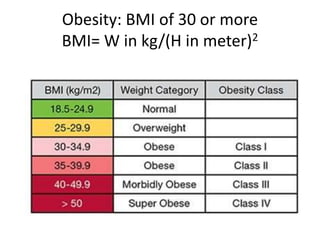
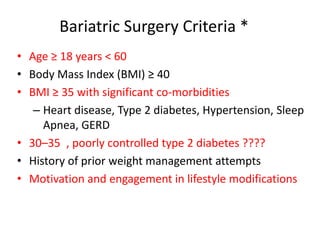
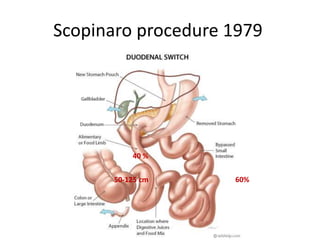
1) Bariatric surgery is recommended for patients with a BMI over 40, or over 35 with significant comorbidities. It includes both restrictive procedures that reduce stomach size and malabsorptive procedures that alter digestion.
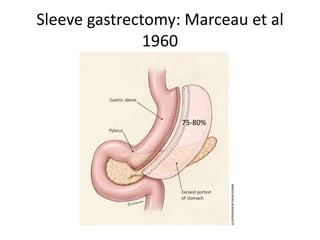
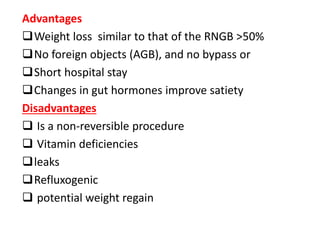
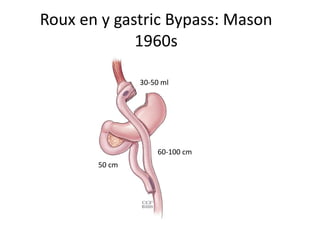
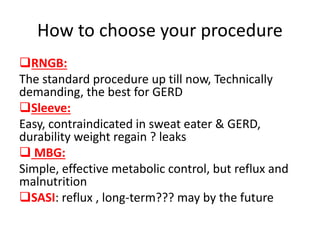
2) The Roux-en-Y gastric bypass is the most commonly performed procedure, resulting in 60-80% excess weight loss. However, it is technically complex with greater risks. Sleeve gastrectomies have increased in popularity as they are less complex but still effective.
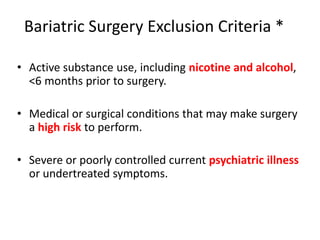
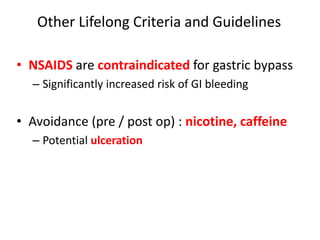
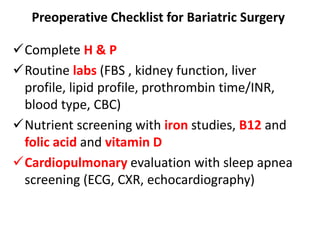
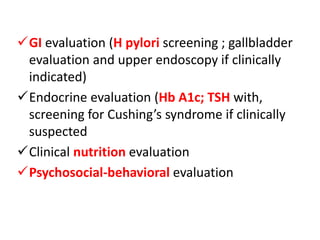
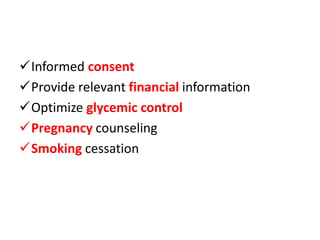
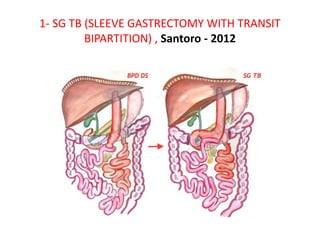
3) Careful patient selection and lifelong nutritional supplementation and monitoring are important for success and safety. Outcomes have greatly improved with experience and new procedures continue to be developed and refined.