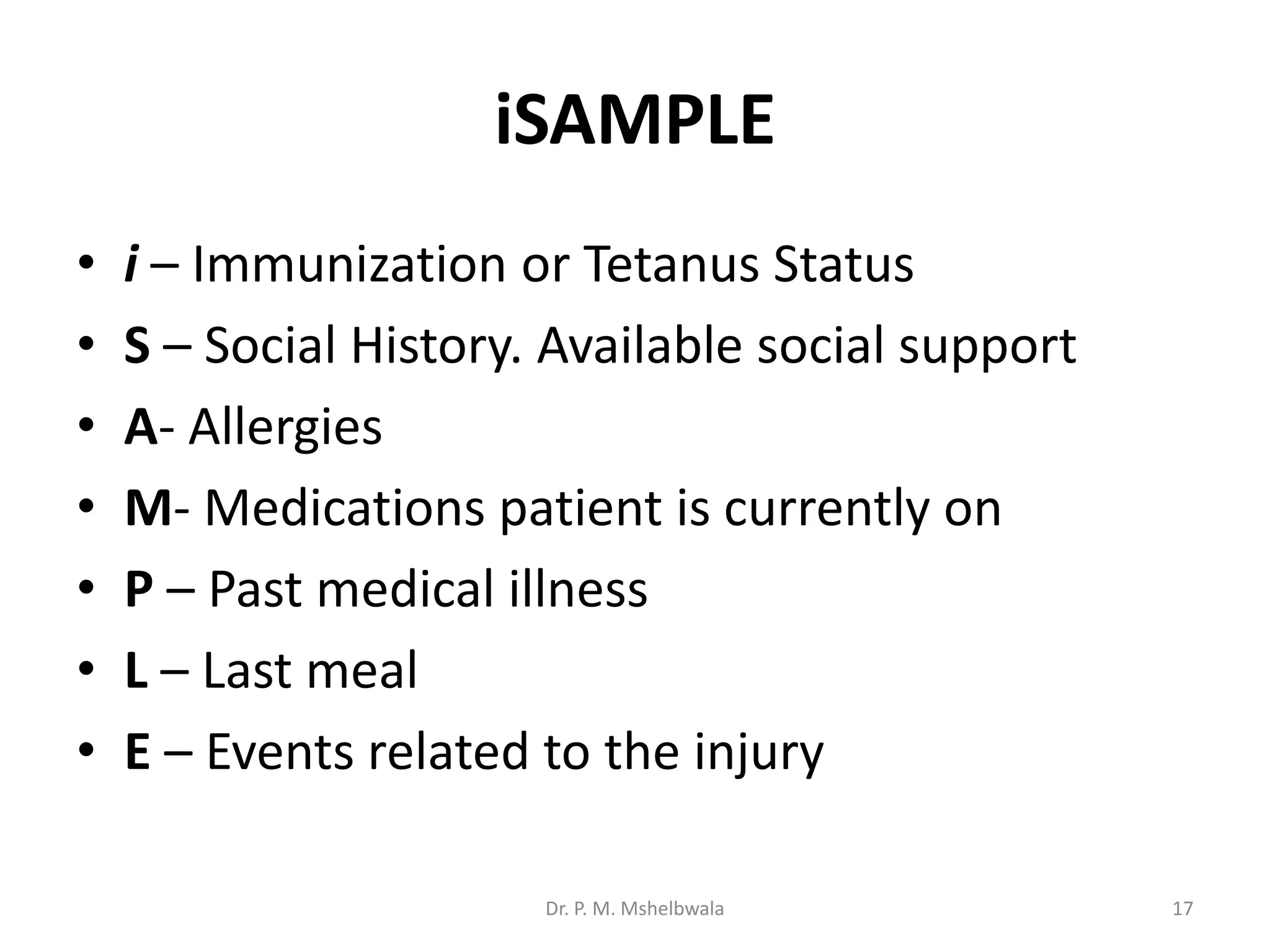
Trauma is a significant global health issue, being the third leading cause of death, and requires a systematic approach for effective assessment, triage, and resuscitation. The document outlines the triage process, primary and secondary surveys, and critical aspects of trauma management including airway, breathing, circulation, and disability assessments. Timely intervention and preventive measures are emphasized as essential for improving trauma outcomes.