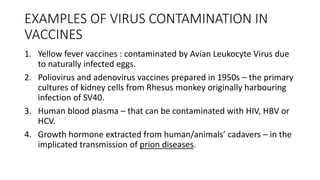
The document discusses validation studies for virus inactivation and removal in biotechnology products. It describes the aims of validation guidelines to provide guidance on designing validation studies, including selecting viruses and interpreting results to define effective process steps for inactivating and removing viruses. Validation is important for products derived from cell lines, blood, tissues or other biological sources to prevent viral transmission. Common virus inactivation methods discussed include solvent/detergent treatment, pasteurization, low pH treatment, and UV irradiation. Critical production parameters influencing effectiveness must be thoroughly investigated.