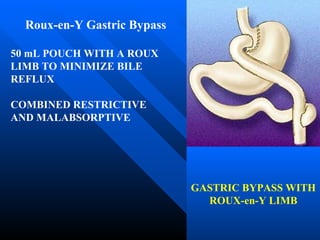
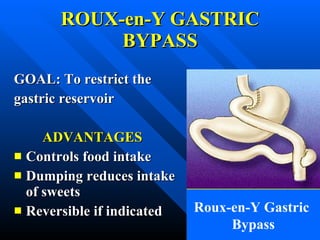
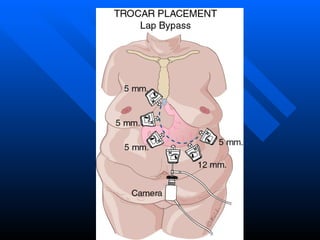
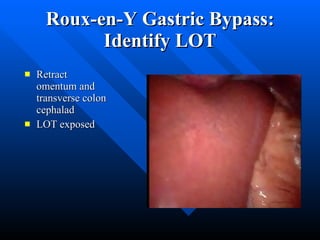
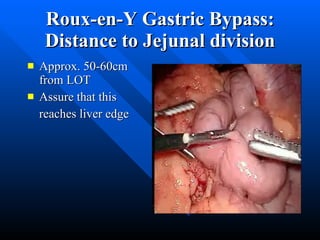
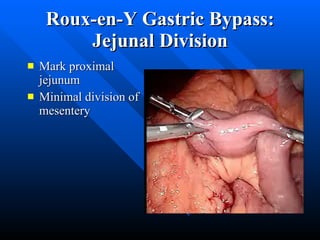
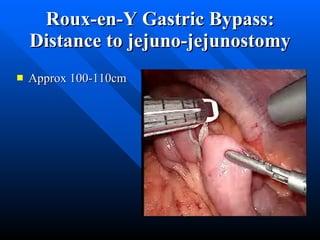
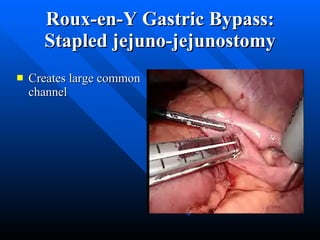
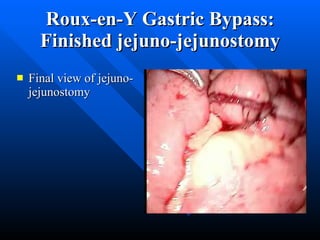
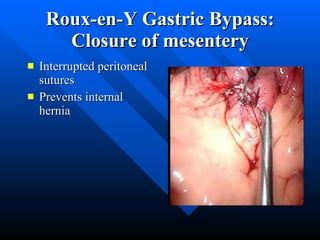
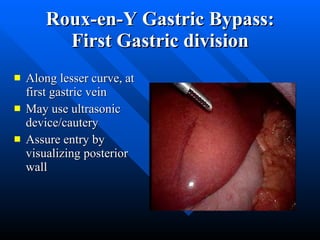
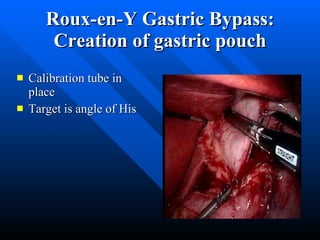
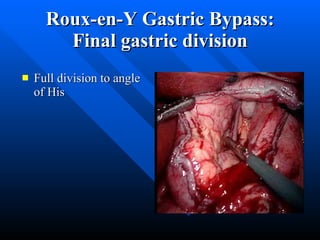
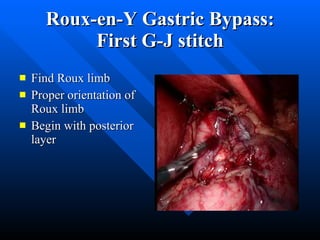
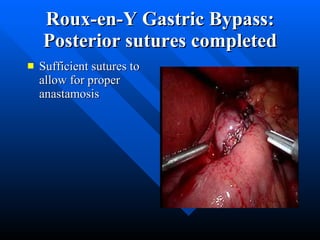
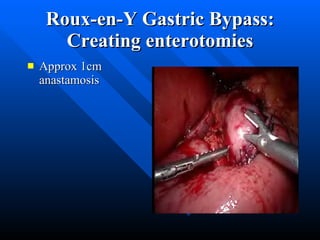
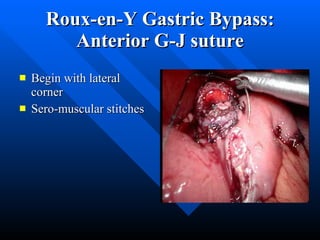
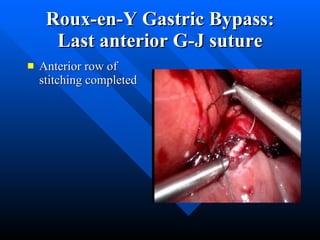
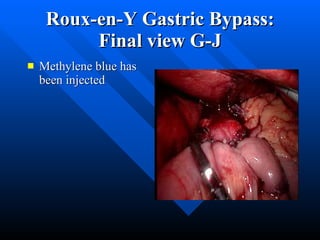
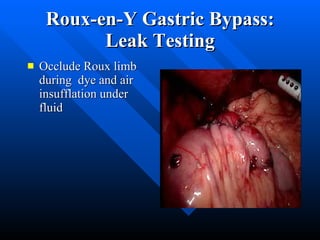
The document describes the technique for performing a laparoscopic Roux-en-Y gastric bypass surgery. It details the steps of the procedure including identifying the ligament of Treitz, measuring and dividing the jejunum to create the Roux limb and biliopancreatic limb, performing a jejunojejunostomy, creating the gastric pouch, and completing an antecolic antegastric gastrojejunostomy. The summary emphasizes key points such as proper identification of anatomical landmarks, appropriate measurement of limb lengths, use of hand sewing for anastomoses, and performing a leak test.