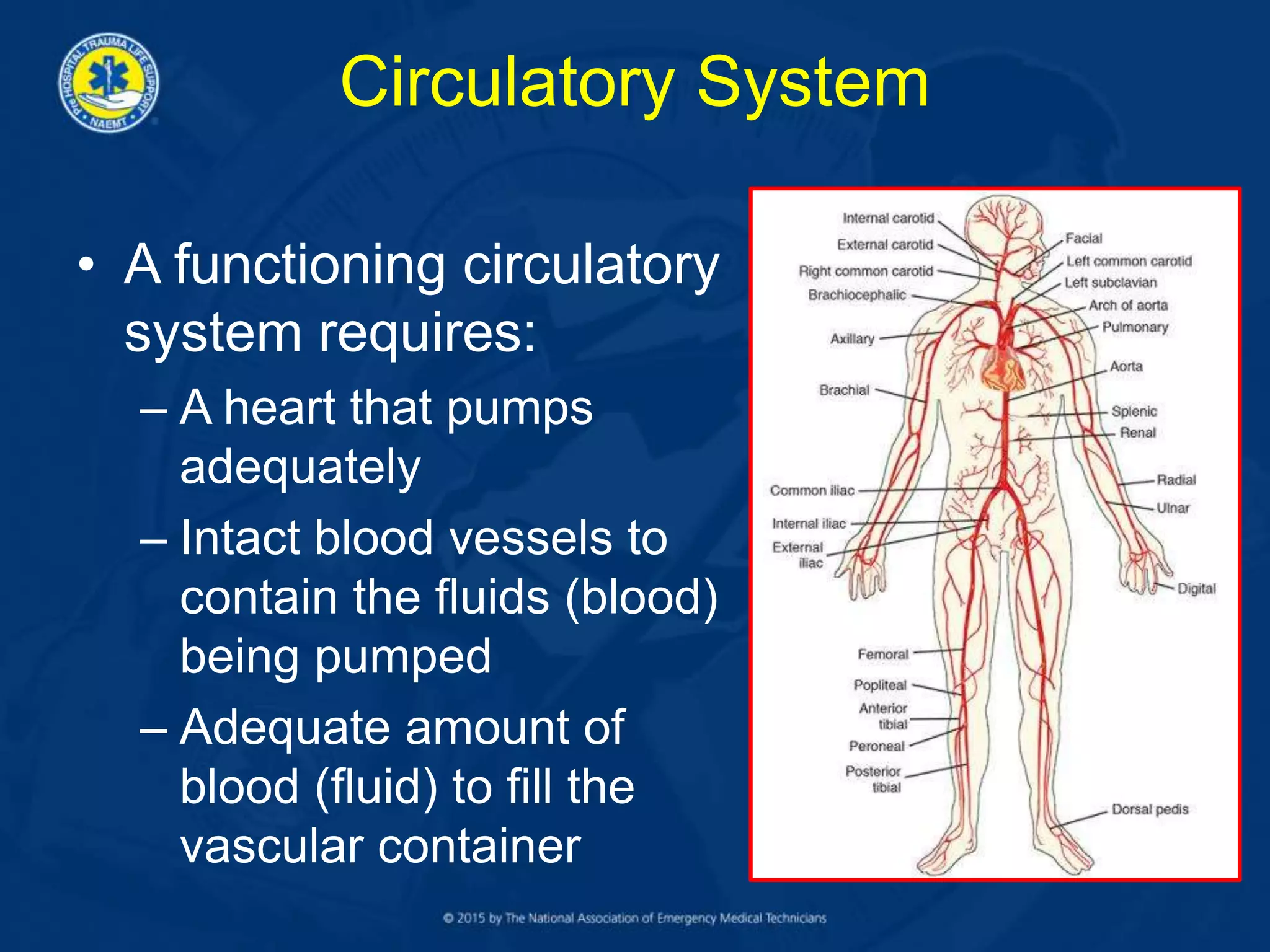
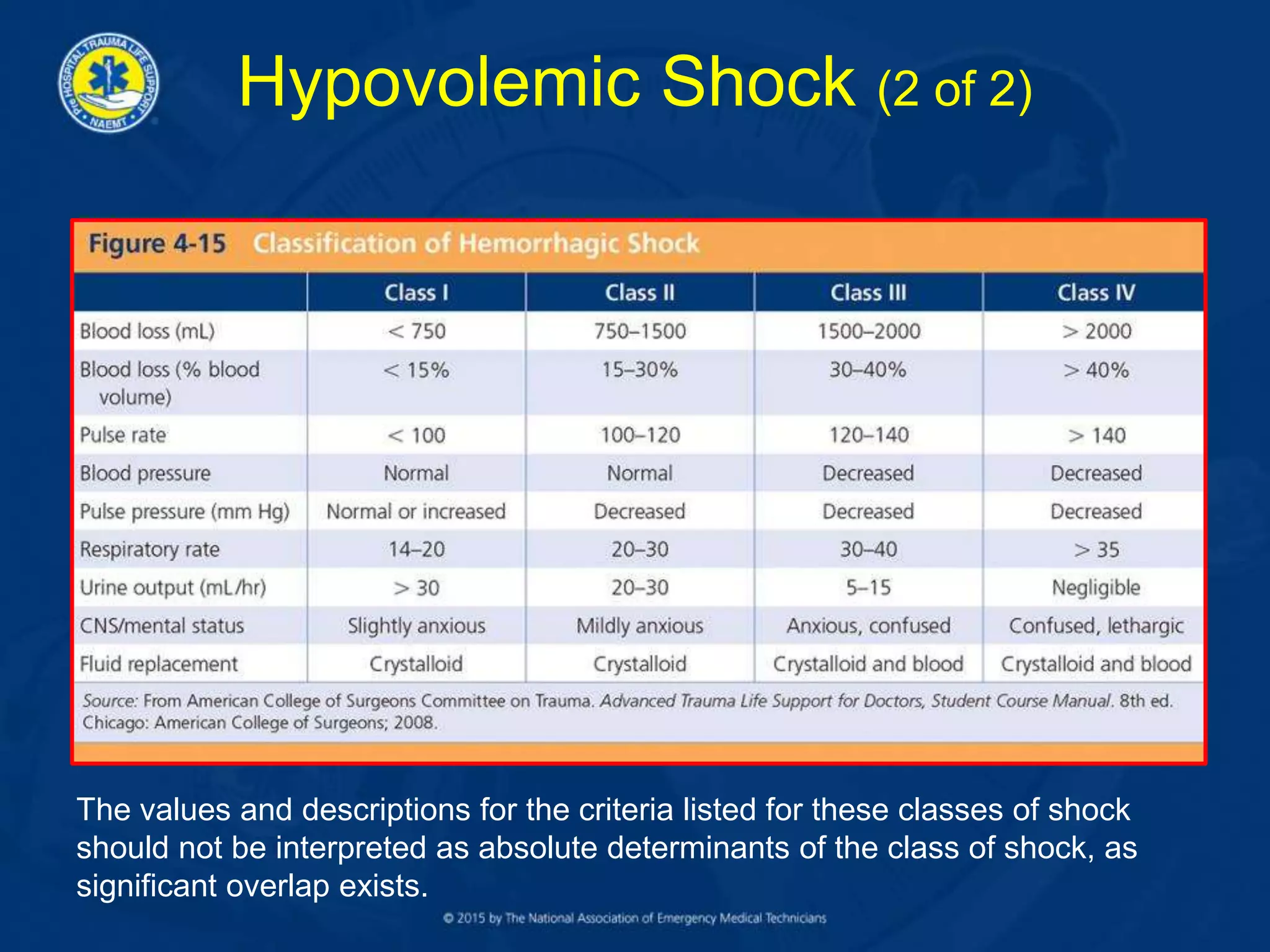
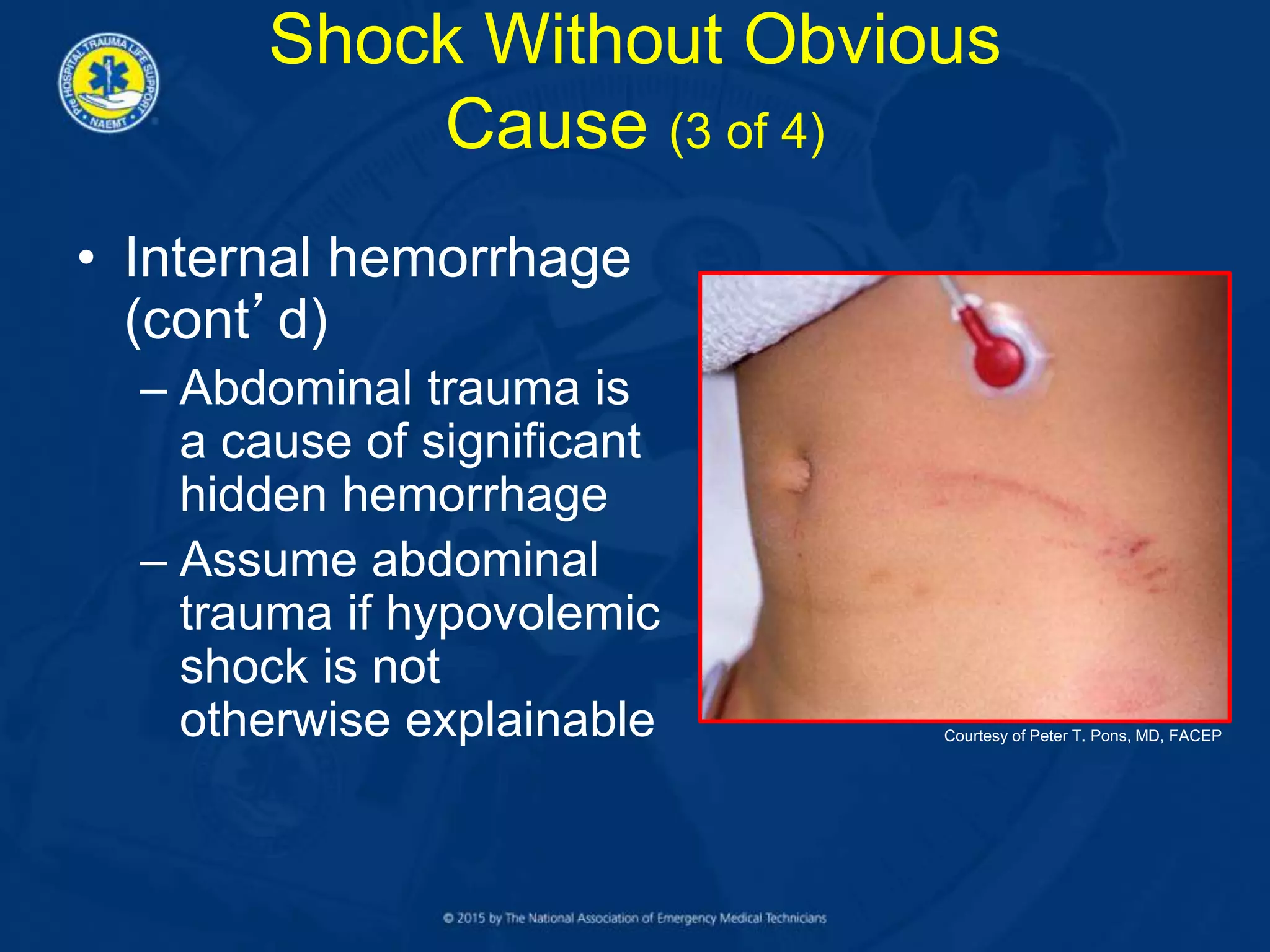
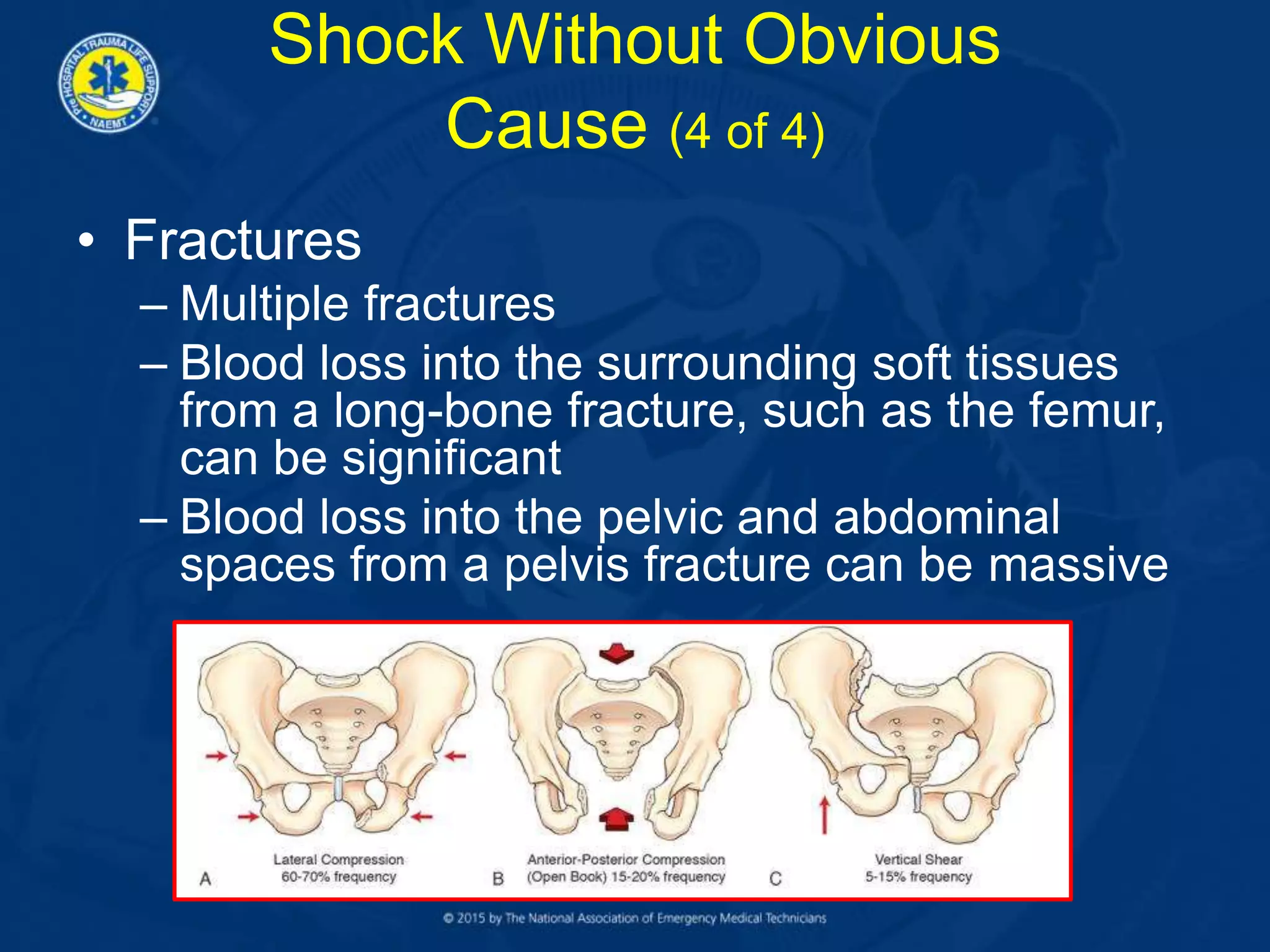
