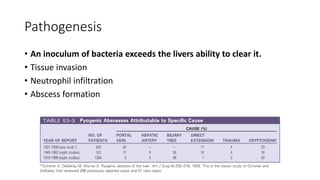
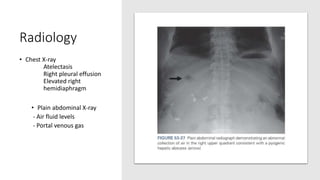
- Liver abscesses are typically caused by bacterial infections spreading from other sites like the biliary tract or portal vein. Common bacteria include E. coli and K. pneumoniae. Abscesses are usually diagnosed using imaging like ultrasound or CT scan and treated with antibiotics and drainage if large.
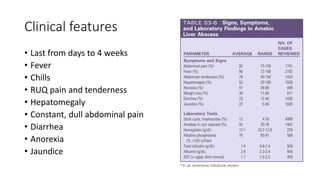
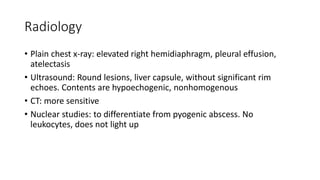
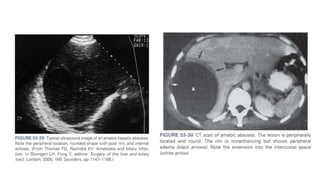
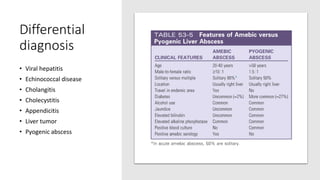
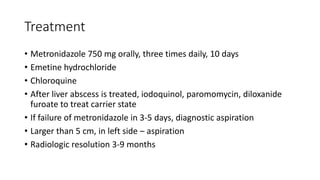
- Amebic abscesses are caused by Entamoeba histolytica infection spreading from the colon. They present similarly to pyogenic abscesses but are diagnosed serologically or with immunoassays. Metronidazole is the treatment.
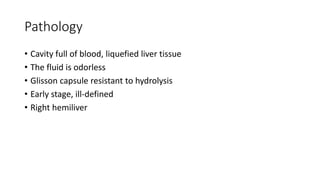
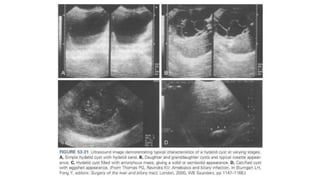
- Hydatid cysts are caused by the parasite Echinococcus granulosus. Humans are an accidental intermediate host. Cysts usually form in the liver and