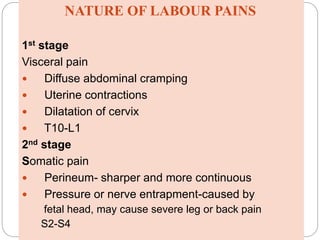
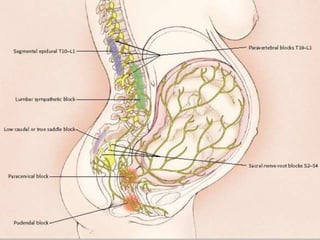
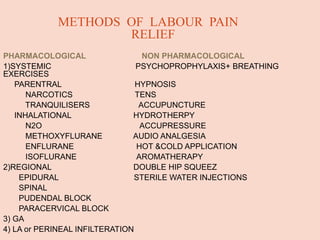
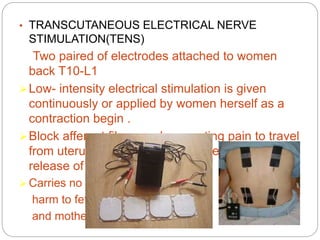
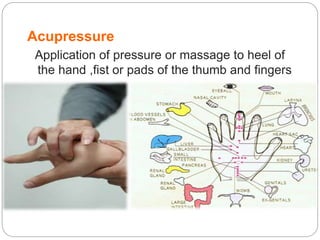
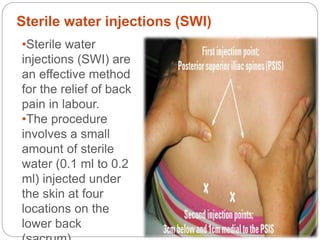
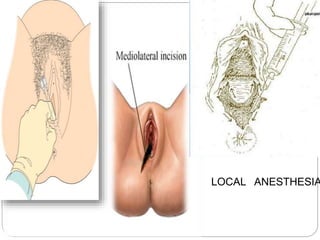
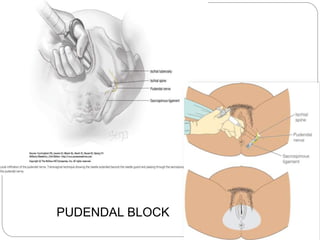
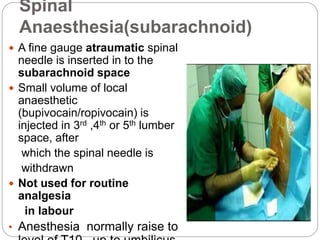
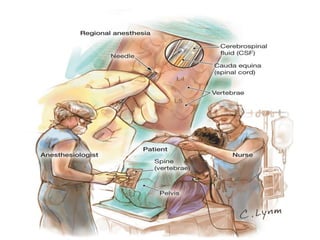
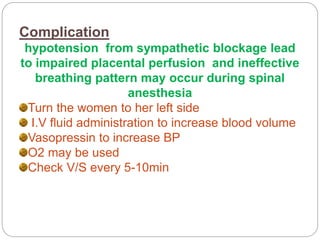
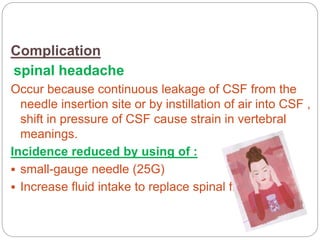
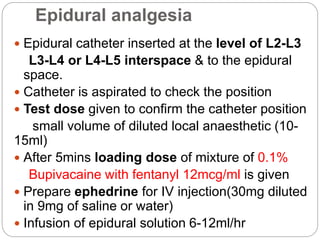
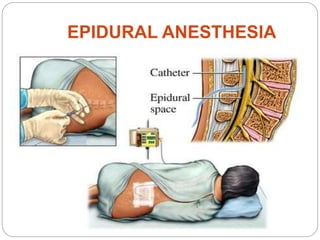
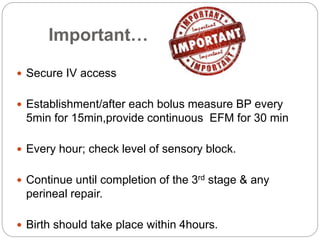
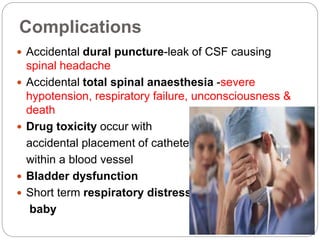
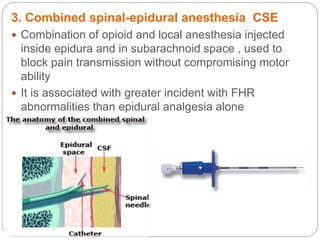
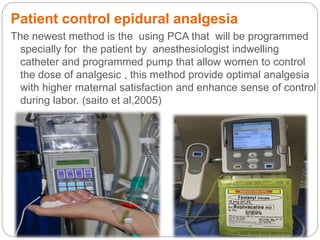
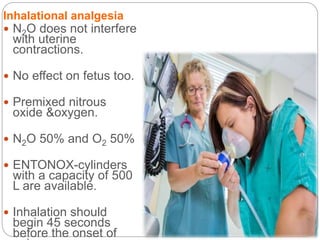
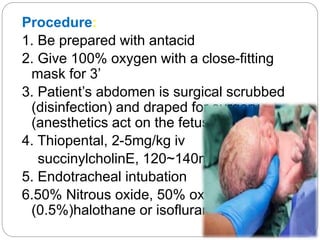
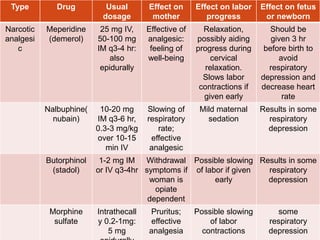
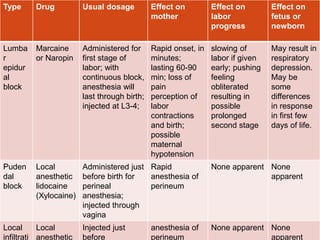
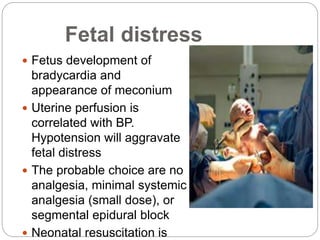
The document discusses pain management options during labor and delivery, including both pharmacological and non-pharmacological approaches. It defines labor pain, describes the nature and stages of labor pain, and discusses endorphins and their role in pain relief. Both non-pharmacological methods like hydrotherapy, TENS, acupuncture, and hypnosis as well as pharmacological options like narcotics, epidural analgesia, spinal analgesia, nitrous oxide, and general anesthesia are explained in terms of their use, effects, advantages, disadvantages, complications, and contraindications. Regional techniques like epidural analgesia are emphasized as the most common and effective method for relieving labor pain.