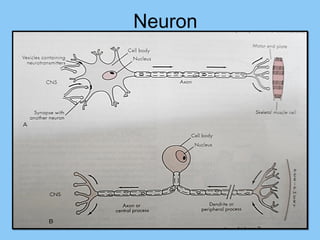
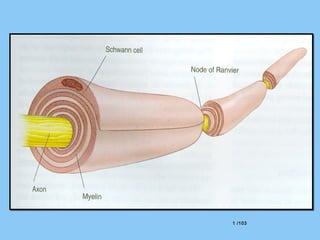
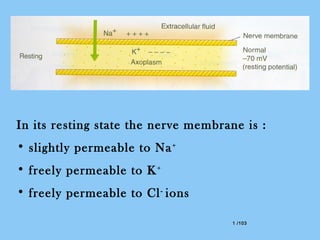
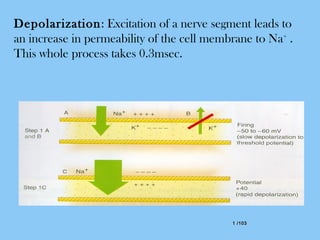
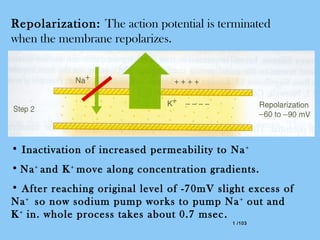
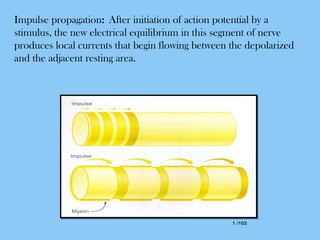
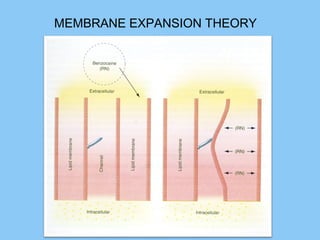
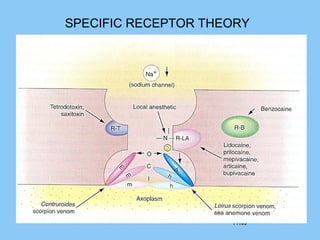
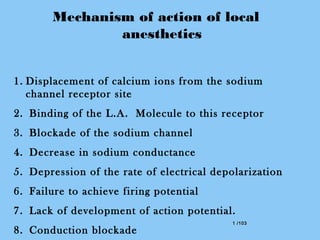
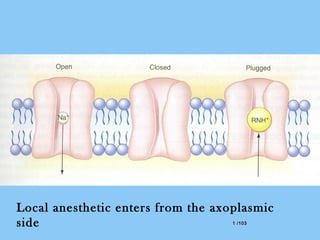
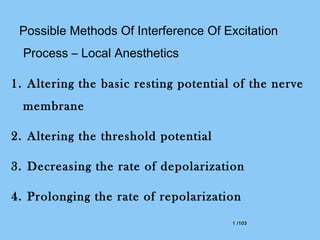
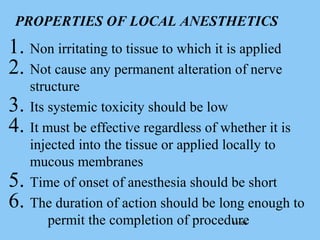
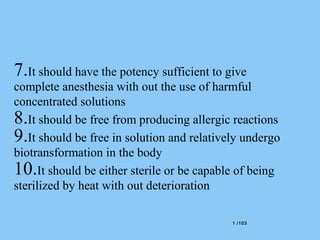
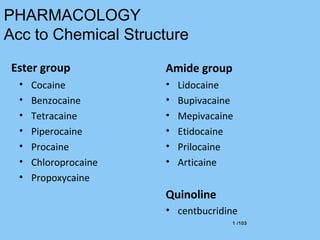
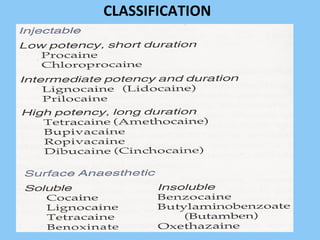
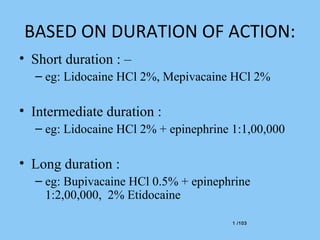
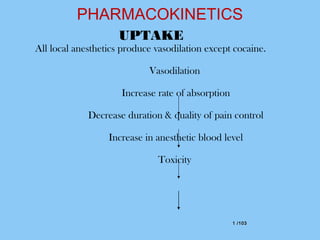
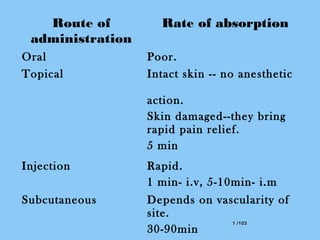
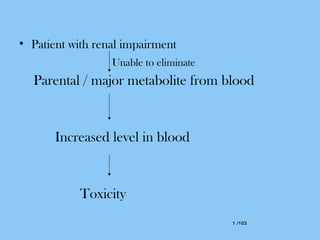
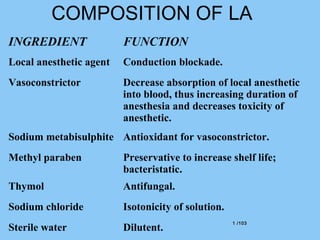
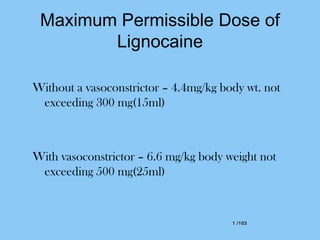
