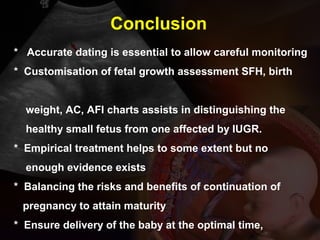
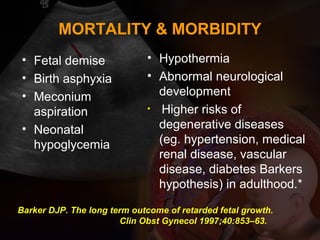
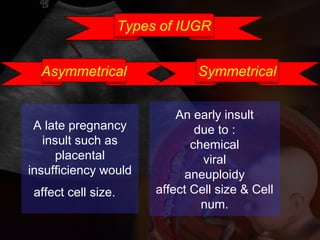
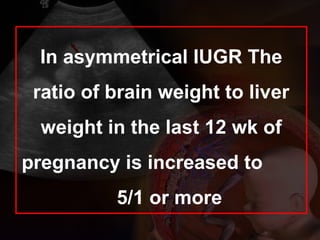
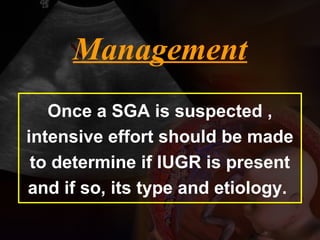
This document discusses intrauterine growth restriction (IUGR), including definitions, causes, detection methods, and management. Key points include:
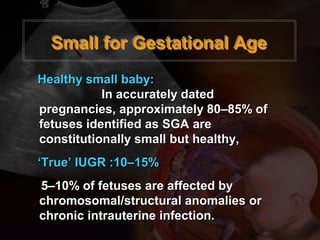
- IUGR, or small for gestational age (SGA), affects 10-15% of fetuses and is caused by placental insufficiency restricting nutrients/oxygen to the fetus.
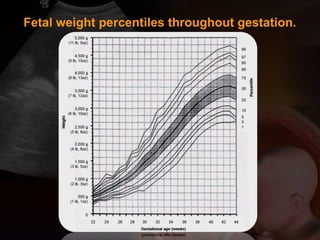
- Ultrasound is used to monitor fetal growth parameters like abdominal circumference and estimated fetal weight against customized charts. Doppler ultrasound of umbilical and uterine arteries can also indicate placental insufficiency.
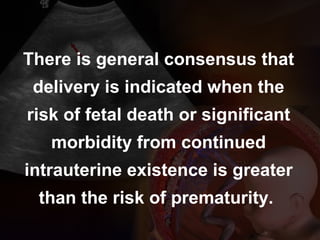
- If IUGR is detected, careful surveillance is required using biophysical profile, amniotic fluid volume, and Doppler ultrasound to determine optimal delivery timing weighing fetal vs. maternal


![6 to 10 times greater than AGA.
120 per 1,000 for all cases of IUGR
80 per 1,000 [after excluding congenital
malformations]
53 percent of preterm stillbirths are IUGR
26 percent of term stillbirths are growth
restricted.
* AGA - appropriate for gestational age
Perinatal Mortality in IUGR:](https://image.slidesharecdn.com/iugrvld-150404080422-conversion-gate01/85/Iugr-vld-5-320.jpg)
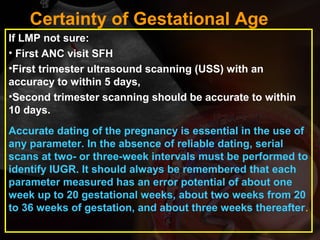
![Detection of IUGR:
Clinical methods:
• Abdominal palpation,
• Weekly measurement of symphyseal fundal
height[SFH]
• Abdominal girth.
There is enough evidence that SFH measurement
performs better if the charts used to plot SFH are
customised to match particular variables affecting
fetal growth in fetuses of different mothers](https://image.slidesharecdn.com/iugrvld-150404080422-conversion-gate01/85/Iugr-vld-10-320.jpg)
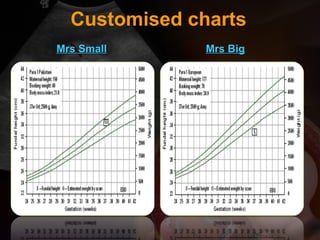
![Role of Ultrasound:
USG biometric parameters:
• Abdominal
circumference[AC]
• estimated fetal
weight[EFW],
• Femoral length[FL],
• head circumference[HC],
• Biparietal diameter[BPD]
USG Prognostic parameters:
•Growth velocity,
•Amniotic fluid volume[AFV],
•Uterine artery Doppler,
•Cerebral artery Doppler
•umbilical artery Doppler,
•Umbilical venous Doppler,
• biophysical profile.
