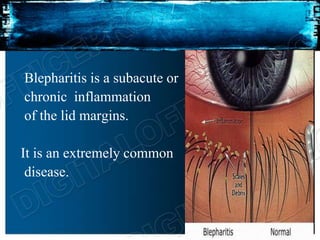
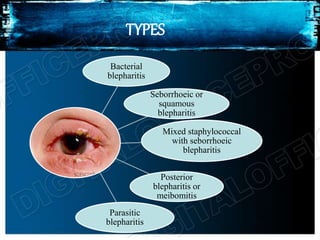
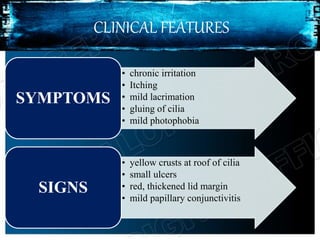
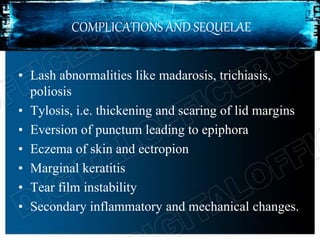
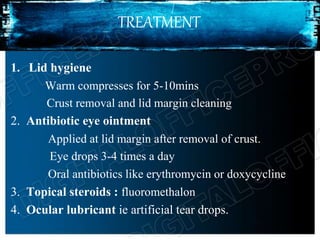
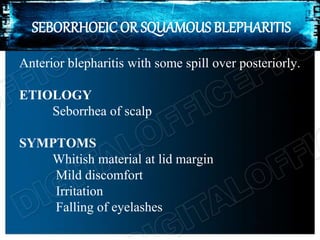
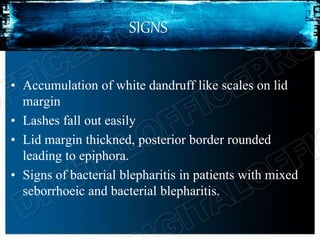
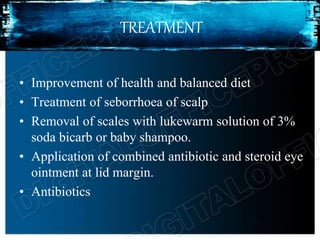
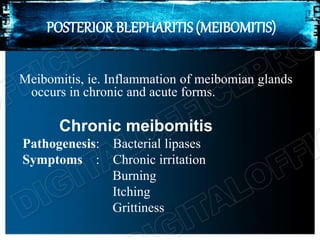
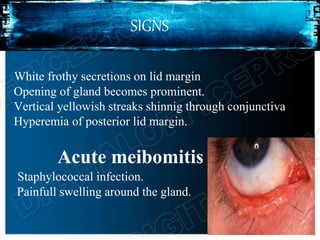
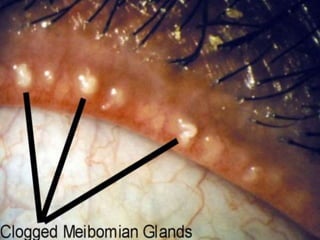
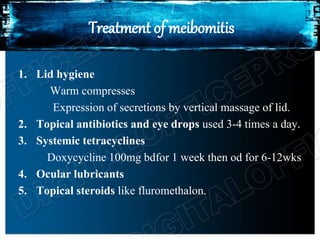
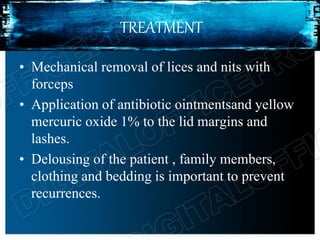
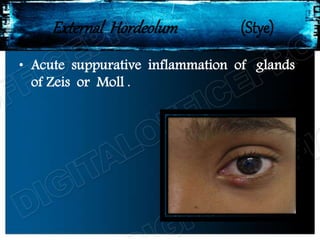
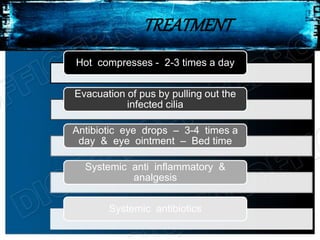
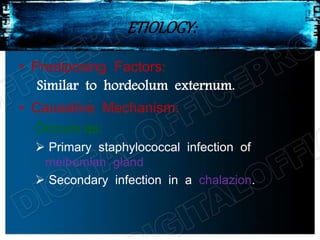
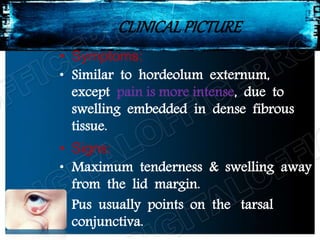
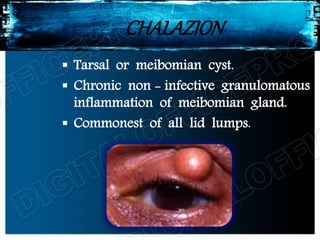
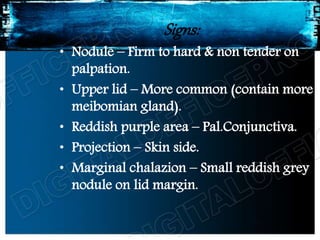
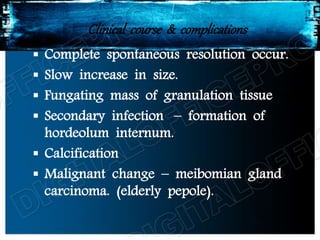
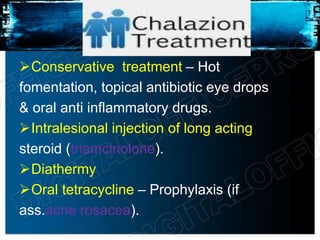
Blepharitis is an inflammation of the eyelid margins that can be caused by bacteria, seborrhea, or meibomian gland dysfunction. It commonly presents with irritation, itching, crusting or scaling of the eyelids. Treatment involves warm compresses, lid scrubs, antibiotic ointments or drops, and oral antibiotics if needed. More severe forms include hordeolum (styes) which are infections of the eyelid glands, and chalazion which are non-infected cysts of the meibomian glands that may require incision and drainage. Regular lid hygiene is important to prevent complications and recurrence.