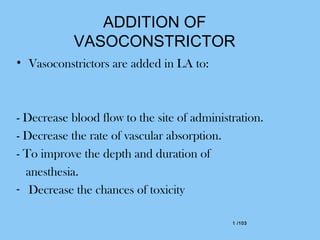
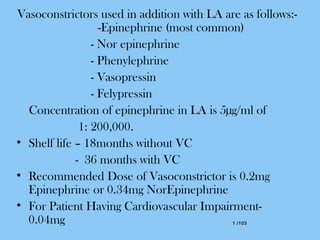
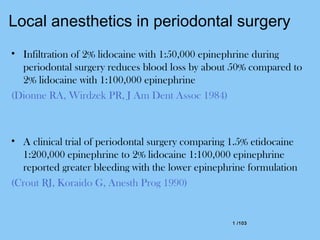
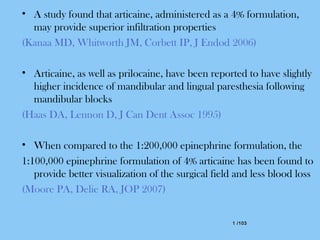
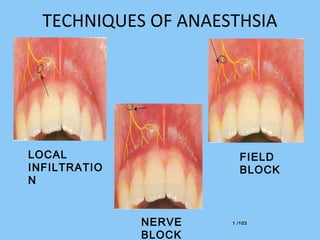
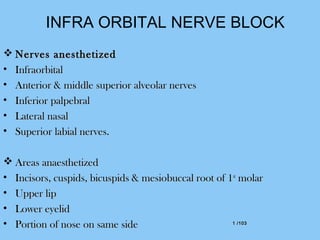
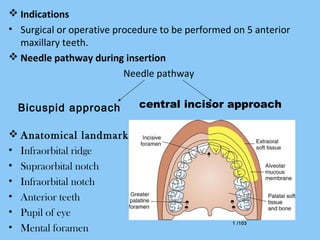
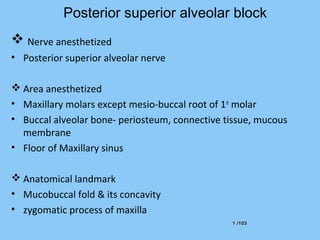
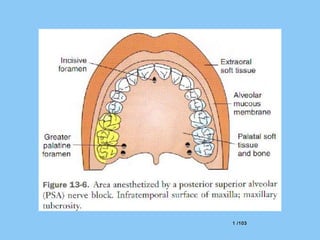
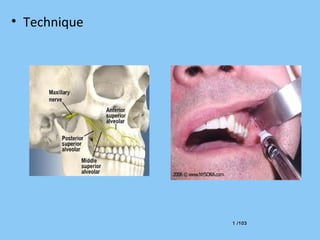
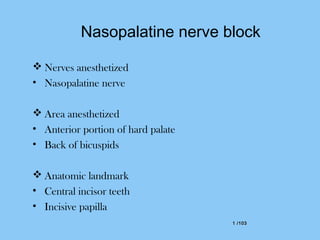
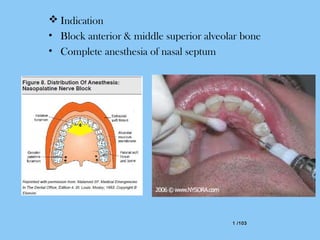
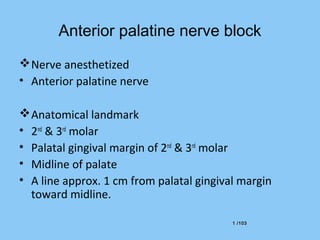
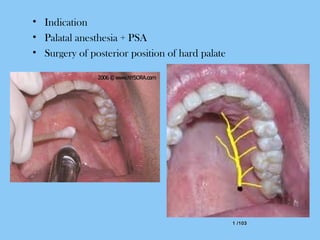
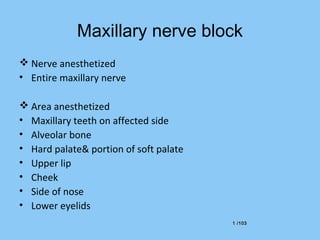
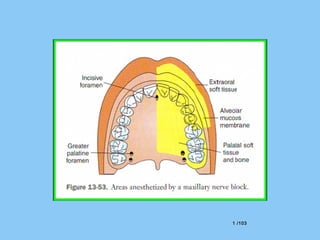
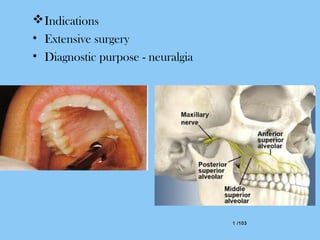
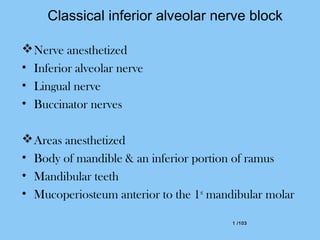
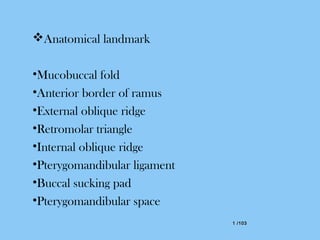
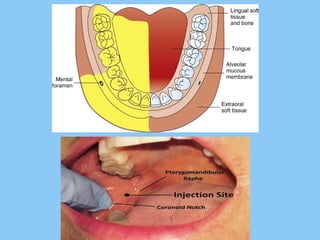
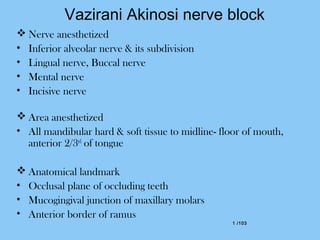