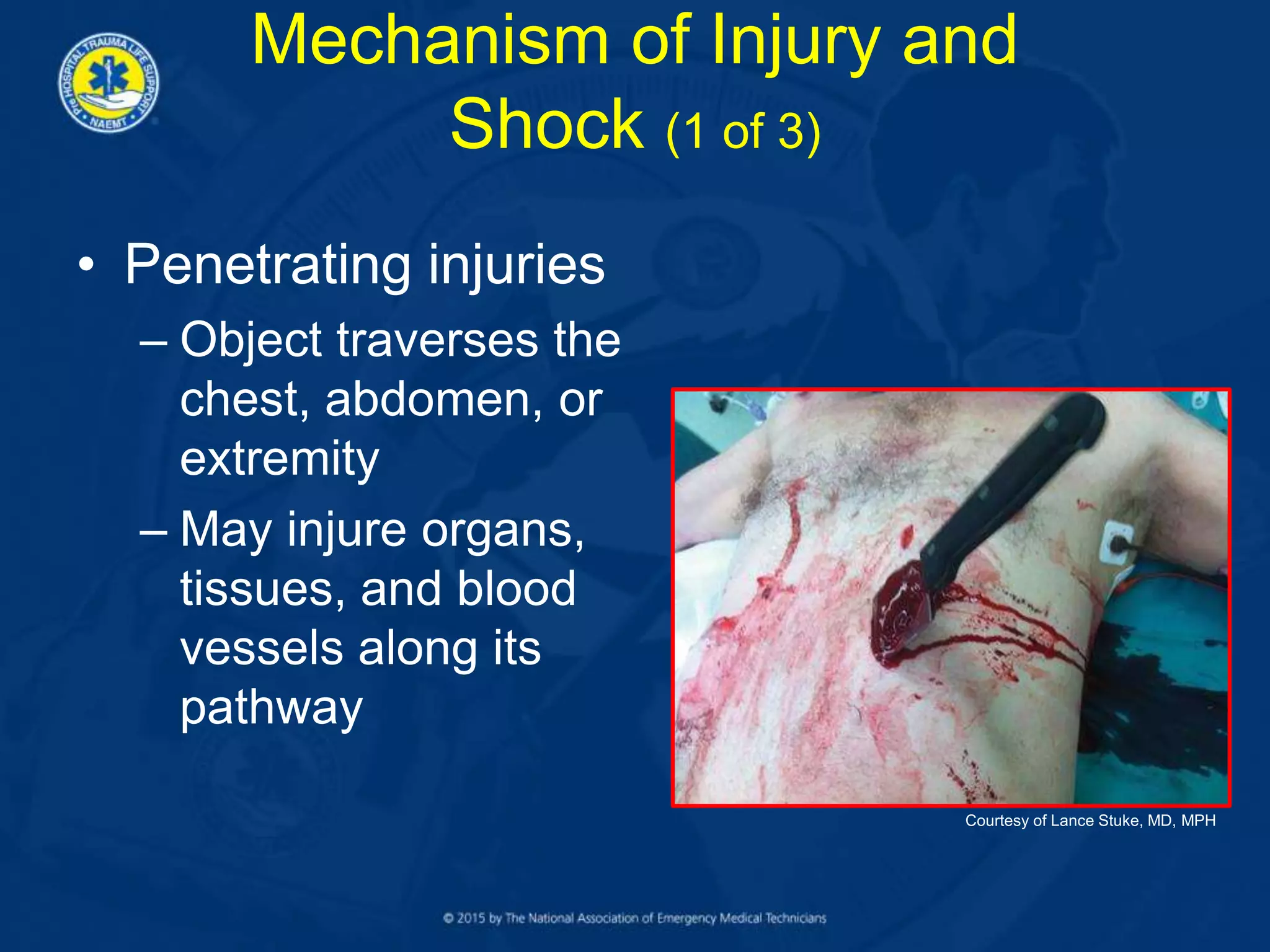
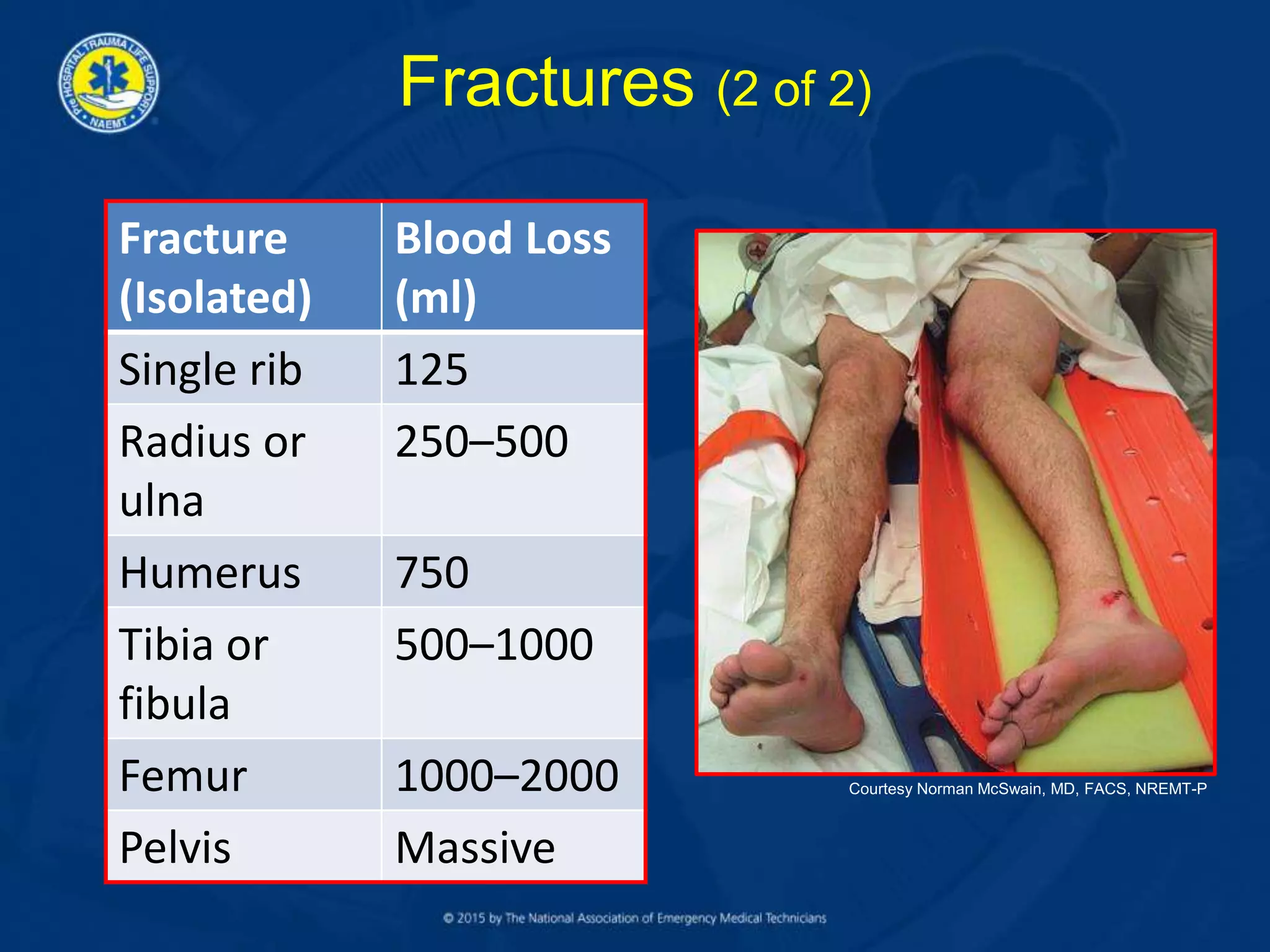
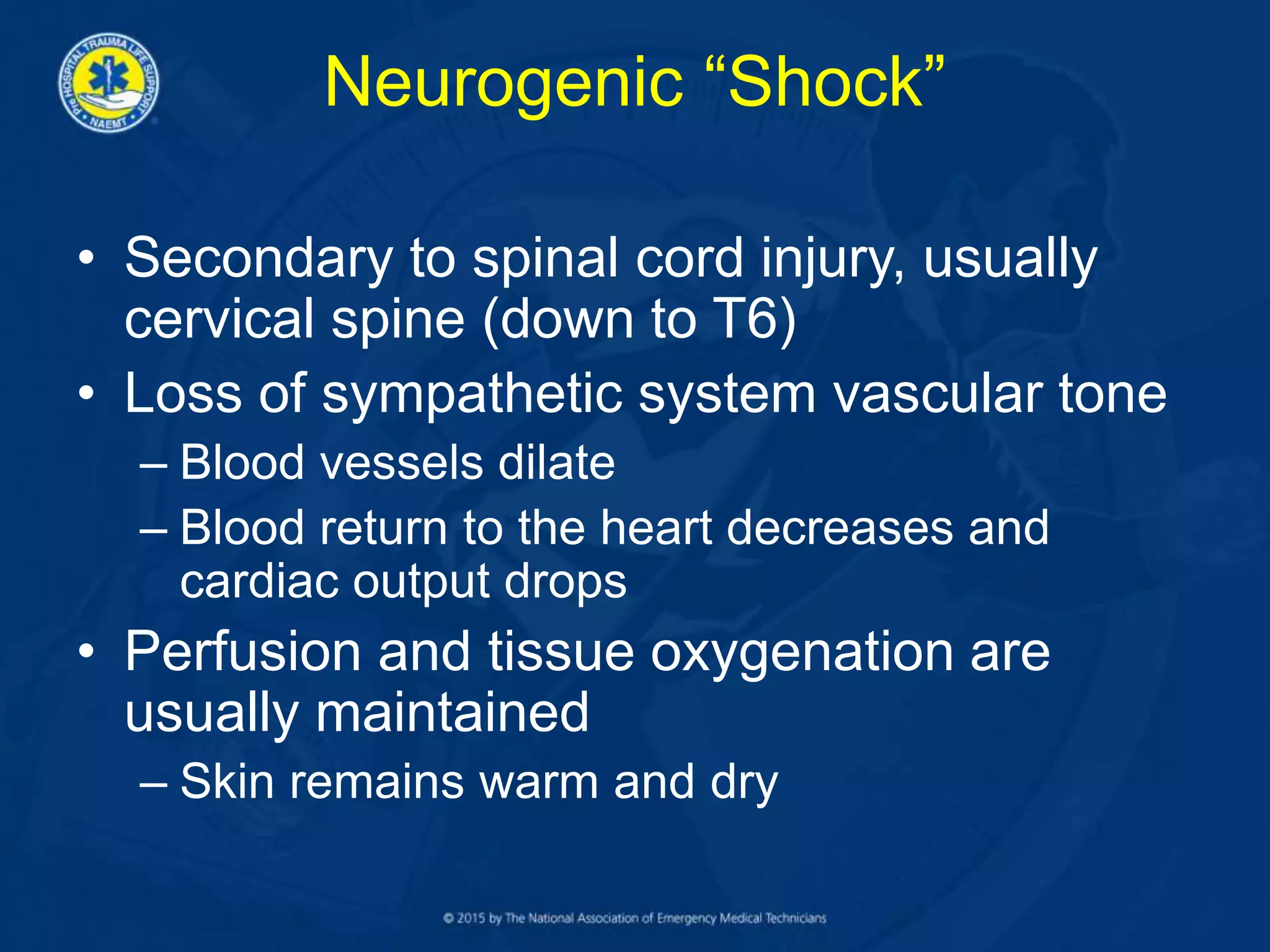
