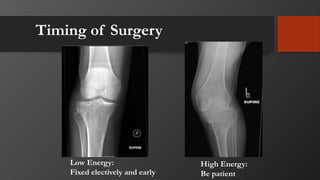
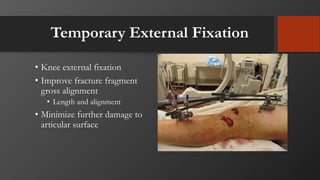
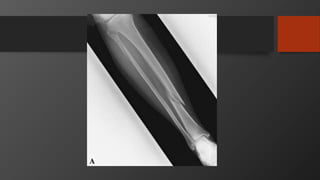
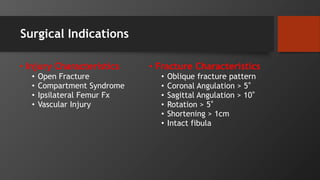
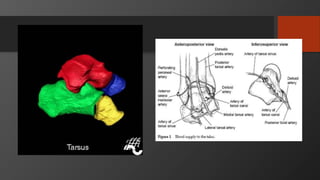
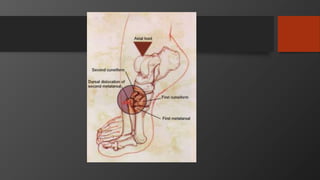
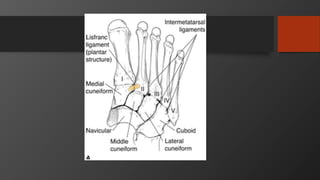
This document provides an overview of common orthopedic injuries of the lower extremity, including the patella, tibia, foot, and ankle. It describes the anatomy, mechanisms of injury, clinical presentation, imaging, and treatment options for fractures of the patella, tibial plateau, tibial shaft, talus, calcaneus, and fifth metatarsal. Treatment may involve non-operative management with casting or early range of motion, or surgical options like open reduction internal fixation or external fixation depending on the fracture pattern and stability. Complications of these injuries include nonunion, malunion, infection, arthritis, and impaired function.