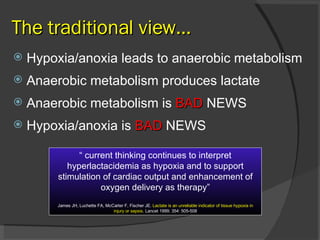
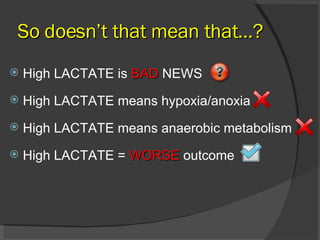
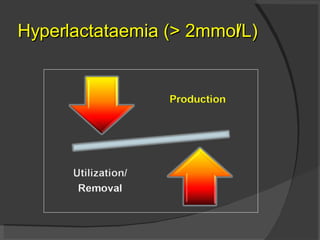
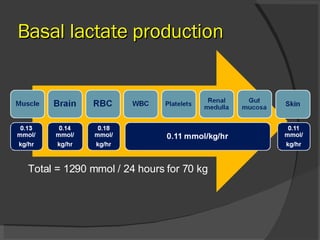
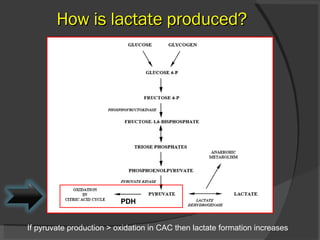
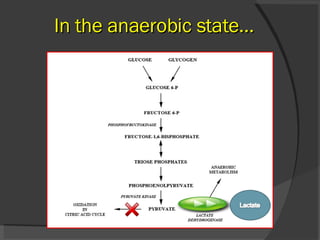
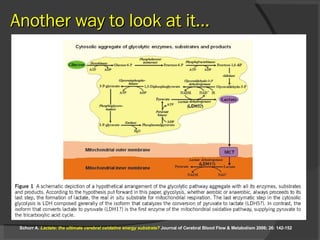
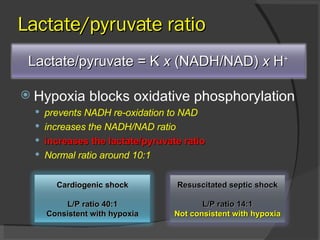
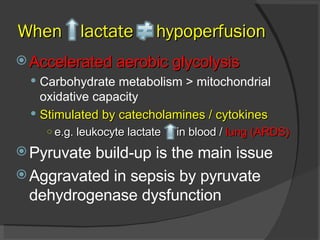
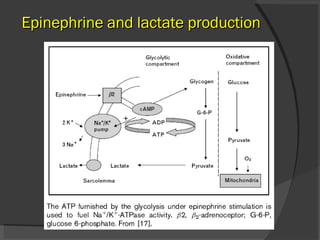
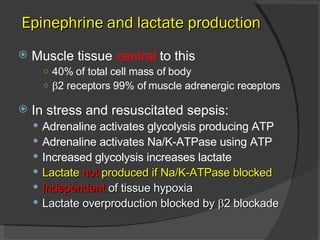
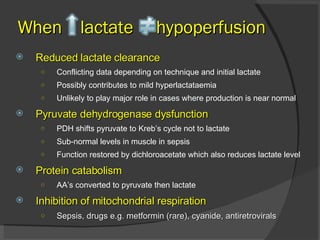
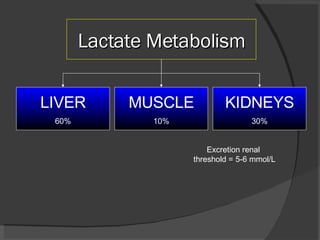
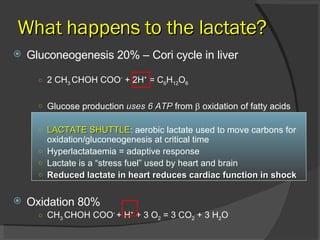
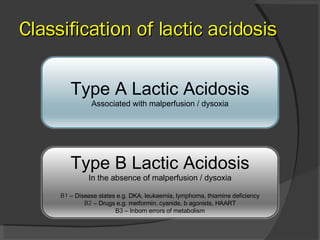
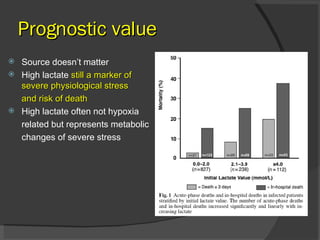
The document discusses lactate production and metabolism. It challenges the traditional view that high lactate levels always indicate tissue hypoxia or anaerobic metabolism. Lactate can be produced through many mechanisms including accelerated aerobic glycolysis stimulated by factors like catecholamines. The liver, kidneys, and muscle all play roles in lactate metabolism, with the majority being used for gluconeogenesis or oxidation rather than indicating hypoxia. High lactate is a marker of physiological stress but the source does not necessarily mean malperfusion, and treatment should focus on the underlying condition rather than just the lactate level alone.