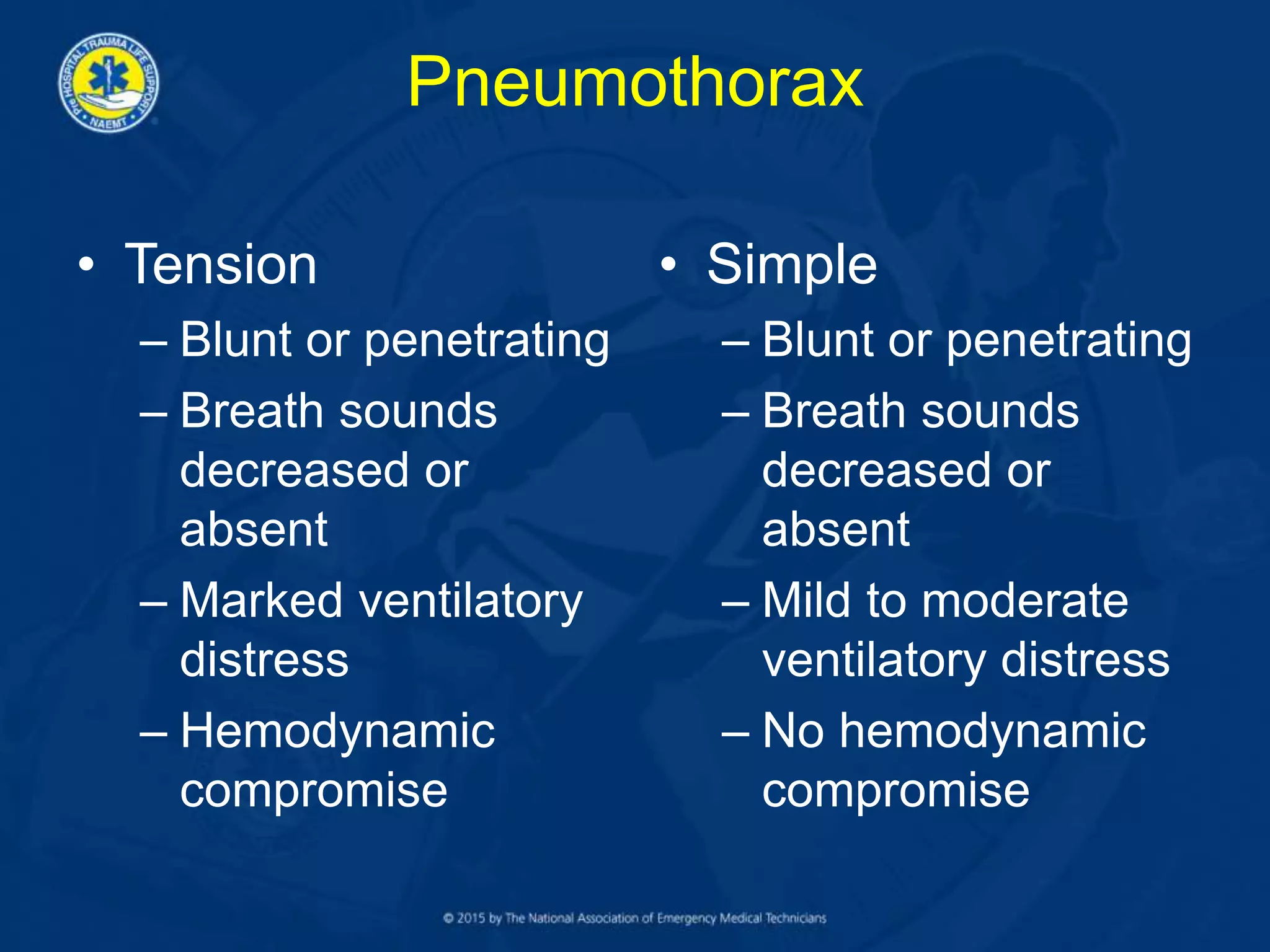
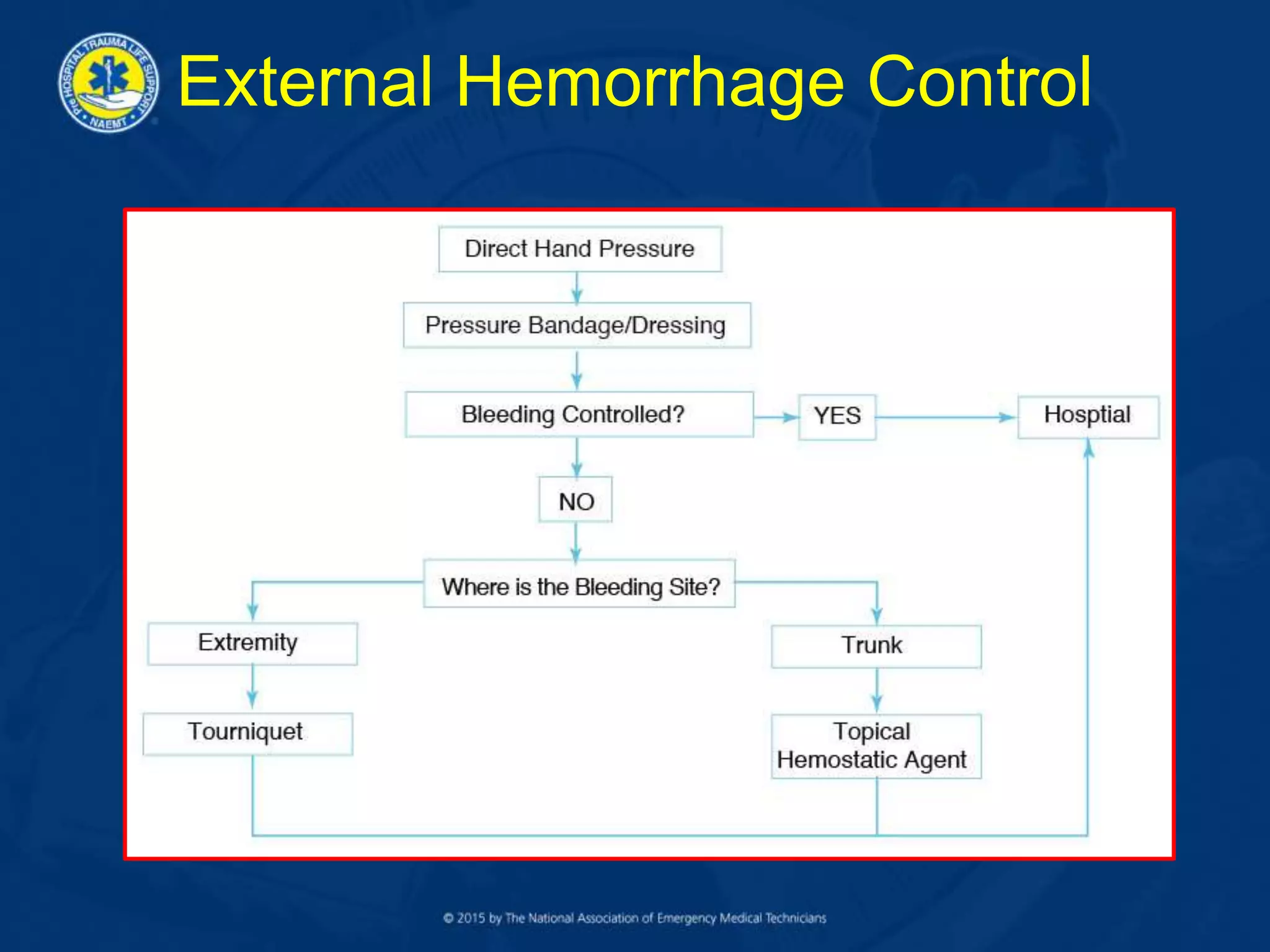
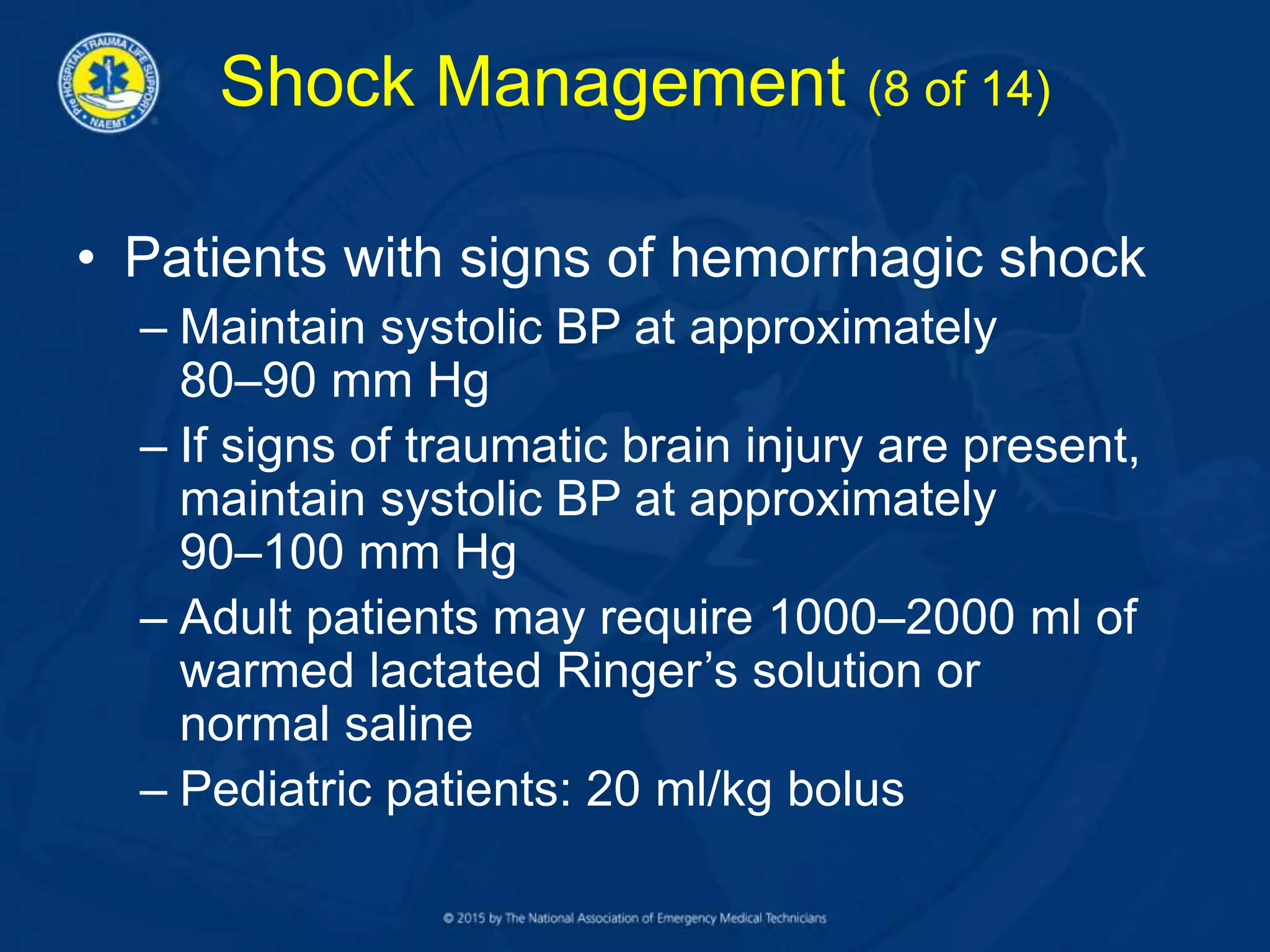
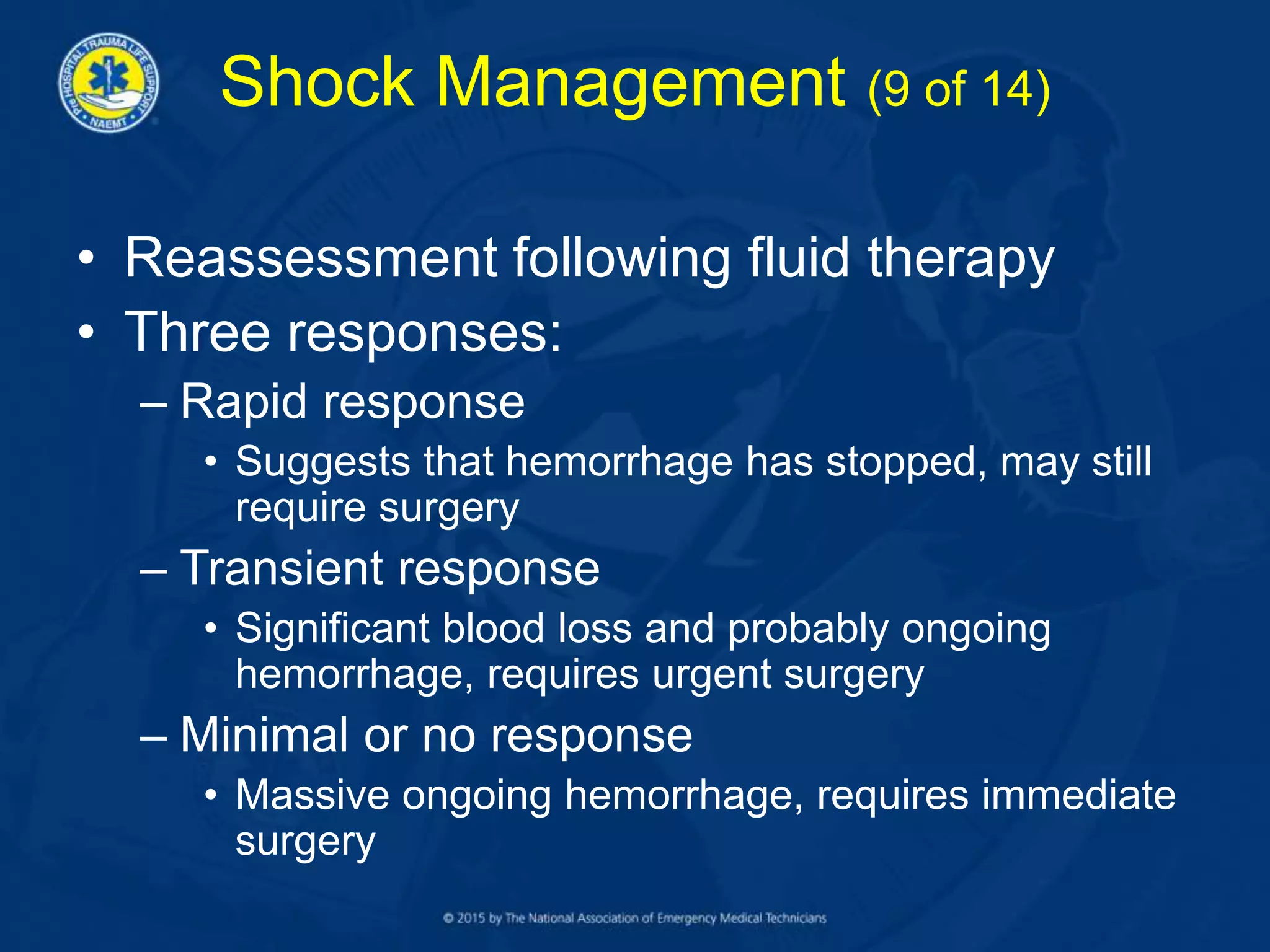
Circulatory shock results from inadequate cellular oxygenation and energy production to meet metabolic needs. The most common cause is hemorrhage from blood or fluid loss. Proper shock management focuses on controlling hemorrhage, restoring adequate circulation and oxygen delivery to tissues, and rapidly transporting patients for definitive care. External hemorrhage is controlled with direct pressure, tourniquets, or hemostatic dressings while internal bleeding requires surgical intervention. Fluid resuscitation balances restoring perfusion with preventing further bleeding. Uncontrolled, shock leads to organ damage and death, so prompt prehospital care can help restore oxygenation and improve outcomes.