The growth velocity is the most sensitive indicator of fetal growth.
for symmetric and asymmetric IUGR AC is a good indicator
[sensitivity of > 95% when AC is <2.5th percentile]
Customiosed charts are available for most parameters](https://image.slidesharecdn.com/iugrvld-150404080422-conversion-gate01/85/Iugr-vld-12-320.jpg)
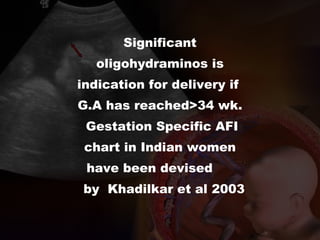
![• Umbilical artery Doppler[UAD]: primary surveillance tool.
When an anomaly scan and umbilical artery Doppler are
normal, the small fetus is likely to be a ‘normal small fetus’
• Amniotic fluid volume[AFI] measurement: Reference range
for AFI has been devised for Indian subset of population.*
• Biophysical Profile[BPP] There is evidence from uncontrolled
observational studies that biophysical profile in high-risk
women has good negative predictive value, fetal death is
rare in women with a normal biophysical profile
• Use of cardiotocography [CTG] antepartum to assess fetal
condition is not associated with better perinatal outcome;
however daily NST is practiced in many centers with its own
efficiency.
Monitoring IUGR pregnancy
*Khadilkar SS, Desai SS, Tayade SM, Purandare CN. Amniotic fluid index in normal pregnancy:
an assessment of gestation specific reference values among Indian women.J Obstet Gynaecol
Res. 2003 Jun;29(3):136-41](https://image.slidesharecdn.com/iugrvld-150404080422-conversion-gate01/85/Iugr-vld-13-320.jpg)
![Gestation specific reference range for AFI values in normal
pregnancy amongst Indian women :
Khadilkar SS,Desai SS, Tayade SM,PurandareCN
J.Obstet.Gynaecol Res vol29,no.3:136-141,June 2003
Gestation specific percentile
values of AFI in Indian Women
Weeks of
Gestation
5th
50th
95th
Number of cases
16--19 80 130 180 19
20 84 132 184 15
21 87 139 194 10
22 88 142 196 12
23 88 145 198 12
24 90 147 200 16
25 92 157 212 20
26 93 158 214 30
27 93 169 219 20
28 92 162 224 22
29 88 150 221 19
30 84 148 218 24
31 83 146 213 32
32 83 144 199 45
33 80 140 195 33
34 76 142 190 28
35 74 138 185 23
36 72 135 183 14
37 70 128 182 36
38 68 122 176 20
39 61 115 168 24
40 59 113 166 24
41--42 54 111 152 19
Total
n= 517
[gestation specific
values< than 5th
percentile:
oligohydramnios and
> 95th
percentile:
polyhydramnios ]](https://image.slidesharecdn.com/iugrvld-150404080422-conversion-gate01/85/Iugr-vld-17-320.jpg)


![Delivery room:
It should be equipped with Intrapartum monitoring with continuous
cardiotocography
ppropriate neonatal staff and facilities to care for the IUGR affected
newborn [NICU].
The mode of delivery
It is based on the gestation, fetal condition, and cervical status
In cases where there is evidence of fetal academia, caesarean section may
be appropriate.
The Growth Restriction Intervention Trial (GRIT)* concluded that, in
general, at gestations less than 31 weeks, delivery is best delayed. The
GRIT has not provided evidence to date that ‘early delivery to pre-empt
severe hypoxia and acidosis reduces any adverse outcome’.
Resnik R. Fetal growth restriction: Management. 2005 UpToDate. Available at: www.uptodate.com
Delivery :](https://image.slidesharecdn.com/iugrvld-150404080422-conversion-gate01/85/Iugr-vld-28-320.jpg)