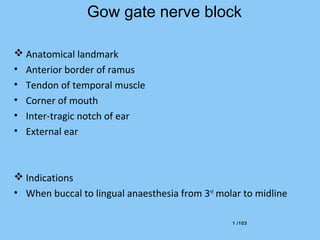
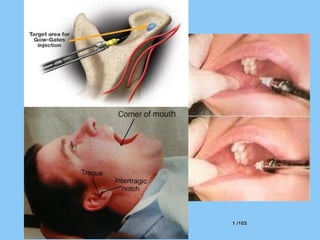
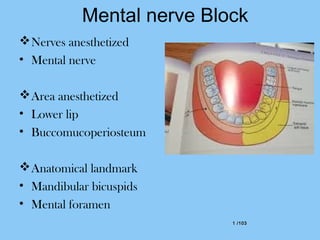
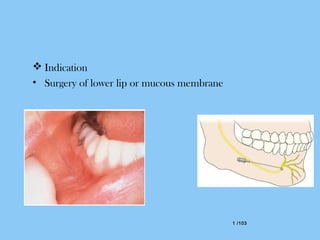
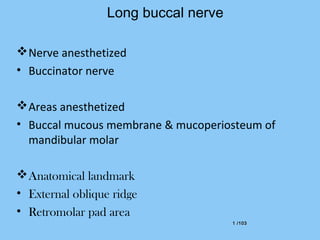
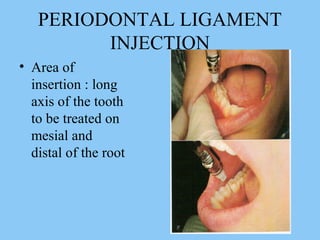
This document provides information on local anesthesia. It begins with definitions and history, describing how local anesthesia was developed by Koller in 1884 using procaine. It then discusses the various methods of inducing local anesthesia and the neuroanatomy and electrophysiology of nerve conduction. The remainder of the document focuses on the pharmacology of local anesthetics, including theories of action, properties, classification, pharmacokinetics, composition, and maximum permissible doses. Specific local anesthetic techniques for the maxilla and mandible are also outlined.