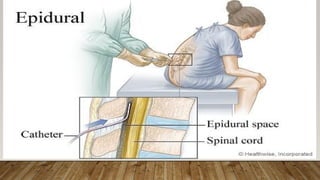
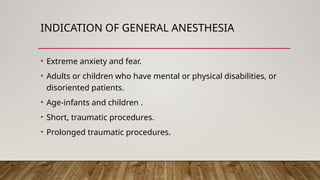
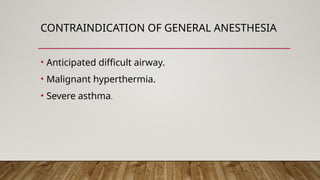
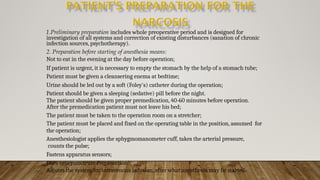
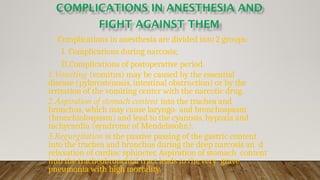
Anesthesia is a medical method used to control pain during surgery through various types of anesthetics that can induce local, regional, or general effects. Local anesthesia targets specific areas with agents blocking nerve conduction, regional anesthesia numbs broader areas, and general anesthesia induces a controlled state of unconsciousness. Each type has distinct indications, contraindications, mechanisms of action, and potential side effects, which are critical for safe and effective surgical procedures.