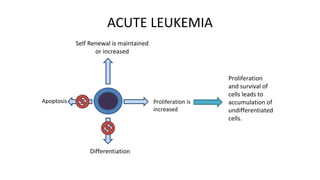
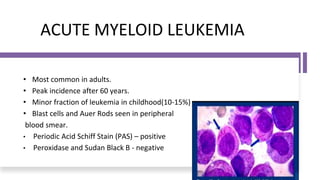
Leukemia is a type of blood cancer that begins in the bone marrow and is characterized by an abnormal increase in white blood cells. The exact cause is unknown but genetic factors, infections, and environmental exposures are associated with increased risk. Leukemia is classified as either acute or chronic and as affecting myeloid or lymphoid cells. Common symptoms include fatigue, fever, easy bruising and bleeding. Treatment involves chemotherapy, radiation therapy, stem cell transplants or splenectomy depending on the classification